| Syndrome/disease | Organism | Symptoms, signs, and neurologic findings | CNS | PNS | Cord | Other findings | Risk factors |
|---|---|---|---|---|---|---|---|
| Anterior polio myelitis syndrome | Poliovirus 1, 2, 3 | Onset: Acute Clinical patterns: Spinal and bulbar paralysis Common features: Asymmetric flaccid paralysis (AFP) | √ | √ | “Minor illness” (3–4 d) influenza-like syndrome “Major illness” (5–7 d) aseptic meningitis, myeloencephalitis | Absence of protective immunity and travel in endemic areas | |
| Nonpolio Coxsackie A, B Echovirus Enterovirus West Nile virus (WNV) | Onset: Acute Clinical patterns: Similar to polio but milder disease Asymptomatic infection: Common except at extremes of age and in immunosuppressed | √ | √ | CNS phase aseptic meningitis, encephalitis, encephalomyelitis | Seasonal incidence in temperate climates (summer), year-round in tropical climates WNV: Vector borne (mosquito) and transmitted by breast milk, blood transfusions, and organ transplants | ||
| Ascending myelitis syndrome (leukomyelitis) | HIV-1 | Onset: Acute/subacute Clinical patterns: | √ | √ | √ | See below | |
| HTLV-1 | Onset: Subacute/chronic Clinical patterns: tropical spastic paraparesis (TSP) or HAM | √ | “Rosette cells” in CSF lymphocytes Coinfection with HIV in IVDUs | Injecting drug use Prior residence in endemic areas | |||
| Herpesviruses: CMV, EBV HSV, VZV | Onset: Acute Clinical patterns: Ascending pattern w/initial plexitis Asymmetric commonly | √ | √ | Primarily seen in immunosuppressed | Related to epidemiology of primary infection | ||
| Herpes B virus (Monkey B) | Onset: Subacute (5–30 d) Clinical pattern: Aseptic meningitis Ascending encephalomyelitis | √ | √ | Prodromal illness: Early (vesicles); Intermediate (numbness, weakness, hiccups) | Macaque monkey bite or exposure to tissues Laboratory workers exposed to contaminated cell cultures | ||
| Transverse myelitis syndrome | Primary myelitis VZV Dengue Spirochetesa Schistosomiasis Post-meningococcal | Onset: Acute (after prodrome) Clinical patterns: Sensory motor level Initial spinal shock Hyperreflexia below level of lesion | √ | Related to epidemiology of primary infection | |||
| Secondary myelitis: Bacteria, fungi, mycobacteria | Onset: Acute/subacute Clinical patterns: Radicular-spinal cord syndrome Cauda equina syndrome | √ | Related to primary infection and organisms | Injecting drug use Hematogenous osteomyelitis Back surgery: Intraoperative contamination | |||
| Acute demyelinating encephalomyelitis (ADEM) | Mycoplasma, Lyme, Enteroviruses, EBV, CMV, VZV, dengue, measles, hepatitis A, Semple Rabies vaccine | Onset: Acute Clinical patterns: Pyramidal and extrapyramidal symptoms, hemiplegia, ataxia, cranial neuropathies, myelitis paresthesias, polyradiculopathy, altered mental status | √ | √ | Related to epidemiology of primary infection |
a Spirochetes include: Borrelia species (B. burgdorferi – Lyme, B. recurrentis – relapsing fever), Leptospira spp., Treponema pallidum.
Abbreviations: CMV = cytomegalovirus; CNS = central nervous system; CSF = cerebrospinal fluid; EBV = Epstein–Barr virus; HAM = HTLV-1-associated myelopathy; HIV = human immunodeficiency virus; HSV = herpes simplex virus; HTLV = human T-cell lymphotropic virus; IDUs = injecting drug users; IVDU = intravenous drug use; PNS = parasympathetic nervous system; VZV = varicella-zoster virus; WNV = West Nile virus.
| Syndrome/disease | Organism/ antibiotic | Symptoms, signs, and neurologic findings | CNS | PNS | Cord | Other findings | Risk factors |
|---|---|---|---|---|---|---|---|
| Polyneuritis: Acute (AIDP) Guillain–Barré Landry Miller-Fisher Chronic (CIDP) | 1. Idiopathic 2. Infection-associated | Onset: Acute/subacute and chronic Common features: Progressive, symmetric weakness Distal→proximal limbs Truncal→cranial muscles Paresthesias, hypotonia, areflexia Clinical patterns: Ascending, descending, bulbar | √ | √ | Variable autonomic dysfunction (ileus, cardiac) | Preceding viral illness or vaccination, prior episode Infection-associated: Viral (EBV, HIV, dengue, hepatitis) Bacterial (Campylobacter) Chlamydia (C. psittaci) Mycoplasma (M. pneumoniae) Spirochetes (Lyme borreliosis) | |
| Neuropathy due to bacterial toxins | Corynebacterium diphtheriae | Onset: Acute/subacute Clinical patterns: Bulbar symptoms Ascending peripheral neuropathy | √ | √ | Pharyngitis with pseudomembrane Myocarditis Endocarditis | Absence of protective immunity, epidemic respiratory diphtheria, contaminated wound | |
| Clostridium botulinum | Onset: Acute/subacute (dose-related) Clinical patterns: Bulbar symptoms Myasthenia-like weakness | √ | √ | Autonomic dysfunction (dry tongue, ileus, urinary retention) Decreased vital capacity | Food sources Contaminated wounds (IDUs) Sinusitis in cocaine snorters | ||
| Clostridium tetani | Onset: Acute/subacute (dose-related) Clinical patterns: Localized, cephalic, generalized | √ | √ | √ | Autonomic dysfunction Hypertensive crises Decreased vital capacity | Absence or loss of protective immunity Puncture/contaminated wounds Infected neonatal cord stumps | |
| Medication Acute Antibacterials | Aminoglycosides Polymyxins | Onset: Acute (concentration-related) Clinical patterns: Neuromuscular blockade | √ | √ | Decreased vital capacity Generalized paralysis | Excessive or unadjusted dosage for lean body mass | |
| Subacute Anti-TB Antiretrovirals Antibacterials | Isoniazid ddI, ddC, d4T Chloramphenicol Metronidazole Nitrofurantoin | Onset: Subacute (dose and duration) Clinical patterns: Symmetric Distal paresthesias and weakness Progressive loss of distal DTRs | √ | Isoniazid: Lack of pyridoxine Nucleoside antiretrovirals: Pre-existing neuropathy Excessive or unadjusted dosage Antibiotics: Cumulative dosage | |||
| Vasculitis | Polyarteritis nodosa (PAN) Wegener’s | Onset: Subacute Clinical patterns: Mononeuritis multiplex Common features: Asymmetric weakness, paresthesias, loss of DTRs in affected areas | √ | PAN: Asymptomatic micro-aneurysms Wegener’s: sinusitis, pulmonary and renal lesions, +/– eosinophilia | PAN: Chronic active hepatitis B Wegener’s: Unknown etiology | ||
| Leprosy | Mycobacterium leprae | Onset: Insidious/acute Clinical patterns: Mononeuritis multiplex Polyneuropathy Common features: Anesthetic lesions, enlarged nerves | √ | Deformity Nerves most commonly affected: Median, ulnar, peroneal | General Genetic susceptibility Prior residence in endemic areas Neuropathy Tuberculoid Reversal reaction |
Abbreviations: AIDP = acute inflammatory demyelinating polyneuropathy; CIDP = chronic inflammatory demyelinating polyneuropathy; CNS = central nervous system; DTRs = deep tendon reflexes; EBV = Epstein–Barr virus; HIV = human immunodeficiency virus; IDUs = injecting drug users; PNS = peripheral nervous system.
Abbreviations: ADEM = acute demyelinating encephalomyelitis; CNS = central nervous system; CSF = cerebrospinal fluid; HSV = herpes simplex virus; HIV = human immunodeficiency virus; PNS = peripheral nervous system; VZV = varicella-zoster virus; IVDU = intravenous drug use; GBS = Guillain–Barré syndrome; CIDP = chronic inflammatory demyelinating polyneuropathy.
| Autoimmune/idiopathic Acute inflammatory demyelinating polyneuropathy (AIDP – Guillain–Barré syndrome) Chronic inflammatory demyelinating polyneuropathy (CIDP) |
| Vasculitis Bell’s palsy Ataxic dorsal radiculopathy Mononeuritis multiplex from hepatitis B virus (HBV)-associated cryoglobulinemia |
| Opportunistic infections Cryptococcal meningitis: bulbar palsies Herpesviruses polyradiculopathy, sacral radiculitis, Bell’s palsy Epstein–Barr virus Cytomegalovirus (CMV) Varicella-zoster virus (VZV) Herpes simplex type 1 (HSV-1) type 2 (HSV-2) Neurosyphilis: polyradiculopathy Tuberculous meningitis: bulbar palsies |
| Drug toxicity or nutritional Antiretroviral nucleoside analogs Dideoxycytosine (ddC) Dideoxyinosine (ddI) Stavudine (d4T) Niacin analog: isoniazid (INH) without B6 Neurotoxic antibiotics: aminoglycosides, chloramphenicol, metronidazole, nitrofurantoin, polymyxins Vitamin deficiencies: folate, pyridoxine, B12 |
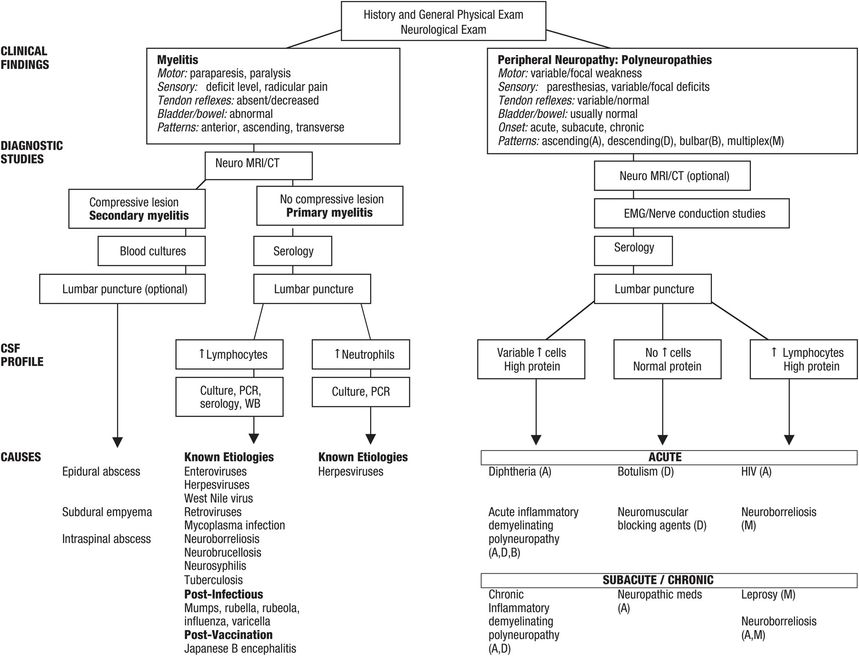
Figure 79.1 Algorithm for clinical and laboratory evaluation of acute myelitis and peripheral neuropathy.
Abbreviations: CSF = cerebrospinal fluid; CT = computed tomography; EMG = electromyogram; MRI = magnetic resonance imaging; PCR = polymerase chain reaction; WB = Western blot.
Myelitis
Myelitis refers to inflammation of the spinal cord. Myelitis may be infectious or noninfectious and primary – directly attacking cord structures – or secondary – adjacent processes altering cord function. Primary myelitis can present as one of three discrete clinical patterns: (1) anterior poliomyelitis, (2) leukomyelitis, or (3) transverse myelitis. Poliomyelitis is inflammation involving gray matter; leukomyelitis is confined to white matter. Transverse myelitis, inflammation of an entire cross section of the spinal cord, can affect more than one spinal segment. A number of infectious agents are known to cause or to be associated with myelitis. Myelitis can also occur after infection or vaccination as in the acute disseminated encephalomyelitis (ADEM) syndrome.
There are five cardinal manifestations of spinal cord disease: pain; motor deficits; sensory deficits; abnormalities of reflexes and muscle tone; and bladder dysfunction. The distribution of neurologic deficits depends on the spinal segment(s) affected. Local pain occurs at the site of the lesion and can assume a radicular quality if the nerve roots are involved. Paresthesias have greater localizing value than radicular pain. Weakness is present in virtually all spinal cord disorders, and in myelitis may progress over hours, days, or weeks. Spinal shock is characterized by absent plantar reflexes, and areflexia and atonia below the level of the lesion. More slowly progressive lesions are associated with hyperreflexia and hypertonia. Bladder dysfunction is usually not an early sign of spinal cord disease, although if spinal shock develops, flaccid bladder paralysis ensues with urinary retention and overflow incontinence. Chronic myelopathies cause a spastic bladder and result in urgency, frequency, and incontinence.
Acute primary infectious transverse myelitis must be distinguished from infectious secondary myelopathies and other noninfectious causes of myelitis such as multiple sclerosis or systemic lupus erythematosus. Magnetic resonance imaging (MRI) of the spinal cord must be performed early to exclude a compressive lesion.
Tropical spastic paraparesis/HTLV-1-associated myelopathy
Human T-cell lymphotropic virus type 1 (HTLV-1) is a retrovirus associated with adult T-cell leukemia/lymphoma and HTLV-1-associated myelopathy/tropical spastic paraparesis (HAM/TSP). Approximately 15 to 20 million people are infected worldwide with endemic areas in the Caribbean, southern Japan, Africa, and Italy. Among first time US blood donors, the prevalence in 2009 was 5 per 10 000,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





