| Type of infection | Setting |
|---|---|
| Bacteremia | Neutropenia, pulmonary or urinary tract focus, burns |
| Pneumonia | Mechanical ventilation, neutropenia, chronic lung disease |
| Endocarditis | Injection drug use, prosthetic heart valve |
| Meningitis, brain abscess | Hematogenous or contiguous spread, neurosurgery, penetrating head trauma |
| Urinary tract infection | Bladder instrumentation |
| Osteomyelitis, septic arthritis (e.g., sternoclavicular joint) | Contiguous or hematogenous spread, injection drug use |
| Osteochondritis | Puncture wounds of the feet |
| Malignant external otitis | Diabetes, advanced age |
| Green nail syndrome | Water immersion, wet skin |
Epidemiology
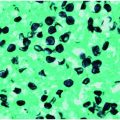
The epidemiology of P. aeruginosa infections reflects its predilection for moist environments. In hospitals, P. aeruginosa has been isolated from respiratory devices, disinfectants, distilled and tap water, and sinks. Pseudomonas aeruginosa can readily colonize the upper respiratory tract of mechanically ventilated patients, the gastrointestinal tract of patients receiving chemotherapy or broad-spectrum antibiotics, and the wounds of burn patients. Colonization usually precedes invasive infection.
Among healthcare-associated infections occurring in intensive care units, P. aeruginosa is the most commonly identified gram-negative pathogen, and the second most commonly identified organism overall. Emergence and spread of antimicrobial resistance, especially multidrug resistance (MDR), among P. aeruginosa is frequent. The National Nosocomial Infections Surveillance System 2003 report revealed that 29.5% of intensive care unit isolates are resistant to quinolones and 31.9% are resistant to third-generation cephalosporins. Furthermore, 21.1% of the isolates are resistant to imipenem, an agent once considered universally active against P. aeruginosa. The emergence and spread of MDR P. aeruginosa challenges the clinician when selecting appropriate antimicrobial therapy and underscores the importance of obtaining cultures with susceptibility testing in patients suspected to have bacterial infections. Knowledge of local antimicrobial resistance trends is essential to ensure optimal patient outcomes.
Diagnosis
The clinical features of P. aeruginosa infections are indistinguishable from those of other bacterial organisms, and a definitive diagnosis requires specimen cultures from the suspected site of infection (i.e., blood, sputum, urine) to identify the organism. Other clinically important gram-negative organisms that resemble P. aeruginosa come from the genera Stenotrophomonas, Burkholderia, and Ralstonia.
Antimicrobial therapy
Initial selection of an agent should be guided by the site of infection, the patient’s allergic history, and the institutional antibiogram. Early, aggressive antimicrobial therapy, with modification when susceptibility results become available, imparts a survival advantage and minimizes the emergence of antimicrobial resistance. Although several antipseudomonal antibiotics exist (Table 148.2), intrinsic or acquired resistance and bacterial persistence at sites of infection complicate management and eradication.
| Antimicrobial agent | Dosea/route /interval | Comment |
|---|---|---|
| β-Lactams | ||
| Ticarcillin–clavulanate | 3.1 g IV q4–6h | |
| Piperacillin | 3–4 g IV q4–6h | |
| Piperacillin–tazobactam | 4.5 g IV q6h 3.375 g IV q6h | Recommended pneumonia dose Recommended nonpneumonia dose |
| Ceftazidime | 2 g IV q8h | Preferred agent for CNS infections |
| Cefepime | 2 g IV q12h | |
| Meropenem | 1 g IV q8h | |
| Imipenem–cilastatin | 0.5 g IV q6h | |
| Aztreonam | 2 g IV q8h | Frequently reserved for penicillin-allergic patients |
| Quinolones | ||
| Ciprofloxacin | 400 mg IV q12h 500–750 mg PO q12h | Most active antipseudomonal quinolone in vivo |
| Levofloxacin | 750 mg IV/PO daily | |
| Aminoglycosidesb,c,d | ||
| Amikacin | 15 mg/kg IV once daily or 7.5 mg/kg IV q12h | |
| Gentamicin | 5 mg/kg IV once daily or 2 mg/kg loading dose, then 1.7 mg/kg IV q8h | |
| Tobramycin | 5 mg/kg IV once daily or 2 mg/kg loading dose, then 1.7 mg/kg IV q8h | |
| Polymyxins | ||
| Polymyxin E (colistin) | 1.5 mg/kg IV q8h | |
| Polymyxin B | 0.75–1.25 mg/kg IV q12h |
a Suggested dosing is for adult patients with normal renal and hepatic function.
b Aminoglycosides are not recommended for monotherapy against P. aeruginosa.
c Once-daily aminoglycoside dosing has been shown to be effective, less nephrotoxic, and less ototoxic, and is the preferred dosing method.
d Aminoglycoside levels and renal function should also be closely monitored during therapy.
Abbreviation: CNS = central nervous system.
β-lactam antibiotics active against P. aeruginosa include the extended-spectrum penicillins, some extended-spectrum cephalosporins, the carbapenems (except ertapenem), and the monobactam aztreonam. These agents form the basis for treatment of most Pseudomonas infections due to extensive clinical experience and patient tolerability. The high prevalence of reported penicillin allergy is the primary limitation.
The aminoglycosides tobramycin, amikacin, and gentamicin have excellent in vitro activity against P. aeruginosa. The concentration-dependent bactericidal activity and the postantibiotic effect of aminoglycosides provide the rationale for once-daily dosing. Aminoglycoside monotherapy should be avoided due to selection of resistant mutants and increased risk of clinical failure. Renal function and serum aminoglycoside levels should be monitored closely.
The quinolones have been frequently used for the treatment of P. aeruginosa and other bacteria. They possess excellent tissue penetration, good oral bioavailability, and a favorable safety profile. Ciprofloxacin and levofloxacin are the most active quinolones against P. aeruginosa, with ciprofloxacin considered the more active of the two. Increasing resistance to the quinolones, however, should temper reliance on their use as the basis for empiric therapy against P. aeruginosa, especially among hospitalized patients.
Use of polymyxin antibiotics has re-emerged due to MDR and pandrug-resistant gram-negative infections, including P. aeruginosa. The polymyxins possess activity against a variety of gram-negative organisms but have been limited in use due to their adverse effects, namely nephrotoxicity and neurotoxicity. Polymyxins are currently recommended only for isolates resistant to other antibiotics. Susceptibility testing should be performed as resistance to the polymyxins has been reported.
Much controversy exists over the use of combination therapy (“double-coverage”) for the treatment of infections due to P. aeruginosa. Data from a Cochrane review of sepsis comparing β-lactam and aminoglycoside combination therapy versus β-lactam monotherapy found no advantage to combination therapy for all-cause mortality (RR 1.01; 95% CI 0.75–1.35) or clinical failure (RR 1.11; 95% CI 0.95–1.29). Empiric combination therapy for most serious infections may still be warranted when considering local resistance data and to ensure appropriate treatment of other possible infecting organisms. The guiding principle for selecting combination therapy should be that each agent has a unique mechanism of action to avoid a possible antagonistic effect; β-lactam and aminoglycoside combination therapies are the most studied and continue to be primarily recommended.
Infections caused by P. aeruginosa
Respiratory infections
Pseudomonas aeruginosa
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree