30 Pineal Region Tumors
Despite sharing a common anatomic location and often displaying similar imaging characteristics, pineal region tumors are extremely heterogeneous with respect to histopathology, natural history, and response to therapy. Moreover, due to their relatively uncommon nature (only 1.2% of all primary central nervous system [CNS] tumors),1 the study of their behavior and outcomes is compromised by limited clinical information. Historically, these tumors were considered unresectable, and the first strides in treatment were made with conventional radiotherapy, often pursued without a tissue diagnosis. At the time, this approach was justified because some previously untreatable pineal region tumors could be cured with radiotherapy.
Under current standards, conventional radiation is only appropriate for certain histologically verified malignant tumors. Approximately 30% of pineal tumors are benign and can be cured with gross total resection, which, in the contemporary microsurgery era, can be achieved with low rates of morbidity. Stereotactic radiosurgery is a potential alternative, particularly in patients with medical contraindications to open surgery.
Determining the most effective treatment strategies for malignant lesions is an ongoing process. The roles of all modalities, including surgery, radiation, radiosurgery, and chemotherapy, are being defined by outcomes from clinical trials and databases. As a result of these efforts, the prognoses of certain types of malignant tumors have already greatly improved. Advances in diagnosis and treatment of these rare and heterogeneous tumors are predicated on accurately establishing tumor cell type and grade. Although, in rare cases, a diagnosis can be made on the basis of circulating tumor-specific markers, the vast majority of pineal tumors can only be accurately diagnosed with ample tissue sampling.
 Historical Background
Historical Background
In the first half of the 20th century, small surgical series from some of the early giants in neurosurgery, including Cushing, Dandy, and van Wagnenen, illustrated the futility of safe pineal region surgery using the rudimentary surgical equipment of the time. In the words of Dandy, this experience was “disastrous … almost to indicate the futility of other efforts.”2 When radiotherapy was introduced in the middle of the 20th century, pineal region surgery had advanced little, and surgical approaches were still considered too dangerous, even for the limited goal of obtaining diagnostic tissue. Contemporary opinion was reflected through Poppen, a pioneer in surgical approaches to the pineal region, who, as recently as 1968, favored “X-ray therapy unless unusually critical conditions necessitate immediate surgical intervention.”3
Controversial Point
• Tissue diagnosis for a pineal region tumor can be made via a diagnostic biopsy or an open surgical approach. The decision should be made after a thorough discussion of the risks and benefits of each option between the physician and patient.
Radiotherapy without tissue diagnosis, along with shunting for hydrocephalus, became the standard of care. This strategy resulted in acceptable 5-year survival rates ranging from 58 to 70%, reflecting the prevalence and exquisite radio-sensitivity of germinomas and the overall slow growth rates of many tumors found in the pineal region.4–6
By the early 1970s, routine use of the operating microscope, the development of microneurosurgical techniques, advances in neuroanesthesia, and the advent of neurologic critical care as a subspecialty helped to usher in the modern era of neurosurgery, in which many operative goals that were considered too dangerous or impossible were now attainable.
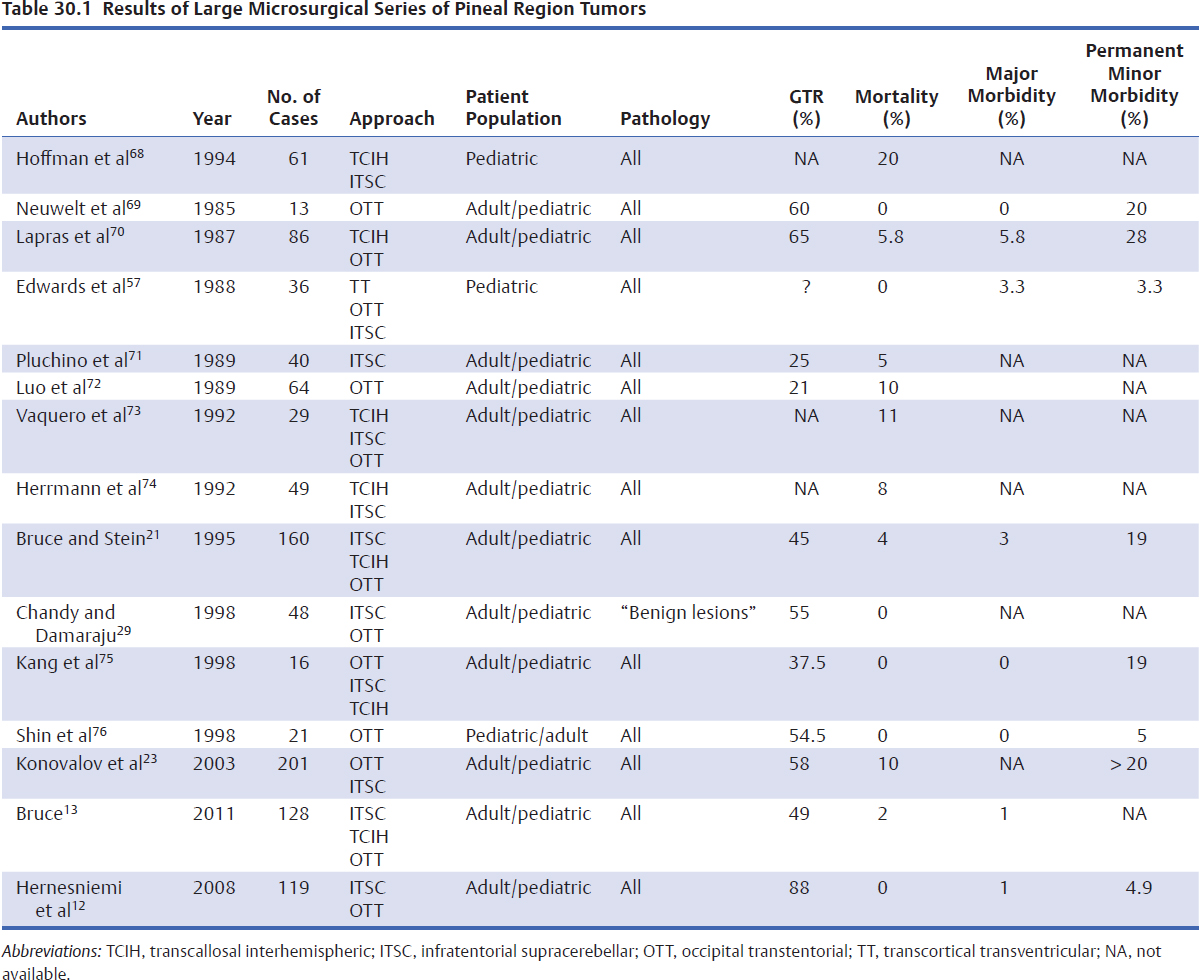
The demonstration of safe, effective pineal region surgery by Stein7 using the infratentorial supracerebellar approach adapted from Krause, and by Jamieson8 using the occipital transtentorial approach adapted from Poppen, required that the role of radical surgery be reexamined. Since these seminal papers were published in 1971, numerous surgical series have demonstrated safe effective surgical approaches to the pineal region over a large number of patients (Table 30.1). Similarly, the introduction and refinement of stereotaxy have improved the safety and efficacy of biopsies in the pineal region. Thus surgical management of pineal region tumors has advanced to the point where a tissue diagnosis to direct therapy is mandatory for patients with negative serum tumor markers, and open surgical resection is a viable tool whose relative merits depend on tumor histology.
 Clinical Presentation and Preoperative Evaluation
Clinical Presentation and Preoperative Evaluation
The vast majority of patients with pineal region tumors present with symptoms of obstructive hydrocephalus: headache, nausea/vomiting, lethargy, and midbrain compression resulting in Parinaud’s phenomena: impaired up-gaze, near-light dissociation, and convergence nystagmus.
Initial evaluation of a pineal region mass entails a directed medical history, a careful neurologic exam, serum assays for germ cell tumor markers, and a contrast-enhanced magnetic resonance imaging (MRI) study. Determination of the degree of hydrocephalus is critical to optimize immediate and subsequent management decisions. Elevated serum β-human chorionic gonadotrophin (β-hCG) is consistent with choriocarcinoma, although slight elevations can be found in germinomas with syncytiotrophoblastic elements. Elevated α-fetoprotein (AFP) is consistent with yolk sac and some embryonal carcinomas. Cerebrospinal fluid (CSF) is only marginally more sensitive for tumor markers than serum and, as such, carries little additional diagnostic potential. Whether detected in the serum or the CSF, positive germ markers are diagnostic for malignant germ cell tumors and obviate the need for a tissue diagnosis.
Pitfalls
• The standard workup for a pineal mass includes assays for germ cell markers. If they are present, radiation treatment can proceed without the need for a tissue diagnosis. Failure to order marker studies can result in an unindicated surgical procedure.
• Pineal cysts are simple cysts that are isointense to CSF and may show some rim enhancement on MRI. They should not be confused with pineal region tumors that are hyper-intense to CSF and more densely enhancing. Pineal cysts can be followed with serial imaging and rarely require treatment.
 Cerebrospinal Fluid Sampling and Diversion
Cerebrospinal Fluid Sampling and Diversion
Hydrocephalus, usually from obstruction of the sylvian aqueduct, can be treated with ventriculoperitoneal shunting or endoscopic third ventriculostomy. In rare cases of mild hydrocephalus, a CSF-diverting procedure can be deferred if an open tumor resection is planned that will likely relieve the obstruction. In general, third ventriculostomy is preferred because it achieves CSF diversion without exposing patients to shunt-related complications, such as shunt malfunction, shunt infection, and abdominal seeding of a malignancy. Either procedure offers an opportunity to assay CSF for tumor markers and cytology. In rare cases, when hydrocephalus is not present, CSF sampling by lumbar puncture may be desirable prior to surgery, especially if CSF dissemination is apparent on pre-operative imaging studies. After CSF diversion, if cytology and markers are negative, a procedure to obtain tissue is indicated, via a stereotactic, an endoscopic, or an open approach.
Pearls
• Endoscopic third ventriculostomy offers many advantages over ventriculoperitoneal shunting in cases of obstructive hydrocephalus from a pineal region mass.
• Mild asymptomatic hydrocephalus might resolve following resection of a pineal mass, obviating the need for CSF diversion.
Pitfall
• In the absence of positive tumor markers, treatment of pineal region tumors requires a histological diagnosis. Up-front radiation can result in an ineffective and unnecessary radiation exposure.
 Diagnostic Biopsy
Diagnostic Biopsy
Stereotactic Biopsy
Stereotactic biopsy of tumors in the pineal region carries an increased risk of hemorrhage compared with biopsies in other regions of the brain, although the clinical impact of this risk may be small. Proximity to numerous vascular structures and CSF spaces raises the likelihood of bleeding during tissue sampling and the possibility that even minor bleeding will fail to tamponade. Additionally, biopsy trajectories typically pass adjacent to the lateral ventricle, risking penetration of pial surfaces en route to the stereotactic target. Biopsy series in which hemorrhage rates were calculated from systematic postoperative computed tomography (CT) scans found only a mildly increased incidence of biopsy-associated hemorrhages, the majority of which carried little, if any, clinical relevance.9,10
Some series have found a higher morbidity associated with pineal region biopsies compared with routine biopsies, whereas others have not. One retrospective multicenter study of 370 patients reported a mortality rate of 1.3%.11 Overall, reported complications seen after stereotactic biopsy of pineal region tumors are almost always transient exacerbations of existing symptoms.
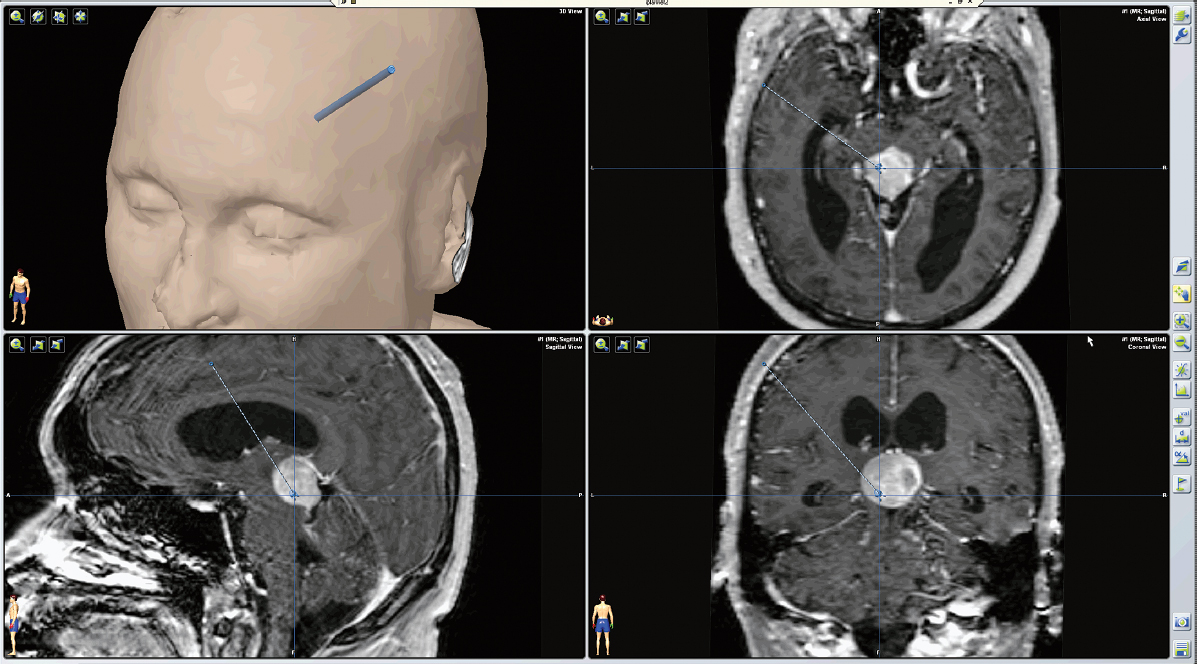
Although safe in experienced hands, stereotactic biopsy in the pineal region does require foresight and an appreciation of the complex anatomy surrounding the pineal region. An anterolateral-superior approach originating anterior to the coronal suture and lateral to the midpupillary line is usually preferred. Often a point just behind the hairline, at the superior temporal line, is convenient and cosmetic. This trajectory traverses the frontal lobe and internal capsule, staying lateral to the lateral ventricle (Fig. 30.1). Alternatively, a posterolateral-superior approach through an entry point at the parieto-occipital junction can be utilized but is most appropriate for tumors with lateral extension. In either case, multiple biopsies can be performed along the trajectory path to increase the diversity of tissue sampled.
Endoscopic Biopsy
Tissue can also be obtained endoscopically in the same sitting as a third ventriculostomy. Although a potentially elegant, “minimally invasive” surgical solution to CSF diversion and tissue diagnosis, it is only truly less invasive than separate diversion and biopsy procedures if performed through a single bur hole. With the vast majority of pineal region tumors, this requires the use of a flexible endoscope. Endoscopic biopsies carry a potentially higher risk of bleeding because the biopsy is taken through a ventricular surface where even minor and delayed bleeding can be difficult to control.
Drawbacks to Diagnostic Biopsy
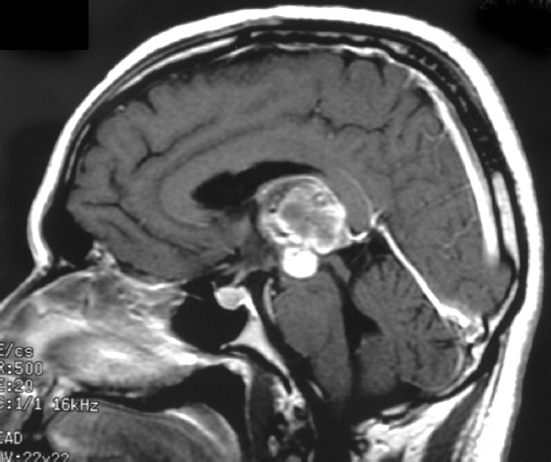
The major drawback to diagnostic biopsies in the pineal region is limited tissue sampling. Pineal region tumors are incredibly varied, are sometimes of mixed histology, and require different treatment paradigms depending on histological differences that are subtle and difficult to recognize even in experienced hands. Thus whether tissue obtained through a diagnostic procedure is truly representative of the entire tumor is always debatable (Fig. 30.2).
 Staging
Staging
Once a histological diagnosis has been made, a management strategy should be developed in collaboration with radiation and oncology specialists. Patients with ependymomas, malignant germ cell tumors, or malignant pineal cell tumors should have a complete contrast-enhanced MRI of the spine to look for metastases.
Special Considerations
• Tumor types such as ependymoma, pineoblastoma, and germinoma that are known to spread along CSF spaces require contrast-enhanced total spine imaging after diagnosis to rule out drop metastases (Fig. 30.3).
• Pineal parenchymal tumors are notoriously difficult to grade accurately. Pathological diagnoses should be performed with as much representative tissue as possible, and confirmed by a neuropathologist with specific expertise in pineal tumors.
Fig. 30.2 Sagittal T1-weighted contrast-enhanced magnetic resonance imaging (MRI) shows a pineal region tumor with a heterogeneous pattern of enhancement. Tissue obtained after craniotomy demonstrated a mixed germ cell tumor.
 Open Surgery
Open Surgery
Overview
Although a diagnostic biopsy is a reasonable first option in selected cases, an open approach is preferable in the majority of cases. Open surgery offers the potential to provide generous tissue sampling, to obviate a shunt by relieving obstructive hydrocephalus, and to proceed with a radical resection if indicated. Once tissue is obtained via an open approach, the decision to proceed with radical resection depends on an accurate histopathological diagnosis and the extent to which a particular diagnosis dictates a benefit from radical resection with an accepted rate of surgical morbidity.
Complications from open surgery range from transient exacerbations of existing symptoms to potentially devastating neurologic injury. Serious morbidity typically results from postoperative hematoma, venous infarction from vein sacrifice, thalamic injury, air embolism in the setting of a sitting-position craniotomy, and visual deficits from occipital lobe retraction. Pineal region surgery is certainly not trivial, but within the last 25 years major morbidity and mortality from published surgical series have improved dramatically and have dropped to 0 to 2% in published surgical series (Table 30.1).12,13
Pearl
• In some cases, gross total resection of a pineal region mass can obviate the need for a CSF diversion procedure.
Approaches
Several operative approaches to the pineal region have been described. The most effective and the most utilized are the supracerebellar-infratentorial approach, the interhemispheric transcallosal approach, and the occipital transtentorial approach.7,13,14 The optimal approach for a specific patient depends, to a degree, on the anatomic features of the tumor but is also influenced by the surgeon’s level of experience and comfort.
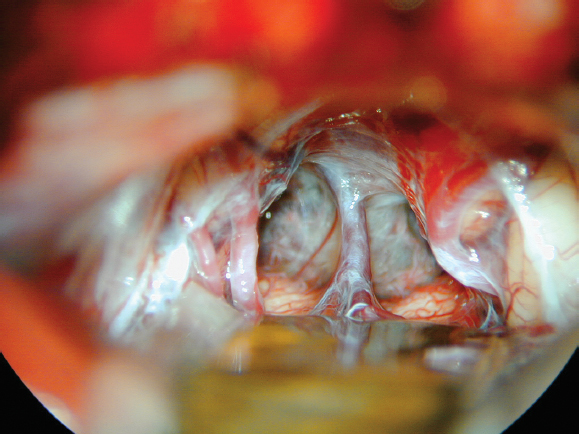
The supracerebellar-infratentorial approach is the most widely used and has the benefit of providing a direct midline approach through a natural corridor between the dorsal cerebellum and the tentorium (Fig. 30.4). This approach facilitates the dissection of the tumor from its attachment along the velum interpositum and deep venous system, which often represents the most difficult aspect of surgical removal.
The supratentorial approaches, including the occipital-transtentorial and the transcallosal-interhemispheric approaches, provide wider exposure than the infratentorial alternative but have the disadvantage of forcing the surgeon to work around and in between components of the deep venous system during tumor resection. The occipital-transtentorial approach requires occipital lobe retraction, which can result in visual field deficits, but once the tentorium is divided, excellent exposure to the pineal region from the quadrigeminal plate into the third ventricle is achievable. The transcallosal-interhemispheric approach requires retraction of the parietal lobe and often the sacrifice of bridging cortical veins to access the interhemispheric corridor.