Radiologic Imaging Considerations
Jeffrey A. Bennett
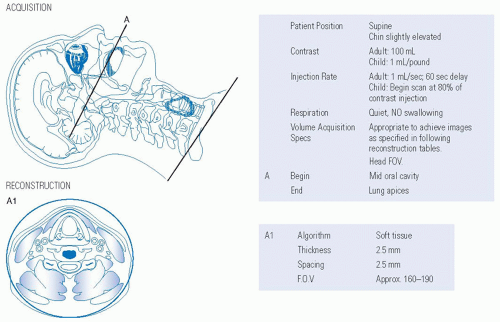
Imaging of the neck is performed in addition to the physical exam, both as part of the initial staging of head and neck cancer and in posttreatment surveillance. It is helpful for confirmation of a clinical NO neck, to assess nonpalpable areas of the neck such as the retropharyngeal region, and to evaluate the extent of palpable adenopathy. Prognostic information can be gained from the size of a nodal mass and the presence of extracapsular spread of tumor beyond the lymph node capsule, with associated possible invasion of muscles and vessels. Contrast-enhanced CT and contrast-enhanced MRI are the primary tools used to assess for the presence of tumor metastases in cervical lymph nodes. Ultrasound is used mostly for image-guided biopsy of a suspicious node. Suggested CT and MRI protocols are given in Figures 14-7 and 14-8.
FDG-PET can also be used to show physiological activity in lymph nodes, but its role in initial staging of head and neck cancer is still to be determined. Several studies have investigated the value of PET scanning for lymph node status in initial staging,1,2,3,4,5,6 with a range of sensitivity from 47% to 100% and a range of specificity from 87% to 100%. Its negative predictive value is approximately 90%.7 Its main limitation is the detection of small, <7 mm positive nodes which is a problem given that >40% of metastatic lymph nodes are < 7 mm in diameter.8 Recent PET research has looked at standard uptake values (SUV) in positive lymph nodes as a prognostic factor, with one study9 showing a higher SUV in nodes with extracapsular extension versus nodes without extracapsular extension, 11.0 versus 5.0. Higher SUV values in nodes were also shown to be predictive of distant failure at 1-year follow-up.
CT has been shown to be slightly superior to MR for the detection of metastatic deposits in lymph nodes.8 Both CT and MRI require intravenous contrast for lymph node detection. Slice thickness should be no < 3 mm for CT and 4 mm for MRI. Multiplanar reformation of thin-section CT data can be helpful for problem solving, for example in showing a preserved fatty hilum in a folded lymph node. Criteria for calling a node positive include size, shape, enhancement pattern, and evaluation of the lymph node capsule.10 Size, traditionally measured as the greatest diameter in the axial plane, is one feature looked at and is certainly helpful in assessing the typically uniformly enhancing lymph nodes seen in lymphoma. The availability of multiplanar reformats in CT and imaging in multiple planes with MRI allows
a better visualization of the entire lymph node. Studies have not been performed to assess the sensitivity and specificity for metastatic head and neck cancer using the greatest diameter of a lymph node in any plane or the lymph node volume, which can be obtained easily with currently available software. Shape can be helpful, as lymph nodes filled with tumor tend to become more spherical. The enhancement pattern is probably the most useful feature. Nodes positive for squamous cell cancer have internal filling defects (Figs. 14-9 and 14-10), even when they are very small.
a better visualization of the entire lymph node. Studies have not been performed to assess the sensitivity and specificity for metastatic head and neck cancer using the greatest diameter of a lymph node in any plane or the lymph node volume, which can be obtained easily with currently available software. Shape can be helpful, as lymph nodes filled with tumor tend to become more spherical. The enhancement pattern is probably the most useful feature. Nodes positive for squamous cell cancer have internal filling defects (Figs. 14-9 and 14-10), even when they are very small.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree