(1)
Department of Anesthesiology, Ichikawa General Hospital, Tokyo Dental College, Tokyo, Japan
Abstract
Palliative care is an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness. For pain assessment, it is important to obtain not only the onset, duration, location, quality, pattern, character, and intensity of pain but also aggravating and relieving factors, associated symptoms and signs, and current pain management agents and their effectiveness. To treat cancer pain, this principles can be summarized in five steps (by the mouth, by the clock, by the ladder, for the individual, and attention to detail). The use of opioids should not be affected by unfounded fears such as respiratory depression, tolerance, or dependence. When satisfactory alleviation of cancer pain cannot be achieved as a result of regular assessment of the response to analgesics or therapy, opioid-resistant cancer pain should be assessed. Opioid-resistant cancer pain includes underdosing, poor absorption or intake of opioids, raised intracranial pressure, and neuropathic pain. In cases of neuropathic pain, adjuvant analgesics such as anticonvulsants or antidepressants should be considered. Both prevention and appropriate interventions for opioid-related adverse effects such as constipation, nausea and vomiting, and drowsiness are one of the key components to continue to treat cancer pain.
Keywords
Cancer painNeuropathic painOpioidPalliative care19.1 Etiology
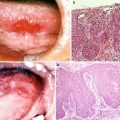
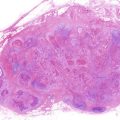
Cancer is the most frequent cause of death (28.5 % of total death) in Japan, and this frequency is gradually increasing. Distressing symptoms are common with progressive life-limiting cancer, especially in their far-advanced stages [1]. Causes for suffering include disease-mediated symptoms such as pain, dyspnea, and fatigue. Moreover, psychological disorders, such as depression, anxiety, and loss of a sense of purpose in living; social demoralization, such as feelings of loss of previously held status and roles within society and family; and the existential or spiritual dimensions of suffering often accompany patients with end-stage diseases. Pain is one of the main and feared symptoms among far-advanced cancer patients (67 %) and also early-stage patients (33 %). Most of them experience continuous pain and almost half patients have severe pain. Causes of cancer pain consist of the cancer itself, complications of the cancer, treatment of the cancer, and comorbidities. The cancer itself makes bone, visceral, or soft tissue involvement, nerve compression or infiltration, muscle spasm, ulceration, raised intracranial pressure. Complications of the cancer involve pressure sores, constipation, postherpetic neuralgia, candidiasis, and lymphedema. The treatment of cancer induces neuropathy caused by chemotherapy, mucositis caused by radiotherapy, and surgery-related issues such as postoperative pain. Comorbidities, which are shown in approximately 30 % of the patients, include non-cancer pain caused by decubitus or back pain, diabetic neuropathy, arthritis, and angina. The experience of pain can exacerbate physical conditions, depression, and anxiety, inducing the prevention of work and reduction of income.
19.2 Definition of Palliative Care
World Health Organization (WHO) has shown the definition of palliative care that it is an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychological, and spiritual [2]. Pain includes not only physical but also psychological, social, and spiritual aspects; therefore palliative care integrates these four big issues. General palliative care is provided by the usual professional cares of the patient and family with low to moderate complexity of palliative care need. Specialist palliative care is provided for patients and their families with moderate to high complexity of palliative care need. Palliative care team offers a support to help patients live as actively as possible until death and the family cope during the patient’s illness and in their own bereavement. Palliative care team consists of physicians to treat physical pain, psychologists, certified nurse in palliative care, pharmacists, nutritionists, and social workers and performs a team approach.
Palliative care was thought to be equal to the terminal care or end-of-life care. When the progressive state of the disease have not been able to regulate following the completion of appropriate anti-cancer treatments, the physicians have decided frequently to change the strategies from disease modifying treatment to supportive care or terminal care. Therefore, palliative care has traditionally been delivered to patients late in the course of the disease. However, late referrals to palliative care are inadequate to alter the quality and delivery of care provided to patients with cancer. To have a meaningful effect on patients’ quality of life and end-of-life care, the current definition has changed that palliative care should be applied early in the course of illness, if applicable, in conjunction with other therapies that are intended to prolong life, such as chemotherapy or radiation (Fig. 19.1). As results of early initiation of palliative care, cancer survival days were reported to be prolonged. Temel et al. have shown that early palliative care led to significant improvements in both quality of life and mood among patients with metastatic non-small-cell lung cancer [3]. Survival rates in the early palliative care group were increased by approximately 3 months compared to that in the standard care group.
Fig. 19.1
Changes in the concept regarding palliative care model
19.3 Physiology
Cancer pain is traditionally classified by either the origin or the location. Nociceptive, neuropathic, psychogenic, and mixed pain is usually used for the classification identified on the basis of the mechanism by which pain is produced. Somatic, visceral, or central pain is another definition classified by the location. Nociceptive cancer pain may result from the activation of the nociceptive receptor following damage to normal tissue or visceral structures. Neuropathic cancer pain is caused by a lesion or disease of the somatosensory nervous system. The underlying mechanisms of neuropathic pain are not understood fully, but it is recognized that pain occurs following reaction of the injured nerves abnormally. Patients may describe having a dull ache with a burning, shooting, or electric shock-like sensations. Psychogenic cancer pain is derived from psychological cause which is not accompanied with explicit physiological diseases.
Somatic cancer pain includes superficial and deep pain. The site of pain is usually localized or well recognized, and the proportion of pain is expressed as aching, throbbing, or tingling. Breakthrough pain is characterized as sudden onset, usually perceived by mobilization or coughing. Visceral cancer pain is caused by the irritation of the pleura or peritoneum and sudden contraction of luminal organs. The site of pain is often poorly localized, and the proportion of pain is described as gnawing or cramping pain.
19.4 Assessment of Pain
Pain assessment is a start point to treat pain. Therefore, failure to assess pain is a critical barrier to better pain management. Principles of pain assessment are follows: to begin with wide open questions before focusing on more specific problems, to watch the patient for clues regarding pain, and to avoid jumping to conclusions.
For pain assessment, it is important to obtain not only the onset, duration, location, quality, pattern, character, and intensity of pain but also aggravating and relieving factors, associated symptoms and signs, and current pain management agents and their effectiveness. Because pain intensity is dependent on each subject, patient self-report is the only gold standard for its assessment. As previously described, many patients have more than one type of pain, it is important that each pain should be assessed separately, and pain should be assessed at appropriate intervals. For example, both pain at rest and pain on mobilization or coughing should be assessed continuously and separately, and pain intensity for the previous 24 h should be evaluated every day following the initiation of treatment in order to change pain management regimen.
Unidimensional tools such as visual analogue scales, verbal rating scales, face scales, and numeric rating scales are employed to obtain information regarding the intensity of the pain experienced by the patient.
19.5 Principles of Pain Management [4]
Following obtaining patient pain information, identification of the patient’s goals of treatment is necessary before the initiation of pain treatment. In 1986, the WHO published the book entitled Cancer Pain Relief and proposed the principles of cancer pain management. To treat cancer pain, these principles can be summarized in five steps (by the mouth, by the clock, by the ladder, for the individual, and attention to detail). By the mouth recommends the oral route in taking drugs into the body. But, in cases of oral cancer, the oral route may not be preferred, because of an inability to take drugs orally due to the invasion of cancer and its related treatments. By the clock indicates the necessity to administer analgesics at regular intervals and not as needed. For example, when slow-release morphine is prescribed after meals three times a day, the interval between dinner and breakfast may be more than 12 h, although the interval between breakfast and lunch would be only 5–6 h. The use of WHO ladder is a key component to treat cancer pain, which demonstrates the treatment process to select analgesics (Fig. 19.2). The analgesics should be selected based on an assessment of the intensity of pain experienced by the patient rather than physicians’ clinical experiences. For the individual indicates analgesics needed by each patient vary widely which is independent on an etiology of pain. In any cases, it is important to assess regularly to confirm not only the response to analgesics or therapy but also the maximum benefit with as few adverse effects as possible. Attention to detail expresses to ensure the patient’s new treatment-induced pain such as opioid adverse events.