Palliation
INTRODUCTION
Radiation therapy (RT) can be a highly effective tool for the treatment of symptoms caused by progressive gynecologic cancers. Common indications for palliative treatment of gynecologic cancers include the following:
Pain caused by erosive lesions involving the primary tumor site or lymph nodes
Vaginal bleeding
Symptomatic systemic metastases
This chapter focuses on the first two of these indications. Palliative treatment of symptomatic systemic metastases is similar for gynecologic cancers and other cancers.
In most cases, the decision to recommend radiation therapy is based primarily on the location of the lesion and the associated symptoms rather than the histology of the tumor. Gynecologic carcinomas, with rare exceptions, are more likely to respond to radiation therapy than to systemic chemotherapy. As a result, radiation therapy is often the palliative treatment of choice in patients with incurable gynecologic cancers. In general, palliative treatment fields should cover the disease that is causing symptoms but do not include elective nodal regions. The use of smaller fields minimizes acute toxic effects and preserves marrow function to improve tolerance of future chemotherapy regimens.
Palliative radiation therapy is frequently given to patients who also require systemic chemotherapy for metastatic disease. Integration of these treatments requires consideration of many factors:
The severity of the symptom.
The nature of the symptom. Debilitating bleeding, pain, or neurologic compromise should be addressed first with radiation since radiation will produce the most rapid response in nearly all cases.
The likelihood of a response to chemotherapy. In patients with less severe symptoms and highly chemosensitive disease, such as small cell carcinoma, initial chemotherapy is preferred since chemotherapy will address all sites of metastatic disease.
The overall extent of the patient’s disease. Systemic therapy may be a higher priority for patients with extensive metastatic disease. Often, a short break is recommended between the completion of radiation therapy and the start of chemotherapy. The delay in starting chemotherapy can be a concern for patients and physicians. The use of hypofractionated regimens can reduce this delay.
INDICATIONS FOR PALLIATIVE RADIATION THERAPY
Vaginal Masses
For patients with recurrence in the vagina as well as distant metastasis, palliative radiation therapy can reduce vaginal bleeding and pain. Treatment fields should cover the involved region of the vagina with a 2- to 3-cm margin. Because the vaginal apex can move 2 cm or more with bladder filling, it is useful to assess vaginal motion by performing simulation both when the patient has a full bladder and when the patient has an empty bladder so that treatment fields can be designed to ensure that the tumor remains in the treatment field without unnecessary irradiation of normal tissues. Intracavitary vaginal brachytherapy may be useful for palliative treatment of very superficial
lesions but generally does not deliver an adequate dose for lesions thicker than 5 mm. For patients who have small volume metastatic disease combined with vaginal recurrence, a short course of palliative external beam therapy with brachytherapy can provide high rates of local control (Fig. 16.1). In general, we do not recommend treatment of lymph nodes in patients with minimal metastatic disease and recurrence at the vaginal apex unless an adjacent node is causing pain or is large and thought likely to cause pain in the near future.
lesions but generally does not deliver an adequate dose for lesions thicker than 5 mm. For patients who have small volume metastatic disease combined with vaginal recurrence, a short course of palliative external beam therapy with brachytherapy can provide high rates of local control (Fig. 16.1). In general, we do not recommend treatment of lymph nodes in patients with minimal metastatic disease and recurrence at the vaginal apex unless an adjacent node is causing pain or is large and thought likely to cause pain in the near future.
Cervical or Uterine Cancer with Metastasis at Presentation
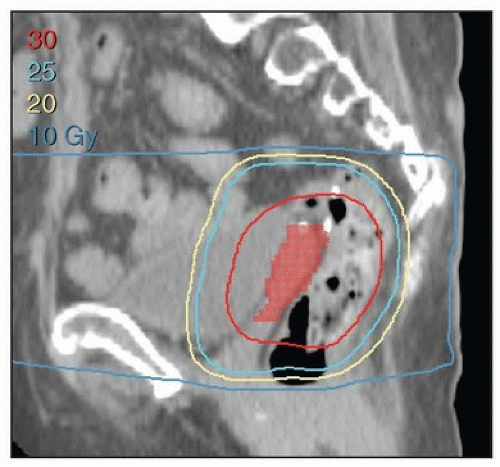
Patients who present with metastatic cervical or uterine cancer frequently suffer from pain and bleeding from the primary cancer. If the patient has an estimated life expectancy of 6 months or more, it may be appropriate to deliver aggressive palliative radiation therapy to the cervix in hopes of providing durable local control in the pelvis. One regimen that we have used in patients with an initial presentation of metastatic cervical cancer is to treat the pelvis to 30 Gy in 10 fractions with concurrent cisplatin and then use brachytherapy to deliver an EqD2 of ˜30 Gy to point A or to 90% of the high-risk clinical target volume. For patients who have massive disease or a short life expectancy, hypofractionated external beam RT can be very effective, with 50% to 100% of patients experiencing marked improvement in symptoms of bleeding and pain.1 Kim et al. reported high rates of response with minimal toxicity with this approach.2
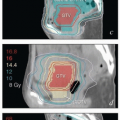
A variety of alternative dose and fractionation schemes have been reported for palliation of pelvic tumors. The Radiation Therapy Oncology Group reported an analysis of patients treated on a prospective study delivering 3.7-Gy fractions twice a day for 2 days (total of 14.8 Gy) repeated every 2 to 4 weeks up to a maximum of 44.4 Gy. Among 61 cervical cancer patients treated, 53% had an objective response to this regimen, and only 7% experienced late toxic effects.3 Treatment with single large fractions can be effective for patients with a poor performance status and poor prognosis. A single 10-Gy fraction provides rapid palliation and can be repeated in a month for patients with persistent symptoms (Fig. 16.2). This regimen results in cessation or substantial reduction in bleeding in ˜75% of patients and elimination or a substantial reduction in pain in ˜50% of patients.1 Our current practice for patients with a poor performance status, defined as a Karnofsky performance status score of 60 or less, is to deliver one 8- to 10-Gy treatment with a conformal plan that excludes as much bowel as possible. If the patient continues to have symptoms a month later, resimulation and treatment with an additional 8 to 10 Gy is considered. This treatment is generally well tolerated; however, retrospective studies of early MD Anderson experience demonstrated that the use of more than two treatments of 10 Gy had an unacceptable rate of major complications.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree