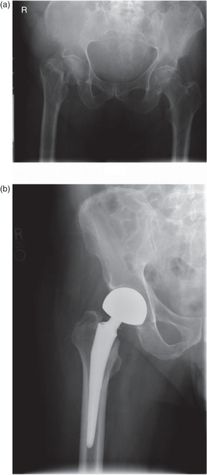
(A) Preoperative and (B) postoperative anteroposterior (AP) radiographs of a displaced periprosthetic fracture of the femur distal to a total hip replacement. The implant was stable in the femur and the decision was made to proceed with open reduction and internal fixation of the fracture while retaining the implant in the stable position.
Pathologic fractures
Metastatic disease
The skeleton is the third most common site of metastatic disease. The incidence of bony involvement in patients with a known malignancy is reported to be between 12% and 70%.[31–33] Common primary malignancies that metastasize to the skeleton are lung, breast, renal, thyroid, and brain. Furthermore, primary malignancies and dyscrasias may involve the skeleton, such as lymphoma, myeloma, and chondrosarcoma. The proximal femur is the most common location of pathologic fracture and is involved in over 50% of cases. This is due to the significant mechanical stresses that occur across the hip joint and proximal femur during ambulation.[34]
Treatments are, again, directed at early patient mobilization. Surgical treatment is the standard of care in treatment of neoplastic fractures, especially those of the femur.[35] The goals are to restore function, alleviate pain, facilitate nursing care, decrease hospital stays, and improve patient quality of life. Surgical contraindications are few but may include obtunded mental status, inability to tolerate the operative procedure, and life expectancy less than one or two months.
Atypical fractures of the femur associated with bisphosphonate use
Bisphosphonate treatment is steadily growing in the elderly population. As osteoporosis screening is promoted widely in the lay media, and patients live longer, bisphosphonate use is increasing. With this increasing prevalence have emerged reports of atypical fractures in the metadiaphysis of the femur that are associated with bisphosphonate use.[36] Many patients report prodromal thigh pain. Occasionally, the thigh pain prompts radiographic evaluation before complete fracture occurs (Figure 34.2A).
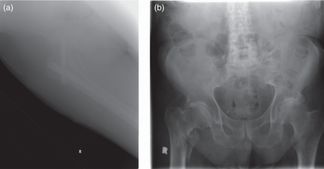
(A) AP radiograph of the right hip of a patient on chronic bisphosphonate therapy with a six-month history of thigh pain. There is an incomplete fracture, transversely oriented, from the thickened lateral cortex that does not extend through medial cortex. This patient was taken to the OR for operative stabilization. (B) AP radiograph of the pelvis of patient on chronic bisphosphonate therapy who sustained a fall. Note the hallmarks of atypical femur fractures: subtrochanteric location, transverse fracture line, lateral cortical thickening, and medial cortical spike.
Investigation of the histology and biomarkers present in the deranged tissue has given rise to the theory that these stem from stress fractures in which bisphosphonate use impairs healing by suppressing bone turnover.[37, 38] In the patient on chronic bisphosphonate treatment, complaints of thigh pain should prompt a radiographic evaluation.
The constellation of cortical thickening, transverse fracture pattern, and a medial spike when the fracture extends through the medial cortex, in the context of a low-energy insult, is the characteristic radiographic presentation (Figure 34.2B).[39] If radiographs are normal but pain persists, a magnetic resonance imaging (MRI) should be performed.[40]
In patients with complete or impending fracture, even those that are nondisplaced, operative treatment is strongly advised to avoid the complications associated with prolonged bed rest.[41, 42] Furthermore, surveillance of the contralateral limb should be performed in these patients with a low threshold for prophylactic treatment, if findings are present,[39] in order to prevent progression and reduce total hospital admission time.[43]
Preoperative considerations
Absolute indications for operative fracture treatment are open fractures, compartment syndrome, and neurovascular compromise. Relative surgical indications include displaced intra-articular fractures in which acceptable reduction and alignment cannot be maintained and fractures that require stabilization in order to mobilize the patient out of bed. Fracture management in the elderly must take into consideration all of the injury factors, patient factors, and special considerations previously described. All aspects must be considered to develop an individualized plan of care.
Timing of surgery in the elderly patient is controversial. Generally, surgery should be performed when comorbid medical conditions have been optimized. Retrospective analayses have offered equivocal assessments on the relationship between timing and morbidity.[44, 45] A prospective study from our institution of 367 hip fracture patients demonstrated that surgical delay of more than two days from hospital admission doubled the risk of patient death at one year when age, sex, and number of comorbidities was controlled.[46]
No significant difference has been demonstrated in survival rates in patients undergoing operative treatment of hip fractures with either regional or general anesthetics.[47, 48] There has been demonstrated a reduced incidence of thromboembolic events (DVT, pulmonary embolus) after use of regional anesthesia.[49] Because pulmonary embolism is a significant cause of morbidity and mortality in the geriatric patient, regional anesthesia is preferable when appropriate.
Implant choice should reflect the surgical goal: to achieve a stable fracture construct with anatomic or near anatomic alignment and/or reduction of articular surfaces to allow early mobilization of the patient and range of motion of the affected joint. Fracture impaction restores structural continuity, allows for force transmission across the fracture segment, and decreases the overall forces on the implant, all of which improve outcome and healing potential.
Intramedullary devices are the implant of choice for fractures in osteopenic bone when the location and fracture pattern are amenable. Placement of intramedullary implants is closer to the mechanical axis of the bone; thus, they act as a load-sharing device. Plates, which are placed directly on the bone, are further from the mechanical axis and act as load-bearing devices.
Hip fractures
Principles
Hip fractures in the elderly can be a life threatening injury because of the impact on medical, functional, and psychological status of the patient. More than 250,000 hip fractures occur annually in the United States, which result in over %9 billion in health-care costs. Current age trends predict a doubling of the yearly incidence of hip fractures by the year 2050.[50–52]
The risk of a hip fracture increases with age, doubling every decade after the age of 50. Hip fractures occur most commonly in Caucasian women, followed by Caucasian men, then African-American women and men. This may be due to differences in bone density between these groups. Institutionalized patients are also at an increased risk for hip fracture, often with greater risk of mortality.[53–58]
Hip fractures in the elderly usually occur from low energy trauma. They are categorized by anatomic location into two classes: intra-capsular (femoral neck fractures) or extra-capsular (intertrochanteric and subtrochanteric fractures). Fractures of the femoral neck are intracapsular, extra-articular fractures that occur in the region between the femoral head and the intertrochanteric line. The location of these fractures can compromise the primary blood supply to the femoral head, especially in displaced fractures.
The intertrochanteric region lies outside the hip capsule, in between the greater and lesser trochanters. This area of metaphyseal bone benefits from a rich blood supply and, as a result, carries a lower risk of the healing complications associated with intracapsular fractures. The greater trochanter is a superolateral structure that serves as the insertion point for the hip abductors and short external rotators. The lesser trochanter is located distally at the posteromedial surface of the proximal femur and serves as the attachment site for the iliopsoas. The calcar femorale is a region of bone located along the posteomedial portion of the proximal femur and acts as a cortical strut to transmit the large forces across the intertrochanteric region.
Presentation and initial management
Patients who have sustained a hip fracture present with complaint of hip and groin pain with the inability to bear weight on the affected extremity after a fall. The affected extremity is usually positioned in external rotation and slight hip flexion. This position provides maximal capsular volume and the most comfort from the hematoma that develops in intracapsular fractures; in displaced extracapsular fractures, the displacement of the fracture results in a shortened and externally rotated position of the lower extremity. There will often be a noticeable leg length discrepancy. Evaluation should include a thorough neurovascular exam of the affected extremity as well as examination of all other extremities to exclude concomitant fracture. Neurologic examination should assess mental status and inquire as to loss of consciousness associated with the fall.
Medical consultation should be obtained at the time of presentation to optimize the patient medically for anticipated surgery. Injury radiographs, initial laboratory investigations, chest radiograph, and electrocardiogram should be performed. A baseline arterial blood gas may be warranted since hip fractures carry a risk for thromboembolic phenomena. A Foley catheter should be placed to eliminate the need for positioning on a bedpan or use of a urinal to minimize patient discomfort. Additionally, the Foley catheter allows accurate measurement of urine production, important for volume status assessment in these patients who may not have had adequate fluid intake after their injury due to access or pain. Orthogonal films should include a true anteroposterior (AP) and cross-table lateral (Figure 34.2) of the hip. A cross-table lateral projection is preferable to a frog-leg lateral, as the latter causes the bone fragments to rotate through the fracture site, further displacing fracture fragments causing increased discomfort to the patient and the potential for further injury.
If the diagnosis of a hip fracture is suspected but not confirmed by routine radiographs, further imaging studies are indicated. An AP view with axial traction and internal rotation of the affected limb can improve the visualization of the entire femoral head and neck. If doubt remains, a technetium bone scan or MRI should be obtained. A technetium bone scan requires two to three days after injury to minimize the risk of false-negative, whereas an MRI can accurately diagnose occult fracture within 24 hours after injury.[59] The preferred treatment of hip fractures is operative because it allows early mobilization of the patient, thereby decreasing the risk of cardiopulmonary events, urinary tract infections, decubitus ulcers, and the rate of mortality in the first year. It also minimizes the period of non–weight bearing, decreases the risk of nonunion/malunion, and increases the ease of transfer. Overall, operative management also decreases the cost of hip fractures, which is becoming increasingly important.[60]
As for any hospitalized patient, the potential for thromboembolic events (DVT or PE) is concerning. In addition to mechanoprophylaxis, chemoprophylaxis should be administered; however, the risk of bleeding in the injured or postoperative patient is an important consideration and must be balanced with the need for prophylaxis. Warfarin, the historic gold standard, requires daily monitoring and carries a significant risk of bleeding. Low molecular weight heparins (LMWH) have been the contemporary choice, effective without the need for laboratory monitoring, although their subcutaneous administration raises compliance concerns post-hospitalization.[61–63] A promising alternative has emerged: rivaroxaban is a direct factor Xa inhibitor, orally administered, with predictable pharmacokinetics and the same efficacy as LWMH.[64] Discussion between the medical and surgical teams should pinpoint the precise starting time postoperatively, but generally chemoprophylaxis should begin 12 hours postoperatively. An inferior vena cava filter may be used when anticoagulation is contraindicated or in patients at a high risk for recurrent thromboembolism.
Outcomes
The goal of surgical treatment of hip fractures is to restore the patient’s functional status to the pre-injury level. At one-year follow-up, 41% of patients will regain their pre-injury ambulatory status, 40% will require increased assistance, and 8% will become nonambulatory.[65]
Mortality rates of hip fracture patients are twice that of age- and sex-matched controls.[44, 66, 67] The highest increase is seen in the first 6 months after injury, and progressively decreases to that of age- and sex-matched controls at one year. However, one-year mortality can be as high as 30%.[67–69]
While the amount of time from injury to surgical treatment has been debated as a predictive factor, a prospective study from our institution in which age, sex, and other comorbidities were controlled, demonstrated that a delay of surgical treatment for more than two days in patients who did not suffer from dementia and were ambulatory prior to injury doubled one-year mortality.[46]
Postoperative rehabilitation should employ a weight bearing as tolerated program. Although some have recommended restricted weight bearing (or even non–weight bearing), in situations when fracture fixation is felt to be suboptimal, we feel that this has a very negative impact on the overall recovery and does not accomplish the intended goal of limiting forces across the hip (and therefore on the fracture fixation). Joint reaction forces across the hip are actually higher with non-weight bearing as opposed to toe-touch weight bearing. When elderly patients are allowed immediate postoperative weight bearing as tolerated, they tend to self-regulate the amount of weight on the injured extremity and will gradually increase the amount of weight bearing as their comfort allows.[70, 71] The approach encourages, rather than limits, their recovery of mobility and ambulation.
Femoral neck fractures
Femoral neck fractures, as previously discussed, are intracapsular fractures. They are generally classified as nondisplaced or displaced. Nondisplaced fractures may be treated nonoperatively, for the sick or nonambulatory patient; however, there are reports of increased rates of nonunion. For this reason as well as for earlier mobilization, internal fixation, with cannulated screws or a head screw with side plate (sliding hip screw), is preferable. Displaced fractures are similarly treated for patients under 60 years old. Displaced fractures in patients over 80 years old are treated with arthroplasty, a total hip replacement for healthy, active patients, and hemiarthroplasty for lower-demand patients. For patients between 60 and 80 years old, the decision to fix the fracture versus replacing the joint has to be individualized, taking into account the patient’s lifestyle, independence, physiologic age, bone quality, and comorbidities.[72] See Figures 34.3 and 34.4.

A sketch depicting the proper method of evaluating suspected hip fractures, demonstrating (A) AP and (B) cross-table lateral radiographs of a displaced fracture of the subcapital femoral neck in a patient with limited ambulatory capability.
(A), Preoperative and (B) postoperative AP radiographs of a displaced fracture of the subcapital femoral neck in a patient with limited ambulatory capability. This injury is associated with a high incidence of avascular necrosis, compromising healing when the femoral head is retained. Therefore, this fracture was treated with hip hemiarthroplasty.
Osteonecrosis of the femoral head and nonunion following femoral neck fractures increase in frequency as the degree of fracture displacement increases. Therefore, nondisplaced fractures have rates of these complications between 5%–10% while these rates are 20%–35% for displaced fractures.[73–79] The presence of these complications is a common indication for revision surgery. See Figure 34.5.
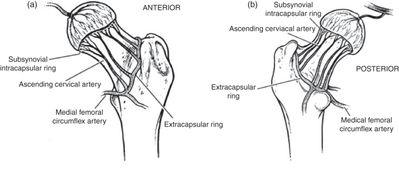
Vascular anatomy of the femoral neck.
Intertrochanteric hip fractures
Intertrochanteric hip fractures are classified as stable or unstable, based on whether or not the posteriomedial buttress (calcar femorale) is intact or comminuted. This is determined on injury radiographs based upon the position of the lesser trochanter. Stable fractures are characterized by an intact lesser trochanter on the distal fracture fragment, whereas unstable fractures demonstrate a large, displaced lesser trochanteric fragment. A large, displaced lesser trochanteric fragment is an indication of calcar comminution and an unstable fracture pattern.
Surgery is the treatment of choice for all intertrochanteric hip fractures. Although they have been most commonly treated with extramedullary devices (those that reside outside of the central canal of the femur, such as a sliding hip screw), recently, an increasing number are being treated with cephalomedullary (intramedullary) devices (Figure 34.6). Both methods are accepted forms of operative treatment and have demonstrated similar results and complications in recent prospective, randomized studies.[80–82] The indications and goals for nonoperative treatment are similar to those for femoral neck fractures.
(A) Preoperative and (B) postoperative AP radiographs of an unstable intertrochanteric hip fracture. This fracture was fixed with a cephalomedullary device.
Ankle fractures
The ankle joint is a modified hinge joint consisting of the lateral malleolus (tuberosity on the distal fibula), the medial malleolus (tuberosity on the distal tibia), the plafond (central articular surface of the distal tibia), and the talus. Binding these osseous structures are the lateral collateral ligament, the deltoid ligament, and the tibiofibular syndesmosis. The lateral collateral ligament is composed of three structures: the anterior talofibular ligment, the calcaneofibular ligmament, and the posterior tibiofibular ligament. The deltoid ligament consists of an anterior, superficial portion that attaches to the navicular, sustentaculum tali, and the talus, while the stronger, deeper, posterior portion originates on the posterior colliculus of the medial malleolus and inserts on the medial surface of the talus.
The clinical examination of a patient with a suspected ankle injury should include palpation of the abovementioned osseous and ligamentous structures. Swelling and ecchymoses should be noted. Weight-bearing ability must be determined (patients are rarely able to bear weight on an unstable fracture). A neurovascular exam should be performed, ensuring that ankle dorsi- and plantarflexion are intact, as is great toe flexion and extension. Sensation should be tested over the dorsum of the foot, first web space, medial and lateral edges of the foot, and the plantar surface.
The decision to evaluate an ankle radiographically after injury should be made using the Ottawa Ankle Rules. Only patients with tenderness over the inferior or posterior pole of either malleolus (defined as the distal 6 cm for these guidelines) and the inability to take four steps independently (even if limping) should have x-rays.[83] Radiographic examination should include three views of the ankle: an antero-posterior view, a mortise view (20 degree internal rotation oblique), and a lateral view. Ankle fractures can include isolated lateral malleolus/distal fibula fractures, isolated medial malleolus fractures, fractures of both malleoli (bimalleoloar), or both malleoli and the posterior portion of the tibial plafond (trimalleolar). Isolated fractures of the lateral malleolus should be evaluated with stress views to exclude the presence of a medial soft tissue injury that will lead to ankle instability.[84]
The goal of treatment of ankle fractures in elderly patients is to restore the normal tibiotalar relationship while maintaining a congruous joint surface. Stable injuries, such as isolated lateral malleolus fractures without medial disruption, should be rested in the acute post-injury period with gradual return to weight-bearing as tolerated with the use of a brace or fracture boot.
Bi-malleolar injuries (including their equivalent lateral malleolus fractures combined with medial soft tissue disruption) and fractures associated with talar displacement and joint incongruity are unstable and require operative fixation. Even slight talar incongruity can lead to early post-traumatic arthritis.[85] The primary goal of operative treatment of an elderly patient with an ankle fracture is to obtain or maintain an anatomic relationship of the tibia, fibula, and talus, and thereby joint congruity.
The timing of surgery depends largely on the condition of the soft tissue envelope. Ankle fractures and fracture-dislocations can be associated with significant swelling and the development of fracture blisters. When present, operative treatment should be avoided because of the risk of soft tissue sloughing following the surgical procedure. The return of skin wrinkles about the ankle herald adequate subsidence of swelling. Studies have shown that operative treatment restores anatomic relationships and stability, as well as improving function and pain scores over time.[86, 87] Patients with unstable injuries should remain non–weight bearing until bony union is achieved and soft tissue supporting structures have had the chance to heal.
Proximal humerus fractures
Proximal humerus fractures are common in the elderly population. The proximal humerus is the third most common site of fracture and often occurs as a result of a low energy mechanism, such as a fall from standing position.
The current system used to classify fractures of the proximal humerus fractures was first described by Neer.[88, 89] This classification divides the proximal humerus into four anatomic segments: the head, the shaft, the lesser tuberosity, and the greater tuberosity. A segment is considered independent if it is displaced 1 cm or more, or angulated 45 degrees or more from its anatomic position. Thus, proximal humerus fractures can be defined as one part (minimally displaced), or as two-, three-, or four-part fractures. This system provides treatment guidelines and predicts outcome based upon fracture type.
Minimally displaced fractures account for approximately 85% of all proximal humerus fractures. These fractures have an intact surrounding soft-tissue envelope, and all parts can be expected to move as a single unit. These injuries are treated with an initial period of immobilization in a sling, followed by range of motion exercises beginning about one week post-injury.
Two-part fractures through the surgical neck of the humerus are treated operatively with reduction and internal fixation. Fractures through the anatomic neck are rare and treated with reduction and internal fixation in younger patients and with arthroplasty in older patients. Greater tuberosity fractures are treated operatively if there is greater than 5 mm superior translation, to preserve rotator cuff function. Lesser tuberosity fractures may be treated closed unless there is a block to internal rotation.
Three- and four-part fractures are at increased risk for osteonecrosis of the humeral head and require operative management. Treatment preference – internal fixation versus prosthetic replacement – is determined by patient factors (age, activity level) and fracture factors (bone quality, comminution, and presence of dislocation). Currently, options for prosthetic replacement include hemiarthroplasty or reverse total shoulder arthroplasty (Figure 34.7).
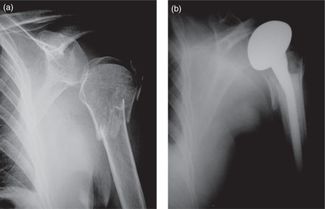
(A) Preoperative and (B) postoperative AP radiographs of a displaced three-part fracture of the proximal humerus treated with prosthetic replacement.
Regardless of treatment approach, elderly patients with displaced proximal humerus fractures require a prolonged, supervised physiotherapy program to optimize functional outcomes. Minimally displaced one-part and adequately reduced two-part fractures can be expected to have good functional outcomes. Poor results may be related to compromise of the rotator cuff, malunion, nonunion, or osteonecrosis. Results of prosthetic replacement are predictable for pain relief, but less consistent for functional recovery.
Distal radius fractures
Distal radius fractures occur more commonly in geriatric patients than any other. The incidence increases dramatically with age, particularly for women, and parallels that seen for fractures of the proximal humerus and proximal femur.[90] Distal radius fractures have been attributed to the presence of osteoporosis, as well as poor eyesight, impaired coordination, and decreased muscular strength.
Unstable fractures are identified by marked comminution, greater than 1 cm of shortening, loss of palmar tilt, greater than 10 degrees of dorsal tilt, and intraarticular displacment (Figure 34.8A, B). Unstable fractures account for 15%–25% of distal radius injuries in the geriatric population and are generally associated with poorer outcome.

(A) AP and (B) lateral radiographs of an unstable distal radius fracture demonstrating significant shortening and comminution as well as loss of radial inclination and palmar tilt. (C) This fracture was indicated for operative fixation, and was repaired using open reduction and internal fixation with a volar plate.
Closed reduction and splint/cast application is the treatment of choice for most distal radius fractures in elderly patients and should be attempted initially, even for unstable fractures. If closed reduction is successful, immobilization should continue for six weeks and radiographs should be performed weekly for three to four weeks to ensure that the reduction is maintained.
If closed reduction is not successful or not able to be maintained, operative intervention may be necessary, particularly when treating an active-elderly patient with involvement of the dominant extremity. A variety of operative techniques have been described, such as external fixation, percutaneous pin fixation, and internal plate fixation. The choice is often surgeon-dependent, and each option has its own, risk–benefit profile.
Functional outcome after distal radius fracture is often favorable, though dependent on patient factors, treatment method, and quality of reduction. Minimally displaced fractures treated in cast immobilization generally do well with minimal loss of pre-injury function. Surgical fixation of displaced fractures demonstrates good to excellent results in 70%–90% of patients with comminuted, unstable fractures.[91].] However, in low-demand elderly patients, even closed treatment of displaced fractures may yield acceptable functional results despite a cosmetic deformity.[92] Ultimately, the treatment of each patient should be individualized and should be based on fracture type, as well as presence of comorbidities, pre-injury functional status, and hand dominance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




