Problems in the Staging of Lung Cancer
Philip T. Cagle
THE TNM STAGING SYSTEM
The stage, or anatomic extent, of a cancer at the time of diagnosis is one of the most important factors in predicting prognosis, selecting therapy, and stratifying patients for clinical trials and other research protocols.1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20 and 21 To be useful, a staging system must be as objective and reproducible as possible. There are multiple staging systems of which the tumor-node-metastasis (TNM) system is most commonly used, based on a combination of primary tumor size and local invasiveness (T), extent of nodal metastases (N), and presence or absence of distant metastases (M). The specific stage of a patient is derived from the combined TNM and patients in the same stage group are expected to have similar prognosis and be candidates for similar approaches to treatment. Generally, the higher the stage (or the T, N, or M individually), the worse the prognosis.1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18 and 19 This staging system is developed and maintained by the American Joint Committee on Cancer (AJCC) and the Union Internationale Contre le Cancer (UICC) and is periodically updated (the 7th edition went into effect in January 201017; see Chapter 25). Traditionally, TNM stage has been thus far the single most important factor in determining survival of lung cancer patients.19,20 and 21
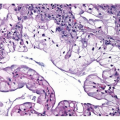
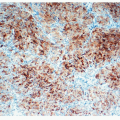
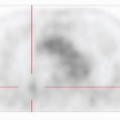
TNM staging may be either clinical or pathologic. Clinical staging, designated with the prefix “c,” is based on clinical and imaging findings prior to any treatment, including history and physical examination, computed tomography (CT) scan, positron emission tomography (PET) scan, integrated CT-PET, magnetic resonance imaging, as well as surgical staging procedures such as mediastinoscopy (see Chapters 18 and 19). Pathologic staging, designated with the prefix “p,” is based in most cases on gross and histologic examination of cancer resection specimens by the surgical pathologist. Obviously, the latter means that a treatment procedure, surgical resection, has occurred before staging is performed leading some critics to state that pathologic staging is at a disadvantage because clinical staging can be done prior to any treatment decision and used for those decisions. However, even after resection, vital information about prognosis and follow-up therapy can be gleaned from pathologic staging. On the other hand, the criteria for pathologic staging can be met without complete resection of a cancer if the highest T and N categories or the M1 category of the cancer can be histologically confirmed on biopsy or other specimens that do not involve complete resection of the primary cancer.17,18
The first TNM staging system for lung cancer was adopted in 1973 by the AJCC and in 1974 by the UICC. This first TNM staging system was proposed by Dr. Clifton Mountain and was based on a database of 2,155 patients from MD Anderson Cancer Center in Houston. The last revision of the lung cancer TNM staging system, prior to 2010, was in 1997 and was based on a database of 5,319 patients from MD Anderson Cancer Center. By 1997, standardization of the regional lymph node stations was established. Although these versions of the TNM staging system were generally valid, they were considered limited because the database is restricted to a single institution and the sample size is comparatively small, especially when broken down into subgroups. There was also some bias toward surgically treated patients.10,12,13
Although the TNM system has been widely used for non-small cell lung carcinomas, an alternative staging system has been widely used for small cell lung carcinoma, the Veterans Administration Lung Study Group System. In this system, patients are categorized into one of two stage groups: limited-stage disease or extensive-stage disease.10,12,13,19,20 and 21
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree