PREOPERATIVE PATIENT PREPARATION
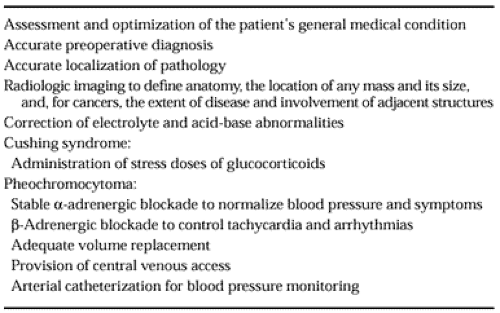
Several factors must be considered to appropriately prepare a patient for adrenalectomy to obtain a successful outcome (Table 89-2) The patient’s medical condition is carefully assessed and optimized to decrease operative risk. Patients with primary aldosteronism, for example, may have congestive heart failure, cardiac arrhythmias, or nephropathy. In addition, an accurate diagnosis is vital for appropriate surgical management. For pheochromocytoma, in particular, preoperative treatments and intraoperative monitoring are distinctly different from those used in other adrenal conditions.
Diagnostic biochemical tests and standard radiologic imaging may not definitively identify the cause of the endocrine disorder in some cases. Advances in imaging techniques and interventional radiologic procedures have greatly facilitated the diagnosis and localization of adrenal disorders. For example, for primary aldosteronism, adrenal vein sampling for aldosterone and cortisol is the definitive study if other radiologic imaging tests cannot differentiate an aldosteronoma from idiopathic adrenocortical hyperplasia as the cause. An aldosteronoma is effectively treated with adrenalectomy, while idiopathic adrenocortical hyperplasia is not improved after unilateral adrenalectomy and is managed medically.7 Similarly, petrosal sinus sampling has facilitated the differentiation of pituitary-dependent and pituitary-independent Cushing syndrome in difficult cases. If biochemical tests suggest a primary adrenal cause of Cushing syndrome, but CT fails to show a discrete unilateral adrenal mass, then iodine-131 (131I)–labeled methylnorcholesterol imaging may be useful to image primary pigmented micronodular adrenal hyperplasia.8 Bilateral adrenalectomy is curative for primary
pigmented micronodular adrenal hyperplasia and massive macronodular adrenal hyperplasia.1
pigmented micronodular adrenal hyperplasia and massive macronodular adrenal hyperplasia.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree