RADIATION TECHNIQUES
GOALS OF RADIATION THERAPY AND CONVENTIONAL EXTERNAL BEAM TECHNIQUES
The primary goal of irradiation of tumors in the pituitary-hypo-thalamic region is delivery of the prescribed tumor dose with minimal exposure to critical normal surrounding structures, particularly the visual and auditory systems, brainstem, and temporal lobes, and to excessively large volumes of hypothalamus. The modern radiotherapeutic process is based on precise delineation of the target and critical structures, which is achieved using contrast-enhanced, thinslice CT scanning. Further improvements in tumor localization are possible by correlation of CT and MRI data.73
The newer localization techniques can correct for the geometric distortion of MRI data sets and provide three-dimensional CT and magnetic resonance images and target volume correlation. Most patients with neuroendocrine tumors undergo the treatment planning process and the actual radiation treatments
with a head immobilization device. The author’s practice is to use a thermoplastic material that is molded to the patient’s face and immobilized to a baseplate. The reproducibility of this device is within 2 to 3 mm on a daily basis during a conventional 5- to 6-week course of radiotherapy.
with a head immobilization device. The author’s practice is to use a thermoplastic material that is molded to the patient’s face and immobilized to a baseplate. The reproducibility of this device is within 2 to 3 mm on a daily basis during a conventional 5- to 6-week course of radiotherapy.
The treatment planning process itself is typically carried out at a workstation with three-dimensional capability. The objective of the treatment planning process is to evaluate the relative dose distribution to the tumor and surrounding normal tissues of a variety of field arrangements. The optimal plan is selected and is further refined by beam modulation with devices such as beamattenuating wedges, compensators, or customized blocks. The use of two opposed lateral fields with low-energy photons is not recommended because of a slightly higher risk of temporal lobe radionecrosis. Satisfactory dose distribution generally is achieved with a three-field technique that uses two opposed lateral beams and a vertex or coronal field directed downward from the scalp to the pituitary fossa. This technique is less suitable for small tumors with minimal suprasellar extension, because the vertex field traverses a considerable amount of normal brain.
Other acceptable techniques include a four-field arrangement, which typically requires wedges in at least two fields, and the use of an arc technique. The bicoronal 110-degree arc technique with a reversing wedge filter moving in each beam is commonly used. With this setup, the linear accelerator rotates from the level of the ears superiorly to the midline, creating a 110-degree coronal arc. A similar arc is then created on the contralateral side. Although these arc fields can exhibit substantial nonuniformity of dose distribution because of the curvature of the skull, this can be corrected by using wedge filters in the field.
Similarly, an axialoblique bilateral arc arrangement with wedges can be used if the patient’s head can be flexed sufficiently to exclude the eyes from the treatment field. The author’s standard practice is to generate multiple plans for each patient, evaluate the isodose distributions, and select the most appropriate treatment technique. With such refined treatment planning, the dose gradient within the tumor is typically <5%, and the dose falloff to surrounding critical structures is very sharp. An example of such an isodose distribution is presented in Figure 22-2, which illustrates an axialoblique arc pair with 15-degree wedges.
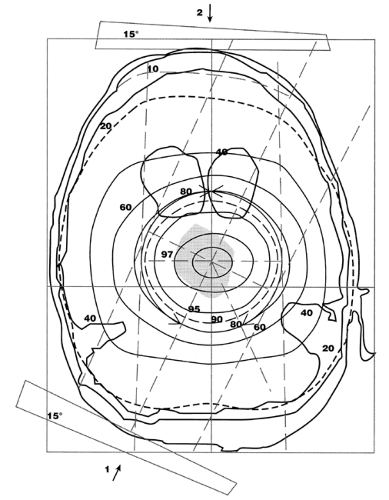 FIGURE 22-2. Isodose distribution using the arc technique (first setting) reveals a sharp dose falloff from the center of the target. |
The advent of three-dimensional treatment planning has introduced a new level of sophistication into the simulation process. Using 3-D techniques, three standard 2-D techniques (opposed-lateral two-field setup, 110-degree bilateral arcs, and a three-field technique) were compared with a single 330-degree rotational arc method (avoiding the eyes) and a four-field noncoplanar arc technique in an attempt to identify the optimal technique for minimizing exposure of normal tissues surrounding the pituitary.74 These observations have significant practice implications. The two-field opposed-lateral technique using 6 MV photons resulted in the highest dose to the temporal lobes and, therefore, should not be used routinely. The dose to the temporal lobes could easily be reduced with this technique, simply by using a higher energy beam, such as 18 MV. The three-field technique was superior to the opposed-lateral technique in reducing temporal lobe dose. Both the bilateral arc and single 330-degree rotation technique further decreased temporal lobe dose, in comparison with the fixed two- and three-field techniques. The four-field noncoplanar arc technique yielded the lowest temporal lobe dose but also resulted in the highest lens dose.
After the treatment planning process, the exact field setup is determined during a simulation session. The patient is repositioned in the same configuration as used for the treatment-planning CT or MRI studies, and the central intersection point of the radiation fields, or isocenter, is determined using a coordinate transform system from the planning CT. The isocenter is verified with orthogonal radiographs. External reference land marks—specific points that had been selected at the time of the treatment-planning CT and that were visualized with barium strips or palates—are revisualized on the orthogonal films using radiopaque markers. These serve as external fiducial coordinate reference points that allow the transformation of CT location to orthogonal films. Because the thermoplastic mask provides rigid and reproducible immobilization, there is no need for skin marks; all necessary marks are placed directly on the mask. Daily alignment of the patient at the treatment machine is carried out using reference marks on the mask and a three-point laser system. At the first treatment session, verification portal images are obtained; in routine cases, weekly portal images are obtained. More complex setups using noncoplanar fields incorporate a portal verification imaging system.
The author uses a total dose of 45 Gy in 1.8-Gy fractions for patients with pituitary adenoma. This dose is delivered in five fractions per week over a 5-week period. Although a clear dose-response relationship has not been established, most reports suggest that 40 to 45 Gy in 1.8- to 2.25-Gy fraction sizes produces high local control rates for most pituitary microadenomas.75 For craniopharyngioma and meningioma, the total dose is increased to 54 Gy. For low-grade glioma, the total dose is a function of the exact histologic type, the extent of residual disease, and the proximity of critical neural structures to the treatment field.
INNOVATIVE RADIATION TECHNIQUES
PARTICLE BEAM IRRADIATION OF THE PITUITARY GLAND
In the early 1950s, studies were performed with stereotactic-charged particles in patients with metastatic breast carcinoma to produce pituitary hormone suppression. Since then, more
than 3500 patients have been treated worldwide to reduce primary pituitary tumors and to suppress pituitary function for the management of diabetic retinopathy, breast cancer, prostate cancer, and other conditions. Most of this experience was accrued at four institutions: the University of California at Berkeley, Massachusetts General Hospital, the Institute for Theoretical and Experimental Physics in Moscow, and the Institute of Nuclear Physics in St. Petersburg. The results in the management of more than 2000 patients with pituitary tumors have been excellent and are summarized in the following sections.
than 3500 patients have been treated worldwide to reduce primary pituitary tumors and to suppress pituitary function for the management of diabetic retinopathy, breast cancer, prostate cancer, and other conditions. Most of this experience was accrued at four institutions: the University of California at Berkeley, Massachusetts General Hospital, the Institute for Theoretical and Experimental Physics in Moscow, and the Institute of Nuclear Physics in St. Petersburg. The results in the management of more than 2000 patients with pituitary tumors have been excellent and are summarized in the following sections.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





