Introduction
Non-parkinsonian movement disorders that tend to affect primarily the elderly include chorea, restless legs and periodic leg movements during sleep and while awake, dystonia and tremor (Table 64.1).
Table 64.1 Definition of movement disorders.
| Disorder | Definition |
| Tremor | Rhythmic oscillation typically about a joint, alternating or simultaneous co-contraction of agonist and antagonist muscle groups |
| Chorea | Irregular, non-stereotypical quick jerks, randomly distributed |
| Dystonia | Sustained abnormal postures, often with a twisting character, sometimes overlying repetitive jerks |
Chorea
Chorea, derived from the Greek word for ‘dance’, is a continuous, random sequence of irregular, unpredictable movements that flit from one body part to another. A variety of choreatic disorders begin during childhood or early adulthood. Those that are important in the elderly include Huntington’s disease (HD), senile chorea and tardive dyskinesia.
Huntington’s Disease
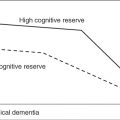
HD is an autosomal dominant neurodegenerative disorder characterized by abnormal involuntary movements, progressive dementia and psychiatric manifestations. In 1993, the specific mutation in HD was identified as an expansion of the unstable CAG trinucleotide repeat in the IT15 gene in chromosome 4p (Kremer et al., 1994; Hersch et al., 1994). Individuals with HD have more than 40 CAG repeats. There is an association of age of onset and number of repeats only in the very early and very late-onset HD (Andrew et al., 1993). Juvenile onset cases are associated with repeat lengths greater than 52 and paternal transmission. This preponderance of paternal transmission has been reported for cases with onset before age 21 and is due to CAG repeat length expansion during spermatogenesis (Hersch et al., 1994). Early onset is associated with the rigid type or Westphal variant of HD. In contrast, late-onset HD, defined as onset at age 50 or later, is associated with less than 42 repeats. Although it is believed that individuals with repeat lengths of 40 and 41 may not exhibit symptoms in their lifetime, it is unclear whether this is due to decreased penetrance among carriers with such lower repeat sizes or the mere fact that they did not live long enough. Approximately 1–2% of at-risk individuals screened for HD will have repeat lengths between 36 and 39. It is difficult to predict which of these individuals will develop symptoms of HD within a normal lifespan (Myers et al., 1998).
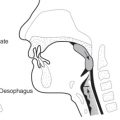
HD has a subtle, insidious onset in the third and fourth decades of life and gradually worsens over a course of 10–20 years until death. Clinically, the disease usually presents with an involuntary movement disorder characterized by chorea, dystonia, bradykinesia, incoordination and impaired postural reflexes. Oculomotor dysfunction is a frequent early sign and is characterized by slowed, delayed or inaccurate saccades. As HD advances, swallowing and speech may become impaired, eventually disrupting communication and leading to aspiration pneumonias. Intellectual decline or dementia is a uniform feature, although the severity of cognitive impairment varies among patients. Psychiatric features are also common and disabling, appearing as the presenting manifestation in up to one-third of HD patients (Biglan and Shoulson, 2002).
Approximately 25% of persons affected by the disease exhibit initial signs of chorea at age 50 or later, and half of these will not come to medical attention until after age 60. The clinical features of late-onset HD resemble those of midlife onset but the illness is more slowly progressive and less functionally debilitating. In late-onset disease, symptoms may appear to plateau or progress very slowly over several years. The most common symptoms in a series of 25 late-onset cases were mild to moderate chorea and cognitive impairment (100% of cases), dysarthria (88%) and gait disturbance (72%) (Myers et al., 1985). The chorea in late-onset HD often allows the patient to stay at home, with minimal nursing support, to remain ambulatory and to maintain activities of daily living for many years.
Pathology and Pharmacology
Histological studies of HD have demonstrated diffuse brain atrophy with severe neuronal loss and gliosis occurring selectively in the caudate nucleus and putamen. This neuronal loss in the striatum is largely confined to the GABAergic medium-sized spiny neurons that project to the globus pallidus, and which receive glutamergic input from the cortex and dopaminergic input from the substantia nigra. The severity of neuropathological changes was found to be closely related to the age at onset of the illness. An earlier clinical onset is associated with more severe neuropathological involvement, while older onset cases show a slower rate of progression of neuropathological changes (Myers et al., 1988).
The exact mechanisms that lead to the selective neuronal loss in HD are poorly understood. Hypotheses include glutamergic excitotoxicity, mitochondrial bioenergetic dysfunction, apoptosis and transcriptional dysregulation (Biglan and Shoulson, 2002). Huntingtin, the mutant protein product of CAG expansion, undergoes abnormal cleavage in the cytoplasm, resulting in the translocation of the N-terminal fragment in the nucleus and the formation of aggregates in the nucleus. It has been hypothesized that this altered cleavage and subsequent nuclear translocation represent key steps in the pathogenic cascade leading to neuronal dysfunction and cell death (Saudou et al., 1998).
Treatment
Currently, there is no effective treatment to slow or reverse the inexorable progression of HD. Neuroprotective strategies have been explored, including coenzyme Q10, remacemide, minocycline, creatine and Huntington’s disease advocacy centre (HDAC), but none of these agents has been proven to alter the natural history of the disease, under the specific experimental conditions studied (Biglan and Shoulson, 2002). There are, however, several approaches to control the symptoms. Unfortunately, HD research has had a tendency to concentrate on the motor aspects of the disorder, whereas the major problems are behavioural (e.g. dementia, depression, psychosis) and the chorea is often the least relevant in terms of management. Chorea improves with the use of dopamine receptor-blocking agents (e.g. neuroleptics) or dopamine-depleting agents (e.g. reserpine or tetrabenazine). The newer, atypical neuroleptics, especially olanzapine, have become the drugs of choice, when treatment of chorea is needed (Bonelli et al., 2002; Jimenez-Jimenez et al., 2002; Paleacu et al., 2002). More recently, amantadine, an N-methyl-D-aspartate (NMDA) antagonist, has been found to be effective in treating chorea in patients with HD (Verhagen Metman et al., 2002). Management of the associated psychiatric disorders with the appropriate administration of psychotropic drugs should also be considered. Depression is managed with selective serotonin reuptake inhibitors (SSRIs) and mirtazapine, and psychosis and behavioural issues are addressed with atypical antipsychotics (Bonelli et al., 2004). Dementia is unfortunately the most disabling facet of this disorder and is untreatable. In fact, the most effective approach to HD available today is genetic counselling.
Spontaneous Oral Dyskinesia and Senile Chorea
Clinical Features
Gowers, at the end of the nineteenth century, described an isolated form of chorea of late life as an entity separate from HD and neuroleptic use (Critchley, 1931). Isolated spontaneous oral dyskinesia (SOD) in the elderly is a clearly defined and fairly common syndrome but is more often recognized as part of other neurological syndromes such as tardive dyskinesia, Huntington’s chorea, acquired hepatocerebral degeneration and complication of prolonged levodopa therapy in Parkinson’s disease (PD). In some patients, the occurrence of SOD is associated with the edentulous state and the improvement with appropriate dental appliances suggests that the absence of teeth in some individuals causes or makes the clinical syndrome worse (Sutcher et al., 1971). In one study, observation was carried out on 1018 non-institutionalized, frail elderly subjects attending day care centres to document the prevalence of SODs. A total of 38 subjects were suspected to have SODs for a prevalence rate of 3.7% and 31 had probable tardive dyskinesia, for a prevalence rate of 3.0%. In a survey covering medical and dental issues in the same population, subjects with suspected SOD reported more frequent ill-fitting dental devices, oral pain and a lower rate of perception of good oral health compared with non-dyskinetics. Individuals with suspected SOD typically presented with mild stereotyped masticatory or labial movements compared with the more complex phenomenology of probable TD (tardive dyskinesia) cases (Blanchet et al., 2004).
Pathology and Pathophysiology
Recent developments in molecular genetics have provided a reliable test for confirmation of the diagnosis of HD that is highly sensitive and specific. Shinotoh et al. (1994) measured CAG trinucleotide repeat expansion in the Huntington’s gene in four cases of senile chorea, and found that CAG repetition lengths were normal. They considered this evidence that senile chorea exists as a distinct clinical entity that is nosologically separate from HD.
There is a paucity of pathological reports of senile chorea in the literature. Neuropathological cases of senile chorea reported in the past were before the advent of genetic testing for HD and it is possible that many of them represented mild cases of HD and no cognitive changes.
Treatment
Chorea can be ameliorated with neuroleptic agents. Neuroleptic agents should be initiated at low doses and slowly titrated upward to optimal symptom control. Neuroleptic use in this age group is associated with a higher incidence of TD and drug-induced parkinsonism (see Chapter 63, Parkinson’s disease). Thus, the use of newer atypical neuroleptics is preferable. Although the atypical neuroleptics have been advocated to carry a much smaller risk of drug-induced parkinsonism or TD, this has not been the case with some of them. Therefore, physicians should be vigilant for the development of these complications. Amantadine is useful in ameliorating chorea, but it is excreted unchanged in the urine and it can become toxic in elderly people with decreased renal function. Anticholinergic agents and dopamine agonists tend to worsen these movements and should be avoided. Treatment of either senile chorea or SODs is indicated only if the movements are severe enough to cause functional impairment. In edentulous patients, well-fitting dentures may improve the symptoms.
Tardive Dyskinesia
TD is defined as abnormal involuntary movements associated with chronic treatment with dopamine receptor-blocking agents. Neuroleptics are the most frequently implicated drugs, although other agents, for example, metoclopramide, have also been associated with the development of TD (Khot et al., 1992). The diagnosis of TD requires (1) history of at least 3 months total cumulative (continuous or discontinuous) neuroleptic exposure; (2) the presence of at least ‘moderate’ abnormal involuntary movements in one or more body areas or at least ‘mild’ movements in two or more body areas; (3) absence of other causes for the movements (Task Force on late Neurological effects of antipsychotic drugs, 1980). Since the earlier reports of TD, a variety of involuntary movements, in addition to the well known oral–buccal–lingual masticatory movements, have been described, including dystonia, akathisia, tics and myoclonus (Burke, 1992). It has been suggested that the newer, atypical neuroleptics (risperidone, olanzapine, quetiapine, ziprasodone, clozapine) are less likely to cause TD (Jeste, 2004; Dolder and Jeste, 2003). Clozapine and quetiapine are the ones associated with the lowest risk (Tarsy et al., 2002).
The typical movements of TD are choreic in speed and amplitude, but usually tend to be more stereotypic and repetitive and less random or unpredictable than chorea of other a etiologies. The orofacial and lingual muscles tend to be involved earlier and more frequently in TD. The disorder is usually only slowly progressive after initial development, and in many patients, especially the elderly, it does not appear to progress at all and may actually gradually improve with age.
Possible risk factors for TD include advanced age, female gender, affective disorder, mental retardation, brain damage, length of neuroleptic exposure, use of anticholinergic drugs, history of acute extrapyramidal side effects, antidepressant drugs, depot neuroleptics, history of drug interruptions or holidays, elevated serum neuroleptic concentrations and late-onset psychosis (Lohr and Bracha, 1988).
Studies evaluating the prevalence and risk factors for TD have been largely confounded by vague diagnostic criteria, biased study samples, lack of matched control populations and concurrent neuroleptic use, which can mask TD. Overall, most studies suggest that the average prevalence of TD is estimated as 15–20% (Khot et al., 1992). In one series, 45% of patients had relatively persistent symptoms over the course of 5 years, while 24% had a fluctuating course. Only 11% improved, while 7% got worse. Remissions usually appear within 1–2 years after discontinuation of medication, although they may not occur until 5 years after discontinuation of medication (Bergen et al., 1989).
Pathology and Pathophysiology
No characteristic pathological abnormalities have been found in TD. The pathophysiology is not clearly understood. The development of dopamine receptor supersensitivity following chronic dopamine receptor blockade is hypothesized to be the mechanism underlying TD. This would explain why, as the neuroleptic agents are withdrawn and receptor blockade reduced, TD may appear for the first time, or pre-existing TD may worsen. Furthermore, exacerbation of the movements by dopaminergic agonists and improvement with increased dopamine receptor blockade or dopamine depletion support the notion that alterations in dopamine receptors are likely to be involved. As a result of the deficiencies in the dopamine supersensitivity hypothesis, attention has also been focused on other neurotransmitters, such as GABA, norepinephrine, acetylcholine and serotonin (Khot et al., 1992).
Treatment
Once it occurs, TD is frequently difficult to treat. Therefore, only individuals with defined indications for the use of these agents should be treated, especially among the elderly, who appear to be at a higher risk for developing TD. Although it is not proven, the neuroleptic dose should be maintained at the lowest possible and the drug should be used for the shortest period of time allowed by the patient’s psychiatric disease. If the patient’s psychiatric disorder is sufficiently severe to require long-term neuroleptic use, an atypical neuroleptic should be considered.
Several medications have been used in the treatment of persistent TD with variable response. These include dopamine depleters (reserpine or tetrabenazine), noradrenergic antagonists (propranolol, clonidine), γ-aminobutyric acid (GABA) agonists (clonazepam, diazepam, valproate, baclofen), botulinum toxin injections and, to a lesser degree, vitamin E, buspirone and calcium channel blockers, which have been used with variable results (Miyasaki and Lang, 1995). When the predominant movement is chorea, anticholinergic agents may worsen the movements; if, on the other hand, dystonia is the primary characteristic, these agents can be beneficial.
Restless Legs Syndrome and Periodic Limb Movements During Sleep and While Awake
Restless legs syndrome (RLS) is a sensorimotor disorder characterized primarily by motor restlessness, which is brought on by rest and accentuated later in the day and during the early night in those with normal circadian rhythms. The urge to move or unpleasant sensations are partially or totally relieved by movement, such as walking or stretching. The prevalence of RLS is estimated to be 10–15% in the general population. Symptoms often begin before age 20, but usually become severe enough to seek medical attention in the fourth decade (Walters et al., 1996). Periodic limb movement disorder (PLMD) is frequently associated with RLS but may occur independently, especially in the elderly. The prevalence of PLMD increases with advancing age. RLS and PLMD, taken together, are the primary diagnosis in 13.3% of patients complaining of insomnia (see Chapter 54, Sleep apnoea and sleep disorders) and in 6.9% of patients complaining of excessive daytime sleepiness (Montplaisir and Godbout, 1989).
RLS and PLMD have been related to several other medical conditions, including peripheral neuropathy, iron deficiency anaemia and end-stage renal disease (Garcia-Borreguero et al., 2004). Selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants and monoamine oxidase inhibitors can induce or aggravate PLMD, as does withdrawal from anticonvulsants, benzodiazepines and barbiturates. Exacerbations of RLS can occur during pregnancy or with iron deficiency anaemia. Finally, PLMD may accompany other sleep disorders, in particular, sleep apnoea or narcolepsy (Montplaisir and Godbout, 1989).
RLS can be diagnosed by the following four clinical criteria: (1) an urge to move the legs, usually accompanied or caused by uncomfortable and unpleasant sensations in the legs; (2) the urge to move or unpleasant sensations begin or worsen during periods of rest or inactivity such as lying or sitting; (3) the urge to move or unpleasant sensations are partially or totally relieved by movement, such as walking or stretching; (4) the urge to move or unpleasant sensations are worse in the evening or night than during the day or only occur in the evening or night (Hening et al., 2004). Supportive clinical features include a positive family history, positive response to dopaminergic therapy and the presence of periodic limb movements (during wakefulness or sleep) (Hening et al., 2004). Family history of RLS can be found in 40–90% of patients with RLS (Montplaisir et al., 1997; Winkelmann et al., 2000). PLMD occurs in 80% of patients with RLS. The severity of RLS can vary greatly throughout a patient’s lifetime but the disease is typically chronic and the course progressive. The sudden remissions, lasting for months or even years, are as difficult to explain as are the relapses, which appear without any apparent reason.
Periodic limb movements of sleep (PLMS), originally called nocturnal myoclonus, are best described as rhythmic extensions of the big toe and dorsiflexions of the ankle, sometimes with flexions of the knee and hip, each movement lasting 0.5–5.0 s and occurring every 20–40 s. Standard criteria for PLMS include their occurrence in a series of four or more movements spaced by intervals of 5–90 s (onset to onset) with electromyogram (EMG) burst durations of 0.5–5 s that rise to 1/4 of the EMG biocalibration amplitude (Hening et al., 2004). Intense movements may cause numerous arousals, leading to non-restorative sleep. PLMS may be asymptomatic, diagnosed through a bed partner’s report or polysomnogram. PLMS occur primarily in stage 2, non-REM (rapid eye movement) sleep, less often in stages 3 and 4, and infrequently during REM sleep.
Fifty percent of patients with RLS have abnormal involuntary movements while awake, called periodic leg movements during wake (PLMW), formerly called dyskinesias while awake. Like the PLMS, PLMW are discrete, repetitive, stereotyped movements that recur at intervals of seconds, tend to involve primarily the legs and occur almost exclusively at rest and disappear with action. PLMW are longer compared with the leg movements during sleep (shorter than 10 s during wakefulness vs 5 s during sleep).
Differential diagnosis of RLS and PLMS should include hypnic myoclonus, fragmentary myoclonus, painful legs and moving toes syndrome, nocturnal cramps, body jerks induced by long-term administration of levodopa or akathisia. The symptoms of akathisia are prominent throughout the waking hours of the day or night, whereas the symptoms of RLS are more prominent at night. Akathisia patients manifest the external signs of an inner urge to move, whereas patients with RLS move about to relieve the dysesthetic sensations they have in their legs.
Although our understanding of the pathophysiology and genetics of RLS has advanced considerably, there is currently no recognized objective test for the disorder. Standard sleep measures remain useful in terms of sleep initiation, continuity and sufficiency. These are often combined with measures of PLMS. Recently, the suggested immobilization test (SIT) has been proposed as a possible auxiliary measure, examining the ability of a period of imposed rest to induce subjective and motoric features of RLS. A combination of the SIT conducted in the evening with measurement of sensory discomfort and the presence of frequent PLM during awake epochs of the standard polysomnography (PSG) can provide a high degree of diagnostic accuracy (sensitivity of 82% and specificity of 100%) (Hening et al., 2004).
Pathophysiology and Pharmacology
Several lines of evidence suggest that RLS results from dysfunction of the central rather than the peripheral nervous system. RLS improves with centrally acting dopamine agonists, and this effect can be antagonized only by centrally acting and not peripherally acting dopamine antagonists (Garcia-Borreguero et al
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree