Obesity and Physical Activity
Yani Lu
Jessica Clague
Leslie Bernstein
INTRODUCTION
Evidence showing that physical activity is associated with decreased cancer risk and that obesity is associated with increased cancer risk at certain sites is rapidly accumulating. It is not yet known whether these two factors are interrelated or independent. Physical activity may act to decrease cancer risk primarily by preventing weight gain and obesity. However, physical activity may also have independent effects on cancer risk. In this chapter, we present a summary of the current epidemiologic literature on the possible associations between physical activity and obesity and risk of cancer at several organ sites.
Physical activity is defined as any movement of the body that results in energy expenditure. In this chapter, we focus on recreational physical activity, also called leisure-time physical activity or exercise, and occupational physical activity, including household activity.1 Occupational physical activity typically occurs over a longer period of time and generally requires less energy expenditure per hour than bouts of strenuous or moderate recreational physical activity. The distinction between recreational and occupational activity is important because increasing mechanization and technologic advances have led to decreased occupational physical activity in developed areas of the world, perhaps contributing to a decrease in overall physical activity.
Obesity is defined as the condition of being extremely overweight. In epidemiologic studies, the usual, but not necessarily the best, measure of body mass in adults is Quetelet’s Index, or body mass index (BMI), which is measured as weight in kilograms (kg) divided by the square of height in meters (m2). In the year spanning 2009 to 2010, the prevalence of obesity, defined by having a BMI of 30 kg/m2 or greater, in the US population was 35.5% for adult men and 35.8% for adult women.2 Physical inactivity has likely contributed to the high prevalence of obesity in the United States; data from the 2003 to 2004 National Health and Nutritional Examination Survey, a cross-sectional study of a sample of the civilian, noninstitutionalized population of the United States, has indicated that less than 5% of US adults achieve 30 minutes per day of physical activity, and that men are more physically active than women.3
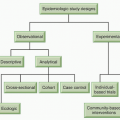
Epidemiologic evidence on the associations of physical activity and obesity with cancer come from observational studies, including cohort studies, which follow populations forward in time after collecting exposure information, and case-control studies, which optimally identify a population-based series of newly diagnosed cases and healthy control subjects, collecting information retrospectively on exposures. In both study designs, physical activity information is usually self-reported and measures vary substantially with respect to timing and level of detail. Studies have measured lifetime or long-term physical activity, activity at defined ages or time points in life, and/or current or recent activity. Ideally, a study would capture activity by type (recreational, occupational, or other, such as an activity related to transportation), duration (minutes per session), frequency (sessions per day), and intensity (low, moderate, or strenuous as defined by examples of activity types) across the lifetime. These studies have often measured height and weight by self-report at one time point, such as at the time of study entry. Some studies have collected other or more detailed anthropometric information, such as waist circumference, hip circumference, or weight at an additional time point like at age 18. Anthropometrics are directly measured by trained study personnel in only a few studies.
Epidemiologic evidence for a role of physical activity or obesity in relation to cancer risk exists for cancers of the breast, colon, endometrium, esophagus, kidney, and pancreatic cancer. Evidence is accumulating to link at least one of these “exposures” to the incidence of gallbladder cancer, non-Hodgkin lymphoma (NHL), and advanced prostate cancer. The evidence for an association between either physical activity or obesity and lung and ovarian cancer is inconclusive.
In addition to specific biologic mechanisms pertinent to physical activity or to obesity at each specific organ site, several global mechanisms have been implicated in both relationships across a number of these organ sites. The steroid hormone and insulin/insulin-like growth factor (IGF) pathways are two such global mechanisms hypothesized to be involved in the links between physical activity or obesity and cancer.4 The role of steroid hormones as a mediator in these relationships is perhaps best understood in the context of breast cancer and endometrial cancer, and will be discussed in those sections. The roles of the insulin and IGF pathways have been discussed in depth with respect to colon cancer and, thus, will be presented in that context. Other global mechanisms have been proposed that have more generalized anticancer impacts and may explain associations between physical activity and several cancer sites; these include heightening immune surveillance, reducing inflammation, increasing insulin sensitivity, controlling growth factor production and activation, decreasing obesity and central adiposity, optimizing DNA repair capacity, and reducing oxidative stress.5,6 Further, obesity has been shown to produce a proinflammatory state and, thus, inflammation may mediate the relationship between obesity and cancer risk.7 It is highly plausible that several of these mechanisms act simultaneously and that they interact synergistically to mediate the associations between physical activity, obesity, and cancer.
BREAST CANCER
Low level of physical activity is an established breast cancer risk factor among postmenopausal women and, to a lesser extent, premenopausal women.4,8,9 The evidence for an association between physical activity and breast cancer has been classified as convincing, with a 20% to 40% reduced risk among physically active women.10 Obesity appears to have a paradoxical relationship with breast cancer risk in that it is an established breast cancer risk factor among postmenopausal women, but may offer some protection for breast cancer among premenopausal women.4
The epidemiologic literature has shown with relative consistency that breast cancer risk is reduced by increasing one’s amount of physical activity.4,8,9,11,12,13 One of the earliest studies, a case-control study of women age 40 years or younger, showed a dramatic reduction in risk of approximately 50% among women who averaged about 4 hours of activity per week during their
reproductive years.14 Similarly, among postmenopausal women, those with higher levels of recreational physical activity during their lifetimes have been shown to have lower breast cancer risk.15 A meta-analysis of 29 case-control studies and 19 cohort studies published between 1994 and 2006 provided strong evidence for an inverse association between physical activity and risk of breast cancer, citing that the evidence for an association between physical activity and premenopausal breast cancer was not as strong as that for postmenopausal breast cancer.8 The conclusion of the meta-analysis was that each additional hour of physical activity per week decreases breast cancer by approximately 6%.
reproductive years.14 Similarly, among postmenopausal women, those with higher levels of recreational physical activity during their lifetimes have been shown to have lower breast cancer risk.15 A meta-analysis of 29 case-control studies and 19 cohort studies published between 1994 and 2006 provided strong evidence for an inverse association between physical activity and risk of breast cancer, citing that the evidence for an association between physical activity and premenopausal breast cancer was not as strong as that for postmenopausal breast cancer.8 The conclusion of the meta-analysis was that each additional hour of physical activity per week decreases breast cancer by approximately 6%.
Epidemiologists require that a risk factor demonstrate consistency across populations before considering it as accepted. Recently, studies have been published on the association between physical activity and breast cancer risk among Japanese,16 Chinese,17 Mexican,18 Tunisian,19 and African American women.20 All studies showed a decreased risk of breast cancer with increasing physical activity. Interestingly, both Suzuki et al.17 and Pronk et al.21 observed the strongest associations among “heavier” women (BMI ≥25 kg/m2 and 23.73 kg/m2, respectively). In the California Teachers Study (CTS), a prospective cohort study of over 133,000 female public school professionals, a variable combining strenuous and moderate long-term recreational physical activity was associated with a reduced risk of estrogen receptor (ER)-negative but not ER-positive invasive breast cancer.11 On the contrary, the Women’s Health Initiative (WHI) observed decreases in breast cancer risk associated with recreational physical activity among postmenopausal women with ER-positive breast cancer and triple negative breast cancer, with only results for ER-positive breast cancer demonstrating a 15% statistically significant reduced risk (when comparing the highest versus lowest tertile of moderate-intensity physical activity).22 Similar but not statistically significant results were observed for strenuous recreational physical activity.22 A major limitation to this and previous studies stratifying by hormone receptor status is the inability to comprehensively classify triple negative breast cancer due to missing HER2 status (unknown in 40% of cases in the WHI study). The use of hormone therapy did not alter the inverse association between recreational physical activity and invasive breast cancer in the Women’s Contraceptive and Reproductive Experiences (CARE) Study.23 Most recently, in the American Cancer Society Cancer Prevention Study II Nutrition Cohort, it was observed that postmenopausal women who engage in at least 7 hours of walking over the course of a week had a modest decreased risk of breast cancer, even in the absence of more vigorous exercise.24 Further, this association did not differ by ER status, BMI, adult weight gain, postmenopausal hormone therapy use, or time spent sitting.24
Lastly, whether physical activity reduces breast cancer risk by impacting preinvasive disease has been studied by assessing the associations with in situ breast cancer and benign breast disease. In the CTS cohort, increasing levels of long-term strenuous recreational physical activity were associated with a decreasing risk of in situ breast cancer.11 Furthermore, a report from the Nurses’ Health Study II cohort showed that lifetime recreational physical activity was associated with a decreased risk of benign breast disease and columnar cell lesions, which may be precursors to breast cancer.25 In summary, epidemiologic studies investigating the association between physical activity and breast cancer risk have produced relatively consistent results showing a reduction in breast cancer risk with increasing level of physical activity. Results to date suggest that moderate-to-strenuous activity may be required for the effect between physical activity and breast cancer risk to be clear; however, clarification of other key details, such as the importance of timing and intensity of activity or variation in effects by tumor characteristics, is pending.
Adult obesity and adult weight gain have both been associated with increased breast cancer risk among postmenopausal women, especially among women who were not current users of menopausal hormone therapy.4,26,27 Most studies among postmenopausal women show a 1.5- to 2-fold increase in risk of invasive breast cancer when comparing the most obese women or those with the largest weight gain to normal-weight women (BMI: 18.5 to 24.9 kg/m2) or those with the least weight gain.4 Paradoxically, overweight or obese premenopausal women have a slightly decreased risk of breast cancer compared with normal-weight or thinner women. Whether larger waist circumference is more important than BMI has been studied in order to separate overall weight gain from abdominal obesity (i.e., visceral fat, which is one element of metabolic syndrome); however, most studies have reported a null association between waist circumference, used as a surrogate for visceral fat, and risk of postmenopausal breast cancer after adjustment for BMI.26 In contrast to the results for postmenopausal women, waist circumference and a positive association with premenopausal breast cancer was found after adjustment for BMI.26 A recent analysis of the Nurses’ Health Study suggests that self-rated body fatness during youth and BMI at age 18 years are both inversely associated with breast cancer risk, with similar results for premenopausal and postmenopausal breast cancer.28
Hormones are central to the discussion of biologic mechanisms linking both physical activity and obesity with breast cancer risk. Physical activity can alter menstrual cycle patterns in premenopausal women, and hormone profiles in both premenopausal and postmenopausal women. Physical activity may lower body fat among children,29 which in turn may delay age at menarche.30 Later age at menarche has been associated with reduced breast cancer risk.31 Physical activity may reduce the frequency of ovulatory cycles.32 Having less frequent and therefore fewer cumulative ovulatory cycles is likely to reduce the lifetime exposure of the breast to endogenous ovarian hormones,31 which are proven proliferative agents.33 Physical activity also can have a direct impact on circulating estrogen levels among postmenopausal women.34
In the postmenopausal period, adipose tissue is the primary source of endogenous hormones via aromatization of androstenedione to estrone.35 Thus, heavier postmenopausal women have higher levels of circulating estrogen than women with less adipose tissue. The involvement of estrogen in the relationship between obesity and breast cancer risk is supported by the observation that obesity does not independently increase breast cancer risk among menopausal hormone therapy users27; the obesity-related increase in estrogen over that provided by exogenous estrogens is negligible. The breast tissue of overweight or obese perimenopausal and postmenopausal women with relatively high risk of breast cancer has been shown to have cytologic abnormalities and higher epithelial cell counts than that of normal-weight women.36 In contrast, obese premenopausal women experience menstrual cycle disturbances, including anovulatory cycles and secondary amenorrhea, thereby lowering their cumulative exposure to estradiol and progesterone.31 A possible explanation for the inverse association between youth body fatness and breast cancer risk is that youth body size is inversely associated with adult IGF-1 levels.28
COLON AND RECTAL CANCER
An inverse association between physical activity and colon cancer risk has been consistently observed among epidemiologic studies; however, the evidence for rectal cancer remains inconclusive. Historically, comprehensive reviews have estimated that physical activity may reduce colon cancer risk by 20% to 25% when comparing individuals with the highest levels to those with the lowest levels of activity.41 Risk reductions are greater for case-control studies (24%) than for cohort studies (17%), and risk reductions for occupational activity (22%) and recreational activity (23%) are similar.41 In cohort studies, colon cancer risk reduction associated with physical activity is greater for men than for women, which
may be due to the influence of hormone therapy on colon cancer risk,42 although case-control studies suggest similar benefits for men and women.43
may be due to the influence of hormone therapy on colon cancer risk,42 although case-control studies suggest similar benefits for men and women.43
Whether physical activity preferentially protects against proximal or distal colon cancer is of interest. A meta-analysis including 21 cohort and case-control studies that examined associations between physical activity and the risks of proximal colon and distal colon cancers produced results suggesting that physical activity is associated with a reduced risk of both proximal colon and distal colon cancers, and that the magnitude of the association does not differ by subsite.44
Although the majority of previous studies have not found an association between physical activity and rectal cancer,41 the National Institutes of Health (NIH)-AARP Diet and Health Study observed a modest reduction in rectal cancer risk for men but not for women after 6.9 years of follow-up.45 Further, in a case-control study conducted in Australia, rectal cancer risk was reduced among men but not among women who participated in vigorous recreational physical activity averaging at least 6 metabolic equivalent task (MET)-hours per week during their adult years.46
An emphasis has been made on trying to identify risk factors for colon adenomas, which are considered precursor lesions for colon cancer; these are detected and removed during colonoscopy or sigmoidoscopy. Wolin et al. conducted a meta-analysis of 20 studies published through April 2010 that investigated the association between recreational physical activity and colon adenomas.47 Adenoma risk was reduced by 19% among men and by 13% among women and, when combining men and women, the inverse association with physical activity was strongest for large/advanced polyps.
Obesity is an established risk factor for colon cancer in both men and women, although the relative risks for men have been higher than those for women.4,26 The adverse impact of being overweight or obese on colon cancer risk is stronger for distal than for proximal colon cancers. In addition, visceral adiposity appears to confer greater risk than general adiposity.26 In the European Prospective Investigation into Cancer and Nutrition (EPIC) study, abdominal obesity as well as adult weight gain were strongly associated with colon cancer risk in both men and women.48,49 No association between these adiposity measures and colon cancer risk was evident among postmenopausal women who had used menopausal hormone therapy, and no association was observed between any measure of adiposity and rectal cancer risk.48 The positive association between obesity and risk of colon cancer was further supported by the findings that both general obesity and abdominal obesity increase the risk of colon adenomas47 with one study of women indicating that the distal colon is the main target site.50 Given that a higher BMI and lack of physical activity are both
risk factors for colon cancer, several statistical approaches have been employed to tease apart their joint and independent effects on colon cancer risk. In the Netherlands Cohort Study,51 colorectal cancer risk was increased at each subsite among larger women in the lowest recreational activity category (<30 minutes per day) than in smaller women in the highest recreational activity category (>90 minutes per day); however, the interaction between physical activity and body size was statistically significant only for proximal tumors. Using different fatness measures for men, the only similar finding was that men with low levels of physical activity whose trouser size was below the median of that for the cohort had an increased risk of distal colon cancer; no differences in risk were noted for other subsites or for men with larger trouser sizes.51 The mechanisms explaining the relationship between physical
activity and colon cancer are not clearly established, but include the impact on insulin sensitivity and IGF profiles, and inflammation, as well as some colon-specific mechanisms. Physical activity may stimulate stool transit in the colon, thereby decreasing the exposure of colonic mucosa to carcinogens in the stool.6 Alternatively, physical activity-induced decreases in prostaglandin E2 may decrease colonic cell proliferation rates and increase colonic motility.6 In addition to steroid hormones, which have been clearly implicated as biologic modifiers of the effect of physical activity and obesity on colon cancer risk, the insulin and IGF pathways may mediate the associations between these exposures and colon cancer risk. For obesity in particular, the link can be inferred because obesity can lead to insulin resistance,52 a syndrome characterized by high circulating insulin levels. High insulin levels appear to promote cell proliferation and tumor growth in the colon7 and may also suppress the expression of IGF-binding proteins 1 and 2, leading to increased bioavailable IGF-1 levels.53 Another possible mechanism is obesity-enhanced inflammation in which increases in adipose tissue macrophages lead to the secretion of inflammatory cytokines associated with colon cancer risk (e.g., tumor necrosis factor [TNF]-α, monocyte chemoattractant protein [MCP]-1, and interleukin [IL]-6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree