10.1 Introduction
Undernutrition can be found in every society, in every corner of the world. This chapter discusses the public health aspects of undernutrition in free-living people in the community. Children are at greatest risk for undernutrition, but it is important to realize that undernutrition can also be a problem in adults, especially the elderly. As manifest in developing countries, undernutrition can be endemic, affecting up to half of the population. Undernutrition, however, is not unknown in industrialized, developed and affluent countries, occurring in diverse niches of the society for the same and distinct reasons for which it is a concern in the developing world. Undernutrition caused by clinical illnesses or associated with hospitalized patients is beyond the scope of this chapter.
10.2 Definitions of undernutrition
Who is undernourished and the cause of the undernutrition depend on how one defines the term. In its essence, it can be seen as an undernourishing process in which the normal needs for one or several nutrients are not being met, or the nutrients are being lost at a greater rate than they are being acquired. When one envisions the problem in a dynamic sense, that is, as one of accumulating a deficit, then the absolute degree of imbalance is immaterial. Diagnosis becomes problematic, however, because it requires serial monitoring of the individual to detect the negative nutrient balance.
However, undernutrition in a public health context is usually assessed using static, anthropometric criteria or data related to the amount of macronutrients in the diet: protein and energy. Definitions of different types of undernutrition are summarized in Table 10.1. Underweight is the situation of having a less than adequate weight-for-age, derived from an international reference curve based on the growth of a homogeneous group of Caucasian children in southern Ohio in the USA, but generalized by United Nations agencies to a universal growth standard. Having a weight-for-age more than 2 standard deviations (SD) below the median of this reference curve is the criterion for a diagnosis of underweight. Wasting is a deficit of greater than 2 SD to the inferior side of the median of normal weight-for-height based on the aforementioned sample of children adopted for international reference. Wasting signifies acute protein–energy malnutrition (PEM). Stunting is extreme short stature, exceeding a deficit of 2 SD below the median of the international reference population’s length or height. It has been interpreted as a state of chronic malnutrition.
Table 10.1 Definition of different types of undernutrition
| Underweight | Weight-for-age <2 SD below the international standard |
| Marasmus | Weight-for-age <60% of the international standard |
| Kwashiorkor | The presence of oedema and weight-for-age <80% of the international standard |
| Marasmic kwashiorkor | The presence of oedema and weight-for-age <60% of the international standard |
| Wasting | Weight-for-height <2 SD below the international standard |
| Stunting | Height-for age <2 SD below the international standard |
| Chronic energy deficiency | Body mass index [weight (kg)/height (m)2] <18.5 |
International statistics about rates of undernutrition almost invariably refer to the fraction of children below the appropriate reference weight for their chronological age. However, if they are also of short stature, it is not appropriate on an individual basis for them to carry as much weight. The preferred diagnostic standard would be weight-for-height. Weight-for-age predominates because weight, but not height, is routinely collected and recorded in the health posts around the world from which the prevalence statistics are generated. Past malnutrition (rather than “chronic”) might be a more legitimate designation, if a child’s height velocity were within normal parameters at whatever his or her age. Whether nutrient availability alone, or in combination with hormonal aberrations resulting from stress, inflammation and infection, is the major determinant of poor longitudinal growth, is not yet understood. Understanding this is important in knowing how to interpret the significance of short stature worldwide.
Anthropometric criteria are used to define undernourished states in all age groups. A commission of the International Dietary Energy Consultative Group defined chronic energy deficiency based on the adult body mass index (BMI). Having a BMI of less than 18.5 kg/m2 is the diagnostic criterion for this condition. Chronic energy deficiency corresponds to a low weight-for-height, or wasting, rather than simply low weight-for-age. Groups of people with chronic energy deficiency in a community have lower work outputs, lower productivity and compromised ability to respond to physiologically stressful conditions. The robustness of chronic energy deficiency across ethnic and geographical variation has not been validated, as adult populations of the Indian subcontinent often have 30% of their individuals in the BMI category signifying chronic energy deficiency. The etiology of chronic energy deficiency may be starvation or chronic illness, such as tuberculosis. Chronic energy deficiency does not imply the presence or absence of edema or micronutrient deficiency.
Other biochemical and clinical measures of nutritional status, such as measuring serum albumin or recording food intakes, are not very useful from the public health perspective. They require more time and expense, involve more invasive measurement techniques, and are less accurate than anthropometry.
10.3 Clinical syndromes of undernutrition
There are two clinical syndromes of severe undernutrition (also known as protein–energy malnutrition, PEM): marasmus and kwashiorkor. Marasmus is characterized by extreme wasting; those suffering from marasmus appear to be just “skin and bones”. Marasmus is the physiological adaptation to marked restriction of dietary energy. There is marked reduction in fat and subcutaneous tissue, as well as atrophy of visceral tissues. Those suffering from marasmus limit their physical activity and have decreased rates of metabolism and protein turnover in an effort to conserve nutrients. Compared with healthy people, marasmic individuals are more susceptible to infection, and more likely to suffer death or disability from infection.
Kwashiorkor is the clinical constellation of edema and undernutrition. This is most commonly seen in children under 5 years of age and is usually associated with irritability, anorexia and ulceration of the skin. The irritability is a pathological mental status change, making the refeeding of these individuals a challenging task. The metabolic derangements are more severe in kwashiorkor, and the case fatality rate is higher than in marasmus. Kwashiorkor was first recognized in West Africa in the 1930s in children weaned from the breast and was thought of as a milk deficiency state. Subsequently, experts suggested that kwashiorkor was the result of dietary protein deficiency; however, evidence to support this hypothesis was lacking. More recent data suggest that it may result from depletion of antioxidants in association with dietary energy deficiency. The Well-come Trust Working Party in 1970 defined marasmus as a weight-for-age of less than 60% of the international standard, and kwashiorkor as the presence of edema and weight-for-age of less than 80% of the standard. When severe wasting and edema occur together the condition is called marasmic kwashiorkor, and the prognosis is worse than that of either marasmus or kwashiorkor. The clinical presentation of marasmic kwashiorkor is similar to that of kwashiorkor.
10.4 Micronutrient deficiency: “hidden hunger”
Although undernutrition is generally treated in textbooks in the domain of the deficits of macronutrients (energy, protein), the same factors that compromise macronutrient status also interfere with adequate nutrition with respect to minerals and vitamins. In 1990, the term “hidden hunger” was adopted to refer to micronutrient malnutrition due to substances so small that one could not see them. Endemic deficiencies of iron, iodine and vitamin A, which long headed the list of deficiency states worldwide, have been of principle concern and received major attention. Other micronutrients of growing public health concern are vitamin D, calcium, zinc, vitamin B12 and riboflavin. Where macronutrient intake is sufficient to meet energy needs, micronutrient deficiency may still exist as the food consumed is of a low nutrient density. An example of this would be a normal weight woman with iron deficiency on a dietary basis. The magnitude of micronutrient deficiency is thought to be huge, affecting 40% of the world’s population, with iron deficiency being the most prevalent, afflicting one-third of the world (see Chapter 13). Table 10.2 lists the principal micronutrients of concern in hidden hunger, the health consequences of deficiency states, the public health magnitude of the problem and examples successful interventions to alleviate the public health problem. Descriptions of public health programs that address hidden hunger are presented in Chapters 11–13.
Table 10.2 Micronutrient deficiencies, their consequences and successful strategies to combat them
In addition to dietary deficiency of vitamins and minerals, genetic constitution can be an important determinant of micronutrient deficiency. Lower dietary intakes of folate in the periconceptional period have been associated with congenital neural tube defects in Western nations. Additional dietary folate intake by mothers in the periconceptional period is associated with a lower incidence of these birth defects. This is the rationale for national supplementation programs where folate is added public foodstuffs, such as the Canadian policy of adding folate to wheat. These public health interventions have effectively reduced the incidence of neural tube defects. Genetic polymorphism, however, seems to play an important role in individual susceptibility. 5,10-Methylenetetrahydrofolate reductase is an enzyme that regenerates oxidized folate in the cell so that it can be used again during cell division. A ther-molabile genetic variant of this enzyme, which is less effective at regenerating folate, occurs in up to 15% of some Caucasian populations. This genetic variant may result in inadequate cellular proliferation when cell division occurs at an accelerated rate, such as in the developing fetus. The deleterious effect of this variant enzyme can be overcome with additional dietary folate, and this may well explain why folate supplementation reduces neural tube defects in Caucasian populations. Asian populations also seem to respond to enriched exposure to folic acid, with lower rates of congenital neural tube lesions. However, in native American and African ethnicities, the responsiveness of this teratogenic condition to folate status has yet to be determined. This example illustrates how gene–nutrient interactions can explain the basis of important public health interventions, and suggests that public health nutritionists and basic medical scientists can combine their knowledge to improve the health of people worldwide.
10.5 Time trends and contemporary prevalences
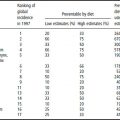
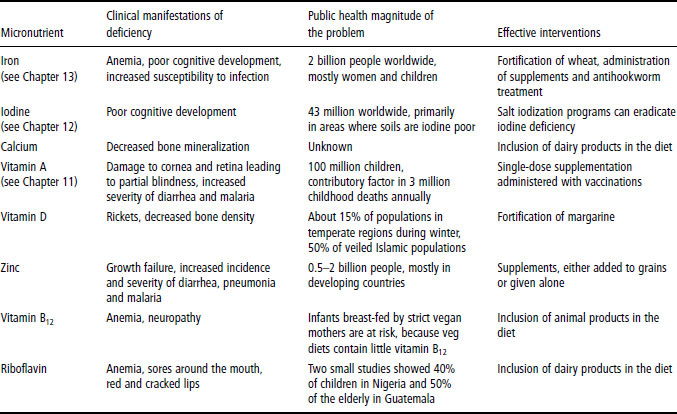
The prevalence of underweight, stunting and wasting, and the estimated dietary energy intake for different regions of world in 2000 and 1980 are shown in Table 10.3. The nation with the highest rates of all forms of anthropometric undernutrition is India. Sub-Saharan Africa is the region that has shown the least improvement since 1980. Figures 10.1–10.4 are maps depicting the geographical prevalence of underweight, stunting, wasting and dietary energy consumption in 2000.
10.6 Etiology: determinants and conditioning factors for undernutrition
Physiological mechanisms causing undernutrition
There are five possible mechanisms that result in nutrient deficiency, mechanisms that alone or in combination can reduce nutritional status:
- decreased nutrient intake, e.g. famine or the anorexia of chronic illnesses such as anorexia nervosa
- decreased nutrient absorption, e.g. generalized carbohydrate and amino acid malabsorption in cholera from rapid intestinal transit times or the malabsorption of sugars after diarrhea-induced lactase deficiency
- decreased nutrient utilization in the body, e.g. concomitant ingestion of antimalarial drugs which interfere with folate metabolism, and congenital enzyme deficiencies that partially block nutrient metabolic pathways, such as those in phenylketonuria
- increased nutrient losses (most commonly through the gastrointestinal tract, but also through the skin or urine), e.g. the protein-losing enteropathy of inflammatory bowel disease and the loss of nutrients through denuded, burned skin
- increased nutrient requirements (through pathophysiological states such as chronic inflammation), e.g. the increased metabolic rate with fever or hyperthyroidism.
Table 10.3 Prevalence of underweight, stunting and wasting in different regions of the world
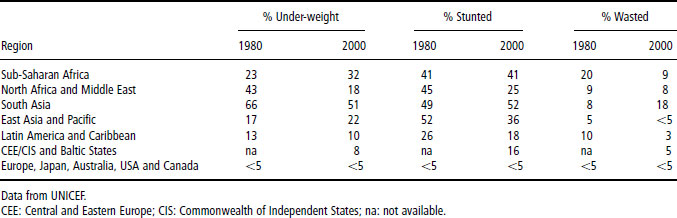
Figure 10.1 Dietary energy consumption in different regions of the world.
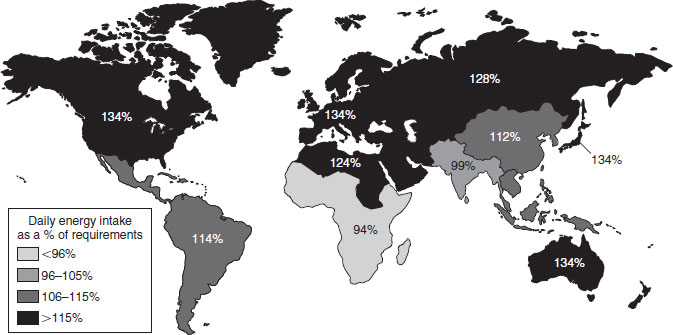
Figure 10.2 Prevalence of underweight in different regions of the world.
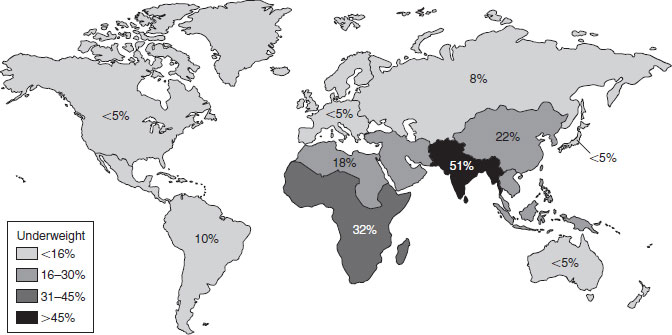
Figure 10.3 Prevalence of stunting in different regions of the world.
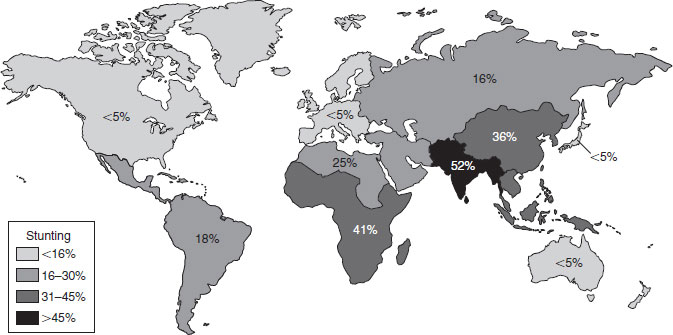
Figure 10.4 Prevalence of wasting in different regions of the world.

In a physiological sense, the five mechanisms explain how nutrient balance can become negative.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree