Chapter 43 Pain Management and Antiemetic Therapy in Hematologic Disorders
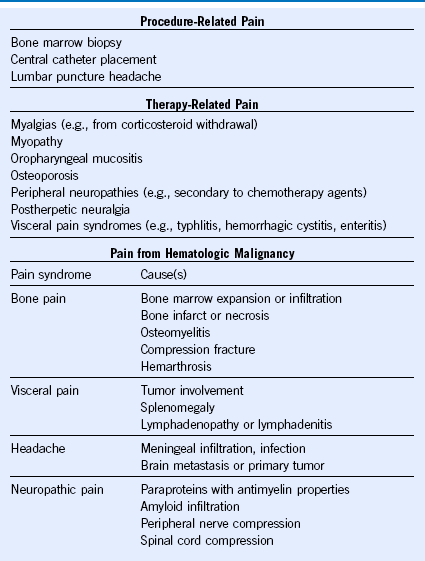
Table 43-2 Classification of Pain Syndromes in Sickle Cell Disease
Adapted from Ballas SK. Pain management of sickle cell disease. Hematol Oncol Clin North Am 19:785, 2005.
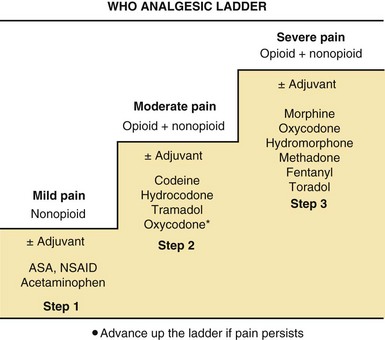
Figure 43-1 STRATEGY FOR PHARMACOLOGIC MANAGEMENT OF PAIN USING THE WORLD HEALTH ORGANIZATION (WHO) ANALGESIC LADDER.