Figure 190.1 Human papillomaviruses (HPV) are the cause of the most common sexually transmitted disease, genital warts, with an annual incidence of 6.2 million and a prevalence of 20 million infections. HIV = human immunodeficiency virus.
Rates of transmission differ according to body site: Transmission from penis to cervix is 58.8 cases per 100 patient years; from cervix to penis is 208.8 cases per 100 patient years. Nonpenetrative intercourse transmits HPV from the anus to the scrotum and from the hand to the penis.
Genital HPV infection
Of the more than 100 different DNA types of HPV, distinguished on the basis of relatedness of their genomes, 40 infect the genital area. These 40 genital types fall into two groups, distinguished by the type of disease that they produce. The first group, which includes the two most common HPV types, 6 and 11, causes exophytic condylomata, referred to as genital warts (Figure 190.2), as well as low-grade dysplasia of the vulva, vagina, and cervix.

Figure 190.2 Exophytic condylomata, also referred to as genital warts.
The second group, typified by types 16 and 18, causes SCC as well as high-grade dysplasia of the cervix, vagina, vulva, and penis, which appears as white areas of skin after the application of acetic acid (Figure 190.3). Low-grade dysplasia is referred to as squamous intraepithelial lesions (SIL) grade I, moderate dysplasia as SIL grade II, and severe dysplasia as SIL grade III. When the cervix is affected, it is termed cervical intraepithelial neoplasia (CIN) with similar grading as SILs. Both groups of HPV viruses may produce asymptomatic infection, subclinical disease, or clinically apparent disease (Figure 190.4).
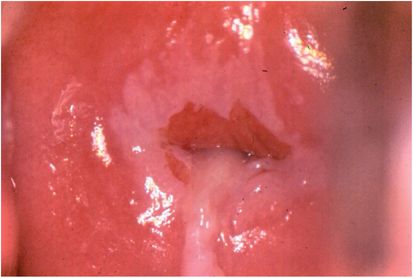
Figure 190.3 High-grade dysplasia of the cervix, vagina, and vulva, appears as white areas after the application of acetic acid.
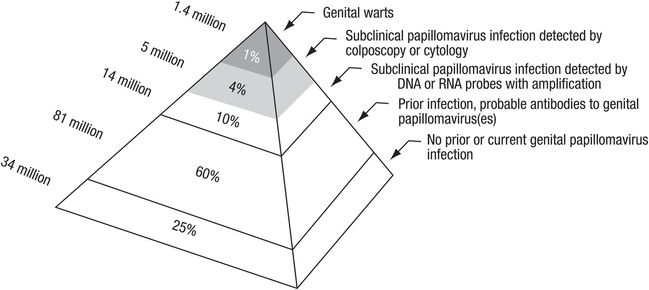
Figure 190.4 Human papillomaviruses may produce asymptomatic infection, subclinical disease, or clinically apparent disease.
HPV may also infect the perianal region and the distal rectum above the dentate line. In people infected with human immunodeficiency virus (HIV), HPV may produce small, innocent-appearing ulcers that on biopsy are proven to be SCC. HIV infection, as well as other immunodeficiency states, increases the likelihood that dysplastic lesions of the cervix may evolve into invasive carcinomas. Recurrent or refractory genital warts may be surrogate markers for concomitant infection by HIV, and it is important to test for HIV in patients with HPV infection.
Despite the enormous prevalence, HPV infections in the majority of woman usually resolve in 6 to 12 months. Up to 30% of infections by low-grade HPV types 6 and 11 may be transient. and will not evolve into a malignant state. Although moderate or severe dysplasia may also remit without treatment, women with these lesions should be evaluated by colposcopy to detect the development of carcinoma in situ. Women with persistent infection by the oncogenic HPV types are at risk for developing precancerous and cancerous lesions (Figure 190.5).
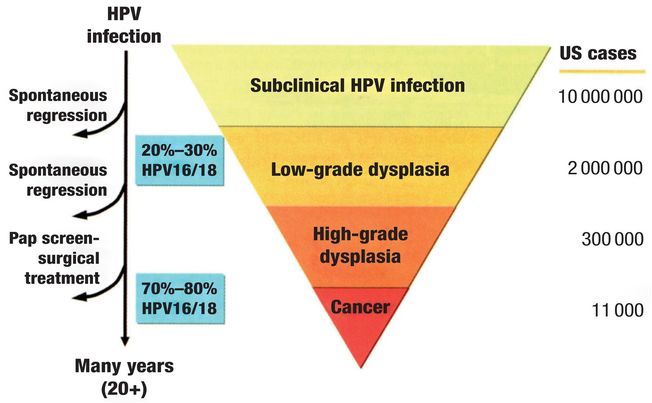
Figure 190.5 Infection by low-grade human papillomavirus (HPV) types may be transient.
HPV causes most cancers of the oropharynx
SCC of the oropharynx are associated with either tobacco/alcohol/betel nut use or HPV infection. HPV type 16 and, less commonly, types 18, 31, and 33 are found in 80% of these tumors. In SCC of the tobacco/alcohol/betel nut type, the host p53 and retinoblastoma oncogenes (pRb) are altered by the virus, while p16, a tumor suppressor, is decreased. In contrast, HPV-associated SCC of the oropharynx contains no mutations of the p53 oncogene and expression of pRb is downregulated, while p16 is upregulated. HPV+ tumors arise in the base of the tongue and tonsillar region, and show a much better response to chemotherapy than the other type.
HPV may be transmitted through open-mouthed kissing as well as oral sex. Among men with no oral sexual contacts, the risk of oral HPV transmission varies with the number of kissing partners. While the overwhelming majority of oral HPV infection clears with no intervention, the increasing prevalence of HPV-positive SCC of the oropharynx raises the question as to the benefit of vaccinating boys as well as girls, and at even earlier ages, to prevent oral, as well as sexual, transmission of HPV.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree