Chapter Outline
INTEGRATING PALLIATIVE CARE FROM THE TIME OF DIAGNOSIS
Advantages of Early Integration of Palliative Care
Enhancing Integration of Palliative Care When Cure is No Longer Possible
MAKING THE TRANSITION TO PALLIATIVE CARE
Discussing a Change in Prognosis
Creating a Plan for Care Based on Goals
Appointing a Health Care Proxy
Resuscitation Status and Other Aspects of Advance Care Planning
More than 2000 children die each year in the United States of cancer-related causes, and many more are living with advanced cancer. In children with cancer, it is not always possible to determine whether the disease will be responsive to cancer-directed therapy, nor is it possible to determine which type of path the dying process will take. Some children may die suddenly and unexpectedly, such as a child undergoing bone marrow transplant who experiences a treatment-related complication. Others may experience a steady and fairly predictable decline, such as the child with a progressive brainstem glioma after radiation therapy. Most children with progressive cancer will experience varying periods of chronic illness punctuated by crises, one of which may prove fatal. An example of this type of path may involve a child with relapsed metastatic neuroblastoma who may be palliated long term before experiencing a life-ending event.
Although intensive, interdisciplinary supportive care, that is, palliative care, is essential for all children with cancer, it is especially critical for children living with more advanced stages of cancer. Involvement of palliative care services has been shown to improve symptom detection and identification of communication needs among children with advanced cancer, but as of 2008, only 58% of Children’s Oncology Group institutions had dedicated palliative care services available, suggesting that there is still room for improvement. Nonetheless in recent years there has been greater awareness and integration of palliative care and, with this, care more consistent with its principles.
Palliative care, as defined by the World Health Organization, is an approach to care that improves the quality of life of patients with life-threatening illness and their families, through the prevention and relief of suffering by means of early identification, assessment, and treatment of pain and other problems, whether physical, psychosocial, or spiritual. The organization’s definition of palliative care appropriate for children and their families is as follows:
- •
Palliative care for children is the active total care of the child’s body, mind, and spirit and also involves giving support to the family.
- •
Palliative care begins when illness is diagnosed and continues regardless of whether a child receives disease-directed treatment.
- •
Health care providers must evaluate and alleviate a child’s physical, psychological, and social distress.
- •
Effective palliative care requires a broad multidisciplinary approach that includes the family and makes use of available community resources; it can be successfully implemented even if resources are limited.
- •
Palliative care may be provided in tertiary care facilities, community health centers, and the home.
Hospice and Palliative Medicine (HPM) became a formal physician subspecialty in 2006, and, currently, to become board eligible, a physician needs to complete a 1-year accredited fellowship program. However not all children with cancer require care by a HPM subspecialist or pediatric palliative care (PPC) team. Basic palliative care knowledge, skills, and behaviors should be known to all clinicians who care for children with life-threatening illnesses and conditions. The role of the HPM subspecialist and team is to provide clinical consultation for more complex situations, to provide education and training, and to improve palliative care outcomes for all children and families through quality improvement and research.
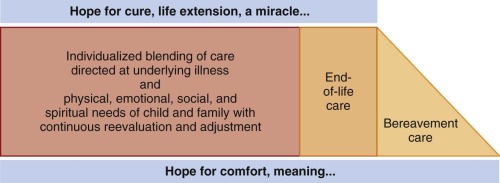
In fact both data and clinical experience favor a blended approach to care that includes disease-directed treatments together with palliative or comfort care. This approach is most often favored by parents, who commonly hope for life prolongation while also desiring maximal comfort and minimal pain and suffering for their child ( Fig. 70-1 ). Pediatric palliative care should not be a choice between life-prolonging treatments (e.g., chemotherapy for cancer) and palliative care. Rather pediatric palliative care should be integrated into an overall care plan that is individualized and adaptable over changing circumstances.
Integrating Palliative Care From the Time of Diagnosis
Although palliative care and end-of-life care are often considered to be a single entity, it is important to note that palliative care can be initiated at any time, not just in the end-of-life period. Rather than being restricted to the last phase of life, palliation includes attention to symptoms from the time of diagnosis. Palliative care also allows for discussion of goals and preferences for care long before death occurs.
In addition rather than precluding intensive life-prolonging care, palliative care can be complementary to therapy with curative intent. With the inclusion of palliative care early in the disease course, children can benefit from attention to symptoms and quality of life concurrent with efforts to control disease. Parents often have many goals of care beyond cure or life prolongation. Parents of children who died of cancer, for example, recall holding simultaneous goals of extending life and minimizing suffering during their child’s treatment course. Concurrent disease-directed care and attention to the physical, psychosocial, and spiritual needs of the child and family may be the optimal approach to meeting these seemingly conflicting goals.
Among some pediatric cancer patients, such as children with pontine gliomas, the pattern of progression is relatively predictable, making planning for the end of life a logical part of care from diagnosis. Patients with other cancers, however, may have long periods of disease control and relative clinical stability. Although ultimately the child may be expected to die of the disease, which relapse or acute decompensation will result in death can be very difficult to predict. Early relapses may be responsive to intensive treatment, and the timing of death may be difficult to predict.
For a child with relapsed neuroblastoma, for instance, many years may elapse between the first recurrence and death. At any moment in time, the use of intensive chemotherapy may seem reasonable and may offer significant hope of life prolongation and remediation of symptoms. However repeated intensive therapies including chemotherapy-related toxicity may not coincide with the family’s wishes for the end of the child’s life and may be associated with unnecessary suffering for the child. Even when families choose life-extending measures, they should have the opportunity to do so in the context of an understanding of the expected path of illness.
Advantages of Early Integration of Palliative Care
Before the patient is clearly in the last phase of life, physicians may find it difficult to initiate conversations about a poor prognosis. But the majority of parents of children with cancer say they want prognostic information, even when the news is upsetting. Patients and families who are poorly prepared for death tend to choose more intensive disease-directed care at the end of life. Without realistic information, they may not have the opportunity to make choices for care that are consistent with their values.
Just as physicians sometimes prefer not to discuss prognosis, pediatricians sometimes consider palliative care to be equivalent to hospice care. As a result they may integrate palliative care concepts such as advanced care planning and anticipatory guidance only once curative options have been exhausted. Yet families may find earlier integration of palliative care to be helpful. A study of bereaved family members of adult cancer patients, for example, found that half believed that palliative care was provided too late in the disease course, whereas less than 5% believed palliative care referrals occurred too early. Physician communication was found to be an important contributing factor; families who believed that the physician had communicated effectively about the patient’s prognosis and end-of-life care were less likely to believe that palliative care was introduced too late.
Early initiation of palliative care facilitates attention to symptoms and quality of life. Involvement of palliative care services improves symptom detection and identification of communication needs among children with advanced cancer. Similarly adults with advanced cancer tend to experience improvement in symptoms, including pain, anorexia, nausea, vomiting, sleeplessness, and constipation, after referral to palliative care services. In addition patients who receive palliative care frequently experience improvements in overall quality of life and well-being.
It is also possible that early discussions about palliative care can help parents to cope with the death. Mothers who experience the sudden death of a child tend to have more intense grief than mothers whose children die after a chronic condition. These findings raise the possibility that emotional and psychological adjustment before a child’s death can help parents to cope with the loss of the child over time.
Perhaps most importantly parents value preparation for the end-of-life period. In a study of bereaved parents of children with cancer, physician communication about what to expect in the end-of-life care period was a component of high-quality care. Parents who felt prepared for the circumstances surrounding the child’s death were also more likely to consider care to be of high quality overall. Communication with parents in advance of the child’s death may allow them to process and be prepared for the death before it happens and to make choices about end-of-life care that are right for them and their child.
Box 70-1 gives some general guidance for discussion about end-of-life preferences. Even if the patient’s outcome is uncertain, death can be discussed as a possibility so that the patient has opportunities to express goals for care.
Beginning the Conversation
“What is your understanding of what is ahead for your child?”
“Would it be helpful to talk about how his or her disease may affect him or her in the months and years ahead?”
“As you think about what is ahead for your child, what would you like to talk about with me? What information can I give you that would be helpful to you?”
Introducing the Possibility of Death
“I am hoping that we will be able to control the disease, but I am worried that this time we may not be successful.”
“Although we do not know for certain what will happen for your child, I do not expect that your child will live a long and healthy life; most children with this disease eventually die because of the disease.”
“I have been noticing that your child seems to be sick more and more often. I have been hoping that we would be able to make him or her better, but I am worried that his or her illness has become more difficult to control and that soon we will not be able to help him or her to get over these illnesses. If that is the case, he or she could die of his or her disease.”
Eliciting Goals of Care
“As you think about your child’s illness, what are your hopes?”
“As you think about your child’s illness, what are your worries?”
“As you think about your child’s illness, what is most important to you right now?”
“You mentioned that what is most important to you is that your child be cured of his or her disease. I am hoping for that, too. But I would also like to know more about your hopes and goals for your child’s care if the time comes when a cure isn’t possible.”
Introducing Palliation
“Although I hope that we can control your child’s disease as long as possible, at the same time I am hoping that he or she feels as good as possible each day.”
“Although it is unlikely that this treatment will cure your child’s disease, it may help him or her to feel better and possibly to live longer.”
Talking About What to Expect
“Would it be helpful to talk about what to expect as your child’s illness gets worse?”
“Although we cannot predict exactly what will happen to your child, most children with this disease eventually have [difficulty breathing]. If that happens to your child, our goal will be to help him or her feel as comfortable as possible. We can use medications to help control his or her discomfort.”
Talking to Children
“What are you looking forward to most of all?”
“Is there anything that is worrying you or making you feel afraid?”
“Is there anything about how you are feeling that is making you feel worried or afraid?”
Enhancing Integration of Palliative Care When Cure is No Longer Possible
Although integration of palliative care from the time of diagnosis is often ideal, sometimes a clinical event such as relapse or a severe complication makes it necessary to discuss a poor prognosis for the first time. A transition from care intended to cure the child can be experienced as a terrible loss for families. However as with discussions about care at the time of diagnosis, honest communication about the child’s prognosis can help the family make reasonable decisions about care, based on their values.
Delays in parental understanding of a poor prognosis can affect the care they choose for their children. In a study of parents of children who died of cancer, parents recalled understanding that the child was likely to die about 3 and one half months after the physician realized this. Earlier parental realization of the low likelihood of cure was associated with increased hospice use and decreased cancer-directed therapy in the end-of-life care period. Although parents sometimes have difficulty accepting a poor prognosis, the difficulty physicians have in communicating a poor prognosis also contributes to parents’ overly optimistic expectations about cure.
Making the Transition to Palliative Care
Discussing a Change in Prognosis
A statement that physicians can use when introducing this discussion with parents is, “Although I had hoped that your child’s disease would be cured and your child could live a long life, I am now worried that this is no longer possible.” Acknowledging the sadness of the situation, responding to the parent’s emotions, and allowing for silence can also be helpful. Parents may ask about treatment options, but such discussion should not obscure the fact that the child’s disease is unlikely to be cured. The physician might respond to such requests by saying, for instance, “It is possible that treatment might help your child to feel better and possibly live longer; the hope would be for the treatment to control the cancer for as long as possible.” Although these conversations are difficult for families and for medical providers, such honesty can help parents to make the best possible decisions for their child. In addition although honest provision of information is important, physicians may be able to clarify the goals of care without needing to have parents necessarily openly acknowledge that cure is not likely; this approach may be preferable to some parents.
Discussing Goals of Care
An important aspect of providing care for children with cancer is an understanding of the goals of care. Often these goals are identified by the parents, but adolescents and even younger children are often able to define priorities for their care as well. Understanding goals of care allows the medical team to make recommendations for care that fit with patient and family values. In addition goals of care, and conversations about these goals, provide another window into parents’ perceptions of what is ahead.
A discussion about goals of care can be started by asking parents what is most important to them as they think about what is ahead for the child. Specific questions about hopes for the future and worries about what is ahead can also be useful. Often parents will verbalize general goals, such as maintaining a good quality of life for as long as possible, minimizing suffering, prolonging life, or curing the child’s cancer. Parents often hold more than one goal and may have separate goals for cancer-directed and symptom-directed therapy; for example, goals of cancer-directed therapy may be to cure or to prolong life, whereas goals of symptom-directed therapy may be to lessen suffering and maximize quality of life. Although such goals may appear to be conflicting, holding more than one goal of care is normal, and physicians can make plans for care with both sets of goals in mind.
Acceptance of the parents’ goals is an important aspect of acknowledging the parents’ values, even when the goals are not in concert with the physicians’ goals. At times, however, parents will continue to articulate a goal of cure, when the medical team believes that such an outcome is not possible. Understanding what the parent would want if the child cannot be cured can help the medical team to make plans for care. Back and colleagues have recommended that the physician ask what the family would want if cure is not possible, a strategy described as hoping for the best but preparing for the worst. This strategy allows the medical team to have a conversation about what the family would want in such a situation.
Even when parents hold goals of cure, physicians need to have clear discussions about the goals of treatment, especially cancer-directed treatment. Depending on the circumstances, the oncologist may want to express goals of controlling the disease for as long as possible, for example. When the purpose of treatment is to help cancer research, with little hope of direct benefit to the child, that goal also should be stated.
In addition to the specific nature of goals of care, parents also consider a number of other values while they make these difficult decisions. For example parents sometimes think about what it means to be a good parent to their child as one compass for decision making. Parents may believe, for instance, that a good parent would focus on preserving the child’s life, would make unselfish decisions in the child’s best interest, or show the child that he or she is loved. In addition to helping parents clarify their own wishes, having conversations about the meaning of the good parent role can help clinicians to reinforce that role as the child’s illness progresses.
Similarly parents may use phrases to sum up the things that are most important to them: “I want the best for my child;” “I have to fight;” “I want my child to have quality of life.” By listening for and probing these phrases, clinicians partner with parents in clarifying their goals and making decisions. Ultimately these conversations about parents’ values allow clinicians and the parents themselves to recognize their values, enact them in the child’s care, and work together during these very difficult times.
Eliciting Children’s Goals
Children and adolescents may express goals in general terms, like their parents, or they may have very specific wishes, such as staying at home, spending time with siblings, or minimizing invasive procedures. Knowing about these goals, which can be elicited by asking children for their hopes and worries, and what is most important to them when they think about what is ahead, can allow the medical team to work toward meeting any specific hopes or needs.
Creating a Plan for Care Based on Goals
Once goals of care have been elicited, then a plan of care can be made. It is important to acknowledge that this plan is flexible and may change frequently. Importantly each family is unique, and even with similar goals there may be very different plans of care. As previously mentioned, pediatric palliative care should be integrated while a family is seeking a life-prolonging or potentially curative therapy. Therefore a plan of care may include preventative therapies, looking for life-prolonging or curative therapies, rehabilitation, and intensive quality of life and symptom management. Having parents consider these questions may help them with decision making.
- •
How will this treatment affect my child’s quality of life?
- •
What is likely to happen without this treatment?
- •
How will the treatment change my child’s prognosis?
- •
What will it be like for my child (and family) to go through this treatment?
- •
Are there other options we should consider that might have the same outcome but with a different approach?
Appointing a Health Care Proxy
For patients older than 18 years, the decision of whom to appoint as a health care proxy may provide an opportunity for discussion of care preferences. This document, often completed on admission to the hospital, allows the patient to designate someone to make medical decisions if the patient is unable to do so. The proxy ideally makes decisions based on knowledge of what the patient would want in various situations and not on what the proxy would want or believe to be appropriate. Most hospitals have standard forms that are completed by the patient and an admissions staff person. This could be an opportunity to explore the true wishes of the young adult patient and lead to rich discussion and meaningful decision making.
Resuscitation Status and Other Aspects of Advance Care Planning
Advance care planning may include (1) designation of a decision maker or, for those older than 18 years old, choosing a health care proxy; (2) discussion of the illness and prognosis; (3) establishment of goals of care; (4) discussion of preferences for resuscitation, artificial nutrition and hydration, and palliative sedation; (5) primary location of care and death; and (6) discussion about organ or tissue donation, including autopsy, and preferences for funeral arrangements. Advanced care planning is a process that requires time and often occurs through multiple conversations and at different phases of the child’s illness.
Of note many clinicians believe that these conversations happen later than they should. Clinicians cite multiple barriers to discussions about advance care planning, especially unrealistic parent expectations about the child’s illness, differences between clinicians’ and parents’ understanding of prognosis, and a lack of parent readiness to have these conversations. Clinician perceptions about parent understanding or readiness, however, should not preclude having these conversations. Physicians also report that they often do not know what to say.
Fortunately several resources are available to assist in these discussions. Five Wishes (for those >18 years) (available at www.agingwithdignity.org ) is a legal document in 37 states. This document presents information and questions in a way that enhances communication about these difficult subjects, and it addresses what kinds of nonmedical interventions would be wanted, such as music, prayer, presence of family, and so on. My Wishes (for those <18 years) (also available at www.agingwithdignity.org ) is not a legal document, but through simple questions and the opportunity to write and draw it affords the child or adolescent the opportunity to communicate his or her wishes. In addition Voicing My Choices has been recently developed for adolescents and young adults aged 16 to 28, using materials from Five Wishes and modified after interviews with adolescent and young adult patients with cancer or who are infected with human immunodeficiency virus. This work involves four priority areas, which can serve as a model for younger patients as well: the ability to express and document preferences for (1) the medical treatment they want and the treatment they do not want; (2) how they would like to be cared for; (3) information they want family and friends to know; and (4) how they want to be remembered.
Other techniques may be helpful, such as asking an adolescent to name his or her wishes, realistic or not. The provider may also ask a question such as, “What is your understanding of your illness now?” Another technique is to suggest that the adolescent write, with a trusted person, such as a child life specialist, psychosocial clinician, or parent, what questions he or she would like to ask of the health care team. Ideally advance care planning among adolescents is family centered, with the family and adolescent both taking part in shaping wishes for care, in an effort to develop a plan for care that all can support. Doing so can allow families to understand their adolescent’s wishes and ultimately carry out these wishes.
Making Recommendations
Even when curative therapies are no longer sought, families report wanting recommendations regarding available interventions. Most do not want the burden of making decisions completely on their own. Providers may believe that, especially when there are treatments with uncertain or marginal benefit, plans for care should be the parents’ choice. However parents can often be best supported by providers who clearly discuss the positives and negatives of each treatment or therapy and then recommend a treatment in the context of the family’s goals and values. This can apply to a wide spectrum of situations such as participating in a phase I or II clinical treatment trial, putting in a chest tube for pleural effusions, using intravenous antibiotics to treat an infection, or instituting a do not resuscitate (DNR) order. Clinicians who make recommendations can alleviate this burden from the parents and help to minimize the parents’ sense of regret and responsibility for choices that ultimately allow death to occur.
Communicating Plans for Care
A plan of care must then be communicated to all involved in the child’s care. Consistency and honesty are among what bereaved parents tell us is most important. Written documentation of team meetings, family meetings, and the care plan is essential. Documentation can also help to communicate plans of care with other providers, such as the home care team or those providing emergency services. Along with a home DNR or comfort care form, for instance, a letter that documents the child’s situation and plans for care can be carried by the parents to help ensure that any care providers they encounter know their goals for care. By partnering with the child and family, the health care team in the hospital or home has the opportunity to enhance quality of life while the child is living and affect the grieving and bereavement that will follow for the family.
Talking with Children about Advanced Illness
To tell or not to tell? This is the question that typically arises when parents and health care providers of children with life-threatening illnesses face the issue of discussing prognosis with children. Health care providers have reported a wide range (10% to 80%, with a median 45% prevalence) of open discussions among parents and children regarding the child’s impending death. Of a sample of 429 parents in Sweden, 34% discussed death with their child, and none of those parents regretted having this discussion. When children were given the information that their illness was terminal, most (63%) received it from the parent and physician together. In addition, several studies have shown that children as young as 6 to 10 years old are willing to participate in end-of-life decision making. Parents’ and health care providers’ distress in navigating these communication processes (especially regarding death) may prevent children and families from accessing appropriate and timely pediatric palliative care.
Parents may be reluctant to discuss death with their child because of the understandable worry that such a conversation may be very upsetting to the child. However children may have some understanding that death is likely but, because they sense the parents’ distress, may feel unable to discuss this topic with a parent. This choice often stems from concern for the parent’s well-being. Providing the child with an opportunity to talk, however, can be therapeutic for the child. We therefore often encourage parents to allow for such an opportunity. For parents to initiate discussion, they need to be supported for their efforts in broaching and carrying out these difficult conversations with their child. When parents were asked how they best could be supported during end-of-life care of their child, they responded by saying that respect for the family’s role, comfort, spiritual care, access to care and resources, communication, support for parental decision making, and caring/humanism were central.
By describing to parents a nonthreatening mode of communication when carrying out discussions with their child, centered on exploring what the child knows and what the child may be worrying about and hoping for in the time ahead, we can often reassure parents that this conversation will be sensitive and guided by the needs of the child.
The needs and wishes of the individual child should guide how communication takes place and its content. A child’s age and level of cognitive development as well as the changing comprehension of death by age can help shape the appropriate conversations regarding the prognosis, treatment choices, and end-of-life decisions; however, all this information cannot necessarily predict what a child understands about death. Furthermore depending on the disease (e.g., brain tumor), the act of communication may be functionally difficult on the part of the child. Thus careful assessment of a child’s physical abilities, maturity, level of comprehension, and coping abilities rests on the family and health care team. Himelstein explains appropriate communication interventions (i.e., language, details, expression, participation) based on age ( Table 70-1 ). Chesler and colleagues found that the age at which the child was diagnosed with cancer was strongly and significantly related to the amount of information the parents provided about the illness: the older the child, the more information was given. However, in another study that retrospectively collected information regarding psychosocial variables on 45 pediatric oncology patients who died, it was found that children between the ages of 3 to 6 years had more information about their own death from their parents than older children between the ages of 7 to 11 years. The investigators concluded that perhaps children in the younger age group had a “magical concept” of death, thus making it easier for caregivers to discuss end of life with these younger children. Hurwitz and colleagues provide questions and statements children raise about dying at various ages, thoughts that guide the behavior, their underlying developmental understanding of death, and strategies and responses that can help children in these situations ( Table 70-2 ).
| Age Range | Characteristics | Predominant Concepts of Death | Spiritual Development | Interventions |
|---|---|---|---|---|
| 0-2 yr |
| None |
|
|
| >2-6 yr |
|
|
|
|
| >6-12 yr | Has concrete thoughts. |
|
|
|
| >12-18 yr |
| Explores nonphysical explanations of death. |
|
|
| Examples of Questions and Statements About Dying | Things That Guide Behavior | Developmental Understanding of Dying | Strategies and Responses to Questions and Statements About Dying |
|---|---|---|---|
| 1-3 Years | |||
| “Mommy, after I die, how long will it be before I’m alive again?” “Daddy, will you still tickle me while I’m dead?” | Understanding of accidental events, of future and past time, and of the difference between living and not living is limited. | Death is often viewed as continuous with life. Life and death are often considered alternate states, like being awake and being asleep, or coming and going. |
|
| 3-5 Years | |||
| “I have been a bad boy, so I have to die.” “I hope the food is good in heaven.” |
|
|
|
| 5-10 Years | |||
| “How will I die? Will it hurt? Is dying scary?” |
|
|
|
| 10-13 Years | |||
| “I’m afraid if I die my mom will just break down. I’m worried that when I die, I’ll miss my family or forget them or something.” |
|
|
|
| 14-18 Years | |||
| “This is so unfair!” “I cannot believe how awful this cancer has made me look.” “I just need to be alone!” “I can’t believe I’m dying. … What did I do wrong?” |
|
| “I can’t imagine how you must be feeling. You need to know that despite it all, you are doing an incredible job of handling all of this. I’d like to hear more about what you are hoping for and what you are worrying about.” |
Assessing the child’s level of autonomy, perception of threat and safety, and individual coping style can help the clinician determine how to communicate with the child regarding palliative care. Independence and individuation will vary. For example, some adolescents, especially those who have close relationships with their parents, may not make a lot of the day-to-day decisions on their own and depend on their parents’ authority and life experience for critical decision making. Other adolescents may be accustomed to “heading” the household and making many of the daily decisions for a family.
Understanding the child’s family history with regard to illness and experience with death are important components to consider when broaching sensitive issues within palliative care. A child who has previously witnessed a relative die or suffer from a serious illness and observed his or her family’s grief may have unique needs related to this experience. Children who are accustomed to making decisions along with their siblings may request to have siblings present during important decision-making events.
Understanding whether the child has a current and/or premorbid history of anxiety and/or depression is also critical in how information is delivered during advanced care planning discussions.
Within the framework of the American culture is the diversity of the various ethnic and religious cultural subgroups that utilize a range of guiding principles with regard to illness and truth-telling. It is critical to assess the family’s identification with their particular culture and inquire what their beliefs are with regard to communication with children about issues pertaining to advanced care, because this may vary from the protective approach (shielding young patients and siblings from full knowledge of the disease) to a more open approach. Although every family’s style of disclosing sensitive information may be different for a variety of reasons, health care providers should consider how parents may feel if they do not prepare their child for impending death, because this has been shown to have long-term implications for parental grief.
Techniques for Communication
In many instances communicating with children regarding palliative care issues is best received when health-care professionals are aware of the child’s level of desired information and concurrently reinforce the primary role of parents. Children between the ages of 8 and 17 years who were interviewed about disclosure regarding their diagnosis and prognosis reported a range of views about the form of disclosure they preferred: a few believed it was better to hear the news at the same time as their parents, some thought it was more appropriate for their parents to be told first, and others reported no strong feelings either way. Patients reported the roles their parents performed in facilitating communication with their health care team: asking questions for them, being the source of information, and reframing the information from the health care team so they could understand it better. Some children reported feeling “protected” by the parent’s executive role in screening the communication with doctors and “marginalized” by the nonparticipant status. Parents of cancer survivors indicated that the shielding of information that took place (i.e., preference regarding whether to provide information to their child about prognosis and treatment options) depended on their child’s age and emotionality.
The range of views reported by pediatric patients exemplifies the necessity for tailoring one’s approach of communication to the individual child. The most beneficial method for determining the most appropriate way to communicate with a particular child is by spending time with him or her. A provider who knows the child well may be best suited for this conversation whenever possible. Prior to the delivery of information, it is helpful to uncover what the child already knows. This can be done through direct conversation or through nonverbal communication (e.g., drawing and symbolic play). Storytelling, such as using the experience of another family with a child or a loved one facing death, may be another modality that can be used by parents and health care providers to broach sensitive topics related to death. Ensuring privacy, confidentiality, and support can facilitate the trust that is needed for the child to disclose what it is that he or she already knows. The next step is finding out what the child wants to know. Then the clinician can give information in small amounts, responding to the child’s reactions and feelings; and can remind the child that there will be additional opportunities to discuss the issues of concern.
Listening
Listening to a child cannot be underrated nor underutilized. Because a child confronting a life-threatening illness is at his or her most vulnerable, listening to the child can be a very powerful tool in placing some of the control back in the hands of the child. Allowing moments for silence in the discussion only reinforces this acknowledgement that the clinician is listening. Providing a child with a tape recorder can be another method for empowering the child. This allows the child to record his or her questions for the upcoming appointment with the clinician, and also allows them to record the clinician’s answers so they can be reviewed if necessary. Asking about and listening to the child’s priorities and providing choices, when possible, may allow the child to participate in “life-enhancing experiences even at the close of life.” (p 746) Listening to the voice of the parent(s) goes hand-in-hand with listening to the child to provide comprehensive family-centered care; it can provide helpful information about the child and make the health care provider a better listener for the child. Listening to the parent without the presence of the child can also be a valuable tool in certain instances when the child’s presence may restrict communication.
Spirituality
Spirituality can be regarded as a multidimensional (mind, body, spirit), unique expression that brings individuals hope, meaning, and purpose. Spirituality is related to, but different from, religion, such that “spirituality is a dynamic state of being in which the individual seeks connectedness, whereas, religion represents the beliefs, values, practices, and rituals that are an observable aspect of a person’s spirituality.” (p 56) Spirituality is often “inexpressible” whereas religion is marked by greater structure. A child can have a “highly developed awareness of spiritual concepts without ever having been part of a formal religious group.” (p 271)
Spirituality in Children
Similar to the development of cognitive abilities, children display a developing awareness of spiritual needs, meaning, or purpose within their lives at various ages. During infancy, children find meaning in their daily life through unconditional love and trust. Toddlers desire self-assertion, worthiness, and success when performing new skills. Preschoolers and school-aged children tend to derive their satisfaction from learning concepts of right/wrong, impulse control, and the benefits of peer socialization. Adolescents find purpose in their developing independence, individuality, and a deeper relationship with a higher being. For a child with a life-threatening illness, spiritual concerns often include a need for unconditional love, forgiveness, hope, safety and security, and development of a legacy. Children also often experience loneliness and loss of wholeness. It can be helpful for children of all ages to be assured that they bring meaning to their families lives and that when they are no longer alive they will be remembered by their family.
Children, in general, more than adults, tend to attribute an illness to “internal” (personal) factors, as opposed to “external” (environmental) factors. Children younger than the age of 7 years, who have yet to develop the ability to think abstractly, often see illness as a form of punishment for something they have done wrong (immanent justice belief). Although some older children may attribute the illness to internal causes to maintain control, others are able to attribute the illness to external causes but also seek out the meaning and purpose of their illness—a task that is very often spiritual.
The Spiritual Assessment
Because children tend to reflect the religious and spiritual values of their parents and family, a family-centered assessment of spirituality is often helpful. Providing spiritual care for parents can prepare them for the questions children ask, such as, “Why is God doing this?” or “What is heaven like”? Parents need assurance that there is no specific “right answer.”
One method for conducting a spiritual assessment is through the use of the B-E-L-I-E-F questions:
B elief system (e.g., Does your family take part in religious events/rituals? Have you discussed the idea of afterlife with your child? Do you believe in a higher power that influences your life?)
E thics or values (e.g., What are the values you believe are most central to your family?)
L ifestyle (e.g., Are there rituals or dietary practices that you/your family follow?)
I nvolvement in a spiritual community (e.g., Are you involved with a spiritual community?)
E ducation (e.g., Do you/your family receive or have received religious education?)
F uture events (In the near future, are there any religious rites of passage set to occur for you or your family members? What role would you like the members of your faith community to play in the spiritual care of your child?).
However most spiritual counselors and chaplains discourage the use of a “checklist format” in assessing spirituality. Instead questions could be posed to the family and/or to the child in a conversation format depending on the situation. Clinically effective pediatric spiritual assessments are conducted in narrative form and may use words, pictures, music, and play, thus inviting a child to explain his or her sources of strength and areas of fear. Discussions with children and their families regarding spirituality early on in the disease course can help bring meaning to what the family is enduring and can provide hope and comfort at end of life. Assessing children’s developmental understanding of faith using Fowler’s stages of faith can be helpful in knowing how to lead these spiritual conversations with children directly and how to guide parents in doing so:
Stage 1: Intuitive Projective Faith (2-7 years) is when children’s thinking is filled with fantasy and notions of faith are based on stories usually told by parents and other caretakers.
Stage 2: Mythic-Literal Faith (7-12 years) incorporates children’s knowledge of cause-and-effect relationships into separating fact from fantasy when constructing an understanding of faith and their religious expression.
Stage 3: Synthetic-Conventional Faith (12-21 years) is when adolescents are able to use abstract reasoning skills to develop their own spiritual identity by separating out what has been told to them and creating new connections between faith-based stories and their own beliefs.
Facing obstacles, challenges, and adversity in life often engenders spiritual thoughts and prompts adults and children alike to ask questions of a higher power, such as, “why me?” “why my child?” It is natural that spirituality is a significant issue for families of children with cancer. Pastoral care providers at children’s hospitals estimate that more than half of child patients can benefit from spiritual care for fear, anxiety, coping with pain, and familial difficulties. Providers in this study identified three major barriers to providing spiritual care: “inadequate training of health care providers to detect patients’ spiritual needs, inadequate staffing of the pastoral care office, and being called to visit with patients and families too late to provide all the spiritual care which could have been provided.” (p e70) When the focus of clinical care is on “the cure” for children, treatment discussions focus on medical facts and issues centered on resolving the “problem” with medications or therapies; spirituality, in palliative care, by contrast, is more about a journey of meaning, where there may be no clear solution. Providing spiritual care to dying children and families requires the professional to face his or her own issues with spirituality, something not all individuals have done or are ready to do. Children’s spirituality tends to be overlooked and, as a result, children may be more likely to feel unheard, invalidated, and alone in the end-of-life period. A focus on spiritual beliefs during the end-of-life period is not only critical to the dying patient but also can have implications for bereavement outcomes, such that people who profess stronger spiritual beliefs may experience a more rapid and complete sense of closure after the death of a loved one.
School
Going to school provides multiple benefits for the school-aged child with cancer. It is the child’s peer group; it is the child’s chance for discovery, mastery, and socialization. Most children want to continue with their class unless they have not been well supported or they feel unable to participate. With the family and child’s permission, creative solutions for participation can allow the child to remain in school often until just days before death. Preparation of school staff and classmates is important, as is a willingness on the family’s part to allow for candid information about the child’s illness and treatment course.
Ideally this information is shared soon after a child is diagnosed. Often hospital or clinic staff will travel to the child’s school and provide information through a “back to school” program. The question frequently arises during these sessions as to whether the child/friend/peer will survive. Most school-aged children have known an adult with cancer, some who have survived and some who have not. Addressing this question in a hopeful way while acknowledging the uncertainty is essential. In all instances if the child dies, it is important for schools and communities to have a plan about ways to communicate this information and support classmates’ questions, fears, and feelings.
One possible disturbing aspect of school attendance by the ill child may be the change in the child’s physical condition. Reassuring classmates of the child’s unchanging personhood may be necessary. Explaining absences, altered appearance, and altered ability to participate in regular class activities may also be helpful.
For the ill child to attend school, school staff and medical providers may need to be creative. Perhaps the child is allowed to attend for half days or just for lunch or on special activity days. Even limited time can be meaningful for the child and his or her peers. An individualized education plan (IEP) tailored to the needs of the child can also allow resources to be mobilized. An ill child should be able to receive home or hospital schooling, and some may be able to complete computer courses or stay in touch with the classroom via teleconferencing.
Advance Care Planning and the School System
As a child’s disease progresses, the family and medical team may decide together that a DNR order should be in effect. This can present challenges as to how to honor this within a child’s community. Many states are in the process of adopting medical orders for life-sustaining treatment to provide consistent communication regarding advanced care decisions for loved ones no matter what the location of care. However most school districts do not have guidelines or policies to deal with this kind of situation, and those that do have policies typically prohibit school staff from honoring an order that would limit attempts on resuscitation. Nonetheless ethical principles of beneficence, nonmaleficence, and autonomy have been offered as justification for honoring limits on attempts at resuscitation for the student. At this point each child, family, and school will need to come to some clear agreement of whether abiding by medical orders for life-sustaining treatment would be observed if the child was at school during a life-ending event.
Grief and Bereavement in the School
Finally anticipatory grief and bereavement needs of classmates and school staff must be considered. Resources are available (e.g., www.dougy.org ); however affording the training and opportunities for staff to integrate this into their knowledge and experiential repertoire may be challenging. It may be helpful for the oncology clinicians who helped treat the child as well as palliative care staff to do an in-service or advise school personnel. Because children with life-threatening illness are living longer, however, acceptance of their goals to enhance their quality of life must be honored whenever possible.
Interdisciplinary Care
The interdisciplinary team is an essential aspect of palliative care for children. How else could we possibly address the physical, social, emotional, and spiritual needs of the child with a life-threatening illness and the family as well? Ideally the team is providing care from the time of diagnosis through death and bereavement. Because care may occur in the hospital, home, or community, most often the child has a primary team (pediatrician or oncologist) whose members take the lead in day-to-day management. Most often the team consists of a physician, nurse practitioner or nurse, and social worker. Other core team members include a psychologist, chaplain, child life specialist, and case manager. The needs of the child and family require an entire team to provide the holistic care that is synonymous with palliative care.
Interdisciplinary care occurs with the child and family as partners. Priorities of the family are elicited, with their values, beliefs, and culture taken into account as recommendations are made that inform the necessary decision making. Family meetings, especially those used to address goals of care, include the parents, the child if appropriate, and interdisciplinary team members, so that information, emotional cues, and nonverbal language may be appreciated from different perspectives. This format also allows for a response that may address the issues holistically. In addition to those already mentioned, at times an interpreter, physical therapist, teacher, respiratory therapist, nutritionist, or pharmacist is present for the family meeting. Importantly, research has shown that when the physician is working with a psychosocial clinician there is closer agreement between the physician and parents in the understanding of the child’s prognosis.
Interdisciplinary care is essential so that not only the child’s and parents’ needs can be addressed but also those of the extended family, community groups, and the hospital, clinic, and home care staff. Particularly when doing a home visit, it is helpful to have several team members present so that physical and emotional needs of the patient, parents, and siblings may receive attention. Each team member carries the responsibility to inform, teach, and reach out to colleagues. Depending on one’s clinical setting, there inevitably will be times that different team members are called on to take the lead.
Pediatric palliative care is particularly challenging. As providers, we have “an obligation to nurture relationships that can hold within their embrace both vulnerability and suffering: that which is experienced by our child patients and their families, and that which we experience within ourselves.” The depth and meaning of this care touches us at our core. We need the expertise, support, and companionship that interdisciplinary care provides.
Coordination of Care
The coordination of care for a child with a life-threatening illness who moves between hospital, home, clinic, and perhaps a rehabilitation facility is daunting. Despite the efforts of many providers, parents often report feeling overwhelmed with the responsibility of care and coordination of services, particularly in the home. There are many barriers to coordination of pediatric palliative care services, including lack of available staff to provide home-based services; limited training of staff in pediatric palliative and hospice care; few resources for services; limited agencies with comprehensive services; and insufficient systems to support communication and coordination between sites of care. Ideally each hospital, clinic, community, or home care agency has designated personnel to perform coordination tasks for the child and family and has protocols specifying a standard of practice.
Thankfully, in the United States a growing number of home care agencies have developed palliative care programs that serve as a bridge to hospice services for children not yet meeting hospice eligibility criteria (<6 months to live) or for those seeking intensive disease-directed therapies. Previously the reimbursement structure and use of medical technology (e.g., intravenous nutrition, assistive respiratory support), experimental therapies, and/or need for block hours of nursing care had precluded enrollment of children on the hospice benefit.
Importantly section 2302 of the recent Patient Protection and Affordable Care Act, termed the “Concurrent Care for Children Requirement” (CCCR) has eliminated the requirement that Medicaid patients younger than 21 years forgo curative or life-prolonging therapies to be eligible for hospice. Therefore Medicaid programs in every state are now required to provide concurrent curative/life-prolonging treatment and hospice services for hospice-eligible children. The development of systems to make such concurrent care a reality has been slow and, in the meantime, a number of state-based pediatric palliative care coalitions have formed to jumpstart access to home-based pediatric hospice/palliative care services, using strategies such as Medicaid waivers or state plan amendments to increase coverage for hospice services. For example Massachusetts implemented a statewide pediatric palliative care program in 2006.
Location of Death
At the end of life, children and families often benefit from intensive support. It is generally assumed that children would prefer to be at home to die, although approximately half of children with progressive cancer die in the hospital, as do the majority of infants and children who die in the United States. In a study from the United Kingdom, research showed that of children dying in the hospital, 85.7% died in the intensive care unit, with the trend having increased over the years from 1997 to 2004. Families and children need to feel safe and well cared for and given permission, if possible, to choose location of care, be that at home, in the hospital, or a hospice house. Asking children where they would most like to be even if they are very sick and what is most important to them is often very instructive.
Although seemingly contradictory, the philosophy of palliative care can be successfully integrated into a hospital setting, including the intensive care unit, when the focus of care also includes the prevention or amelioration of suffering and improving comfort and quality of life. All interventions that affect the child and family need to be assessed in relationship to these goals. This proactive approach focuses on what “we can do” not what we cannot do. We might ask what can we offer that will improve the symptoms and quality of this child’s life (e.g., radiation therapy, a trip to the garden, a special visit from a pet) and provide the most meaning and control for their family instead of asking what interventions are not going to be offered. Staff needs education, support, and guidance because pediatric palliative care, like other types of intensive care, is an area of specialty.
Preparation for Home Care
Preparing parents for events that may occur at home is essential. Even if they may not want to talk about this, written materials can be offered. Anticipating likely symptoms, ways to manage the symptoms, what resources will best match needs, and who will be available on call 24/7 to the family is key to making the transition to home successful. The child’s primary inpatient or clinic providers must work closely with the case managers and social workers who know the intricacies of insurance benefits, home care nurses, and durable medical equipment vendors and who can determine what each can and will provide. It is also important to reach out to the primary care provider, who may have important insights to the home environment and resources in the community.
Even the most experienced families still need maximum physical and emotional supports in the home to care for a child who is facing the end of life. The goal is to have enough support in place so that parents can simply be “parents” and so that family interactions and events may become meaningful experiences.
Hospice Services
For those families and children who know they want to be at home, hospice services can be invaluable. Many hospice agencies now have palliative care programs, which offer greater flexibility and broaden the scope of care. There are many barriers, however, to provision of hospice services to children even with the new legislation section 2302 of the Patient Protection and Affordable Care Act. Many fewer children than adults die, and so maintaining a staff that is willing and able to provide care to children can be challenging. Families and practitioners often see hospice as “giving up,” and it remains difficult to change this assumption. There is a prognostic requirement of life expectancy of less than 6 months, and this can be a significant emotional barrier for families and clinicians. Financially provision of hospice may also be a struggle, because hospice is mandated to provide all the personnel, medications, equipment, and supplies that the child needs and this is capped at a per diem rate. The financial concerns may be mitigated with successful implementation of the Affordable Care Act, which should be reassessed over time.
The first free-standing pediatric palliative care center in the United States, the George Mark House, opened in 2004, and other pediatric hospice houses have followed. Some adult hospice houses are now willing and equipped to accept a child, with the hospice staff often appreciating the support of a previously involved pediatric palliative care team. In addition to hospice care there is a monumental unmet need for many families who are in desperate need of respite care for their child, who may have a prolonged palliative care path ahead of them.
Despite these barriers, palliative care, respite care, and hospice care for all children with life-threatening conditions is the recommendation of the Committee on Bioethics and Committee on Hospital Care. Importantly when experienced in caring for children, hospice teams are ideally suited to provide comprehensive home-based services to the child, siblings, parents, and extended family. Hospice programs often have physicians, nurses, social workers, chaplains, and bereavement staff, art therapists, music therapists, pet therapists, and volunteers who can provide integrative therapies such as massage and Reiki.
Cancer-Directed Therapy
Parents often wish to continue some form of cancer-directed therapy in the end-of-life care period and are more likely to favor using cancer treatment at the end of life than clinicians. The choice of cancer-directed therapy should be considered in the context of goals of care. For example if a parent’s primary goal is to minimize the child’s suffering, then an option that causes few distressing side effects and that necessitates few interventions may be a reasonable choice, if parents wish to continue to provide cancer-directed therapy.
Some regimens with limited toxicity have established efficacy in relapsed or refractory tumors. For example, daily oral etoposide has been used in children with refractory solid tumors, with limited resulting toxicity and with the possibility of tumor response. Oral temozolomide has had similar results in children with neuroblastoma. In refractory acute lymphoblastic leukemia, maintenance-type regimens of 6-mercaptopurine, low dose methotrexate, vincristine, and prednisone may be effective without causing significant side effects. Antibody therapies, such as rituximab for children with B-cell malignancies, and molecular agents, such as imatinib in potentially responsive cancers, may also offer palliation with limited toxicity. Other examples of therapies with limited toxicity can be found in the literature.
Other parents may wish to continue more intensive regimens of chemotherapy. Recent work has found that, when prescribing chemotherapy for children with no realistic chance for cure, oncologists consider the potential toxicity of the chemotherapy, family preferences, and the potential that therapy will decrease cancer-related symptoms. However, nearly half of oncologists studied had prescribed chemotherapy to meet parental wishes, and many oncologists’ recent experiences with end-of-life chemotherapy did not meet their goals of prescribing. Thus physicians should ensure that such regimens offer reasonable hope of meeting the parents’ and child’s goals of care.
Parents may also wish to pursue experimental options such as those provided on phase I clinical trials. In general the likelihood of significant benefit from agents offered on phase I trials is limited, typically under 8%, even in children. Misconceptions about the purpose of phase I trials are common; as with other clinical trials, many subjects believe that the purpose of such a trial is to benefit them personally rather than to benefit future patients. When clinical trials are offered, clarity about the purpose of the trial is important so that parents and children can make informed decisions about whether such therapy will help to meet their goals. In addition such therapies do not preclude concurrent attention to symptoms and quality of life. In fact attention to life prolongation and symptoms simultaneously may best meet the needs of children with advanced cancer and their families.
Other cancer-directed options to be considered include local irradiation or surgery. If a single lesion is causing significant pain or other symptoms, then localized radiation therapy may offer palliation with few systemic side effects. Radiation therapy directed at an isolated painful bony metastasis is one such example. Surgery can be similarly beneficial, but a frank team discussion with the surgeon about the possibility of recovery and the likelihood of recurrence can help in consideration of the likelihood that the child will benefit from the surgery. Debulking of a rapidly growing abdominal tumor, for example, may provide little benefit, in contrast to control of a single painful metastasis by radiation or surgery. A consistent recommendation between the oncologist and surgeon or radiation oncologist should be provided to the family.
Physicians sometimes feel an obligation to describe cancer-directed therapy as either “curative” or “palliative.” Such a distinction may be difficult, however, because at times cancer-directed therapy may offer some chance of cure, even if this chance is low, as well as some possibility of symptom palliation and life extension. In addition this distinction may be difficult for families, who may hold more than one goal for care. We recommend rather than using a label of curative or palliative, that cancer-directed therapy be discussed in terms of the goals for care. For example we may be able to tell parents that the goals of a particular therapy are to control the disease for as long as possible, with a very small possibility of cure, and with a higher likelihood of decreasing symptoms for a period of time. If cure is clearly not a goal of therapy, then that also should be stated.
Families who have been accustomed to using cancer-directed therapy at every recurrence may continue to pursue such options even when the medical team believes that the likelihood of benefit is extremely low. Unfortunately previous work suggests that parents may regret decisions made about end-of-life cancer treatment in retrospect, especially if treatment involved suffering. Thus clinicians should do everything possible to ensure thoughtful decision-making prospectively. In addition when such situations arise, the team should reach consistent recommendations about cancer-directed therapy and should not offer therapies with no chance of benefit and a high risk for harm. However patients and families will have different preferences for end-of-life care; and for some families, continuing to “battle cancer” until the time of death may hold personal meaning. The team should therefore follow the same standards for communication that we have described earlier: assess the family’s understanding of prognosis, allow for further communication about the prognosis if needed, elicit goals of care, come to a team consensus about plans for care that fit with goals, and make recommendations for care based on family and patient goals and the team’s consensus. Intensive interventions may be chosen by families who have overly optimistic perceptions of prognosis ; ongoing communication about the child’s prognosis may allow families to readjust goals and to choose interventions that offer realistic chances of benefit. The team should never be obligated to provide care that is considered to be inappropriately harmful and in such cases should work with hospital ethics teams to define appropriate responses to family requests. But beyond the reaches of harm, families who make thoughtful decisions about care for their children should be allowed to do so, even when plans for care do not match the ideals of staff members.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








