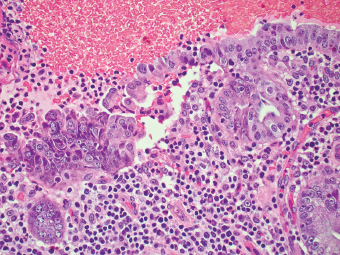
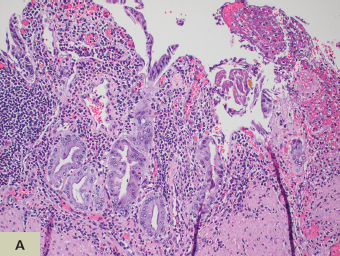
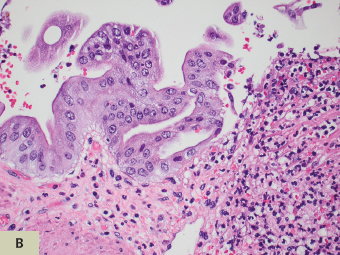
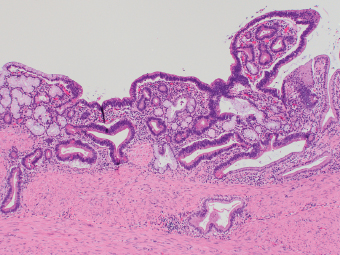
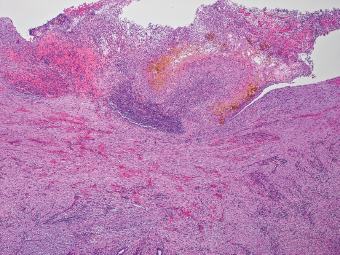
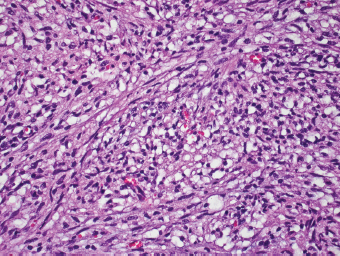
12 Biologic Evolution and Treatment Biologic Evolution and Treatment Biologic Evolution and Treatment The extrahepatic biliary tract, which includes the gallbladder and extrahepatic bile duct, is an excretory ductal system lined by columnar epithelium with underlying smooth muscle layer and perimuscular connective tissue. The latter contains nerves, paraganglia, vessels, and lymphatic channels. Although the histologic variation is more limited than those lesions in the liver, neoplasms and neoplastic mimics can arise from any of the components of the extrahepatic biliary tracts. Many of the neoplastic mimics of the gallbladder are found incidentally during clinical evaluation of cholecystitis or in cholecystectomy specimens. Neoplastic mimics of the gallbladder are generally variations of acute and chronic cholecystitis including porcelain gallbladder and xanthogranulomatous cholecystitis, and lesions associated with chronic cholecystitis such as pyloric gland polyp, cholesterol polyp, adenomyoma, and adenomyomatous hyperplasia (Table 12.1). Other less common neoplastic mimics are inflammatory myofibroblastic tumor and malakoplakia. Due to the nature of excretory ductal system of extrahepatic bile duct, neoplasms and neoplastic mimics of the extrahepatic bile duct commonly cause symptoms of bile duct obstruction with jaundice and pruritus. In rare instances, heterotopic tissue can be encountered in gallbladder and extrahepatic bile duct. Benign bile duct stricture can occur as a postsurgical complication in cholecystectomy, bile duct/bowel anastomosis, extensive hepatic resection, and liver transplantation, or in inflammatory conditions such as PSC, IgG4-related cholangitis, chronic pancreatitis, and radiotherapy. TABLE 12.1 Neoplastic Mimics and Neoplasm of Gallbladder and Extrahepatic Bile Duct GALLBLADDER EXTRAHEPATIC BILIARY TRACT Inflammatory lesions Acute and chronic cholecystitis Primary sclerosing cholangitis Lymphocytic cholecystitis Autoimmune cholangitis Xanthogranulomatous cholecystitis Inflammatory pseudotumor Malakoplakia Metaplasia, hyperplasia, and polyps Pyloric gland metaplasia/polyp Pyloric gland metaplasia/polyp Intestinal metaplasia Cholesterol polyp Fibrous polyp Papillary hyperplasia Heterotopia and developmental anomalies Pancreas heterotopia Pancreas heterotopia Gastric heterotopia Duplication Postsurgical lesions Biloma Bile duct strictures Residual calculi Amputation/traumatic neuroma Acute and chronic cholecystitis can result in a large, firm, or thickened gallbladder, which often mimics a neoplastic process. Acute cholecystitis may be identified by edema, hemorrhage, friability, and/or gangrenous necrosis of the gallbladder wall, whereas chronic cholecystitis is characterized by chronic inflammation and fibrosis of the gallbladder mucosa and wall, often with the formation of Rokitansky-Aschoff sinuses. Extensive calcification of the gallbladder wall in chronic cholecystitis is referred to as porcelain gallbladder, which is associated with a high frequency of gallbladder carcinomas (535) and requires extensive sampling of the gallbladder to exclude malignancy. Ulceration or denudation of the mucosa is a common finding in both acute and chronic cholecystitis, which often results in reactive or regenerative atypia and the distinction from a neoplastic or dysplastic process can be difficult (Figures 12.1–12.3). In contrast to dysplastic cells, cells with regenerative atypia maintain their low nuclear-to-cytoplasmic ratio, with vesicular nuclei and prominent nucleoli, and are p53 negative by immunohistochemistry. Mitotic figures are common. These changes are exaggerated in areas adjacent to ulcers and often admixed with inflammatory infiltrates including scattered neutrophils. FIGURE 12.1 Regenerative atypia in acute cholecystitis often mimics neoplastic epithelium. Ulceration, acute inflammation, and hemorrhage are commonly seen in acute cholecystitis. FIGURE 12.2 In contrast to regenerative atypia, high-grade dysplastic epithelium depicted here shows markedly atypical cells with high nuclear-to-cytoplasmic ratio and nuclear pleomorphism. FIGURE 12.3 Low-grade dysplasia of the gallbladder epithelium resembling low grade adenomatous epithelium of the gastrointestinal tract. Xanthogranulomatous cholecystitis is an uncommon diffuse destructive form of chronic cholecystitis with accumulation of lipid-laden macrophages. It is almost always associated with gallstones and mimics gallbladder carcinoma clinically and on imaging studies. The pathogenesis is uncertain, but an exuberant inflammatory response to extravasated bile, possibly from ruptured Rokitansky-Aschoff sinuses or mucosal ulceration, is likely. Xanthogranulomatous cholecystitis occurs in less than 2% of cholecystectomy specimens (536). The symptoms are indistinguishable from other forms of chronic cholecystitis. Some patients may present with a clinical picture of acute cholecystitis. It can be associated with elevation of CA19-9 and DUPAN-2 serum level in the absence of biliary tract malignancy (537,538). Imaging studies demonstrate a thickened wall of the gallbladder and gallstones are found in almost all patients. Because of the thickening of the wall of the gallbladder, and, on occasion, extension to the adjacent organ, it often mimics gallbladder carcinoma on presentation (539,540). The gallbladder is markedly enlarged and firm. Focal areas of necrosis or hemorrhage can be seen. The lumen almost always contains gallstones. The mucosa is ulcerated mucosa and can be severely fibrotic (Figure 12.4). The cut surface of the wall is tan-yellow and firm, often indistinguishable from gallbladder adenocarcinoma; therefore, careful examination and extensive sampling should be performed. Microscopically, the histologic features can be variegated with collection of lipidladen macrophages, plasma cells, lymphocytes, eosinophils, in the background of extensive fibrosis. The macrophages may also contain ceroid pigment in areas (Figure 12.5). Cellular areas of fibroblastic proliferation can occur (Figure 12.6). Cholesterol clefts, foreign body giant cells, and lymphoid follicles are often present. The extent of involvement can be variable throughout the gallbladder. FIGURE 12.4 The wall of gallbladder in xanthogranulomatous cholecystitis is thickened and fibrotic. Bile concretion is noted at the ulcerated gallbladder mucosa. FIGURE 12.5 Accumulation of ceroid-laden macrophages admixed with chronic inflammatory in xanthogranulomatous cholecystitis. FIGURE 12.6
Neoplastic Mimics of the Gallbladder and Biliary Tree
 ACUTE AND CHRONIC CHOLECYSTITIS
ACUTE AND CHRONIC CHOLECYSTITIS
 XANTHOGRANULOMATOUS CHOLECYSTITIS
XANTHOGRANULOMATOUS CHOLECYSTITIS
 ADENOMYOMATOUS HYPERPLASIA AND ADENOMYOMA
ADENOMYOMATOUS HYPERPLASIA AND ADENOMYOMA
 PRIMARY SCLEROSING CHOLANGITIS
PRIMARY SCLEROSING CHOLANGITIS
 IgG4-RELATED SCLEROSING CHOLANGITIS
IgG4-RELATED SCLEROSING CHOLANGITIS
 POSTSURGICAL NEOPLASTIC MIMICS
POSTSURGICAL NEOPLASTIC MIMICS
INTRODUCTION
ACUTE AND CHRONIC CHOLECYSTITIS
XANTHOGRANULOMATOUS CHOLECYSTITIS
 CLINICAL FEATURES
CLINICAL FEATURES
 HISTOLOGIC FEATURES
HISTOLOGIC FEATURES

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree