Implementation of a Multidisciplinary Care Program
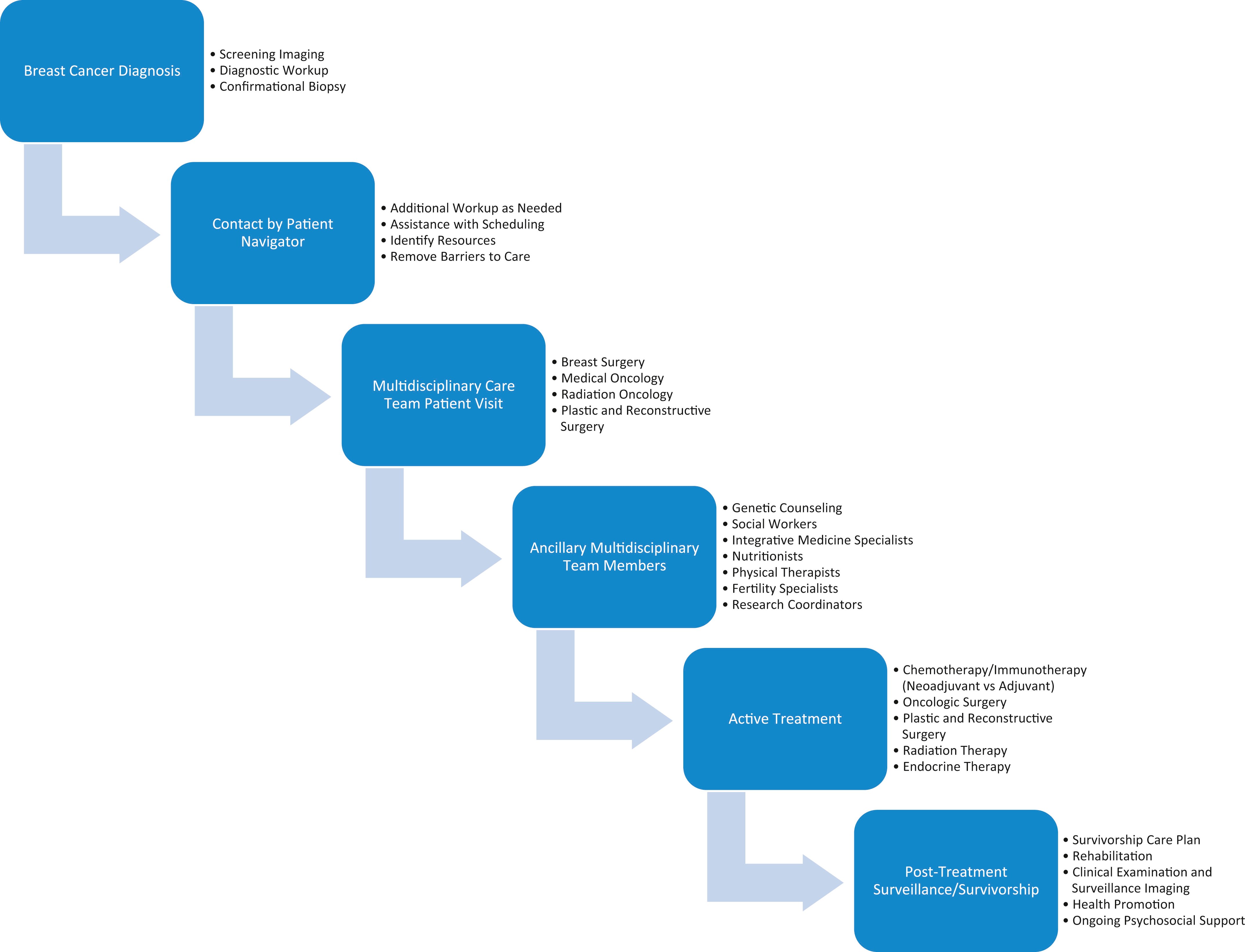
When setting up a multidisciplinary treatment program ( Fig. 2.1 ), several areas must be evaluated, which include selecting the needed personnel, their proximity to the primary treatment site(s), and their ability to attend meetings in-person or virtually. The types of meetings that can be arranged include multidisciplinary tumor boards (case presentations) and multidisciplinary clinic conferences (patient seen and examined by the team) also known as multidisciplinary care centers (MDCC). The difference includes whether there is only a discussion of the patient’s relevant history, physical examination, radiologic studies, and pathology versus the direct patient evaluation with the patient physically present to be examined by the team and participating in the treatment discussion. There are benefits and drawbacks of each approach. For tumor board presentations, clinicians may be present in one location, or may join remotely. The relevant history and findings can be shown to the group by radiology and pathology, and an agreement of the proper treatment pathway can be reached with one member of the team designated to convey the information to the patient and implement the treatment plan. The drawback is that the patient may need to make several visits to the clinicians, and therefore it may not be the most time-effective approach. Some recent studies have recommended patients receive their first course of therapy within 30 days of diagnosis. Delays in treatment implementation may lead to earlier recurrence or reduction in cure rate. In the MDCC model, the patient is seen and examined by the relevant members of the team (typically surgery, medical, radiation oncology, and plastic surgery (when needed), and a decision about treatment is reached and implemented by the chosen team member. Radiologists and pathologists with an interest in breast cancer may also be present or available upon request to review imaging and pathology and/or for surgical planning. Patients are also seen by a nurse navigator to assist in logistics of the treatment implementation, as well as referral to plastic and reconstructive surgeons, social workers, integrative and complementary medicine specialists, nutritionists, physical therapists, and genetic counseling as needed. Drawbacks of this approach include the potential for time inefficiency for the clinician who may need to wait for other members of the multidisciplinary team to complete their evaluations. Often a hybrid model can be effective where the patient’s case is presented to the larger group of clinicians, and a smaller, select group then gathers to meet and examine the patient and have a discussion with the patient regarding the proposed treatment pathway.
Program Components
Multidisciplinary breast cancer treatment teams include the following physician specialties: surgery (breast surgery, surgical oncology, and/or general surgery), plastic and reconstructive surgery, medical oncology, radiation oncology, breast radiology, and pathology. The following ancillary service representatives are recommended to assist the core multidisciplinary team: tumor registry, nurse navigation, research, and genetics. Other areas may be added at the discretion of the site, including complementary and integrative health, fertility specialists, physical and occupational therapy, nutrition, pastoral care, as well as trainees in medicine, nursing, and other allied health fields. For the initial evaluation of the patient, the three major disciplines—surgery, medical oncology, and radiation oncology—should be available to assess and examine the patient. Residents and fellows of the appropriate disciplines are encouraged to attend as well.
Value of Multidisciplinary Care
In a system with a well-defined treatment paradigm and well-defined pathways for care, the implementation of multidisciplinary care teams and pathways allows for the most accurate, up-to-date evidence-based and cost-effective care ( Fig. 2.1 ). Patients are seen by the key members of the treatment team, and treatment decisions are made in a collaborative format using the best evidence. Patients and their families can be part of the decision-making process and feel empowered by their inclusion. Multidisciplinary treatment teams provide a high level of patient and family satisfaction and allow patients to both participate and understand the scientific/medical basis for the treatment decisions. In this setting, patients are encouraged to participate in the shared decision-making process when options are presented. Patients can then be presented and evaluated again during times of treatment change, further allowing refinement and clarification of the individualized care plan.
Which Patients Should Participate?
In an optimal situation, all breast cancer patients would be treated in a multidisciplinary treatment environment. Certain patients should preferentially be seen in a multidisciplinary format (personnel and space permitting). All patients with newly diagnosed invasive or in situ cancer should be seen by a multidisciplinary team to assess the tumor extent and decide about the treatment pathway. Prior to the meeting, it is best that the following information be gathered and available for review: patient’s history including prior breast biopsies and pathology (reviewed by in-house pathologists and radiologists), menstrual and pregnancy history, family history of breast and other cancers, any prior genetic testing, and what, if any, symptoms led to evaluation. In addition, all imaging of the breast should be available for review, including any prior films for comparison. The pathology should be available for in-house review, including all prognostic biomarker studies that have been performed (estrogen and progesterone receptor status, Her-2-neu status, and KI-67 if ordered). The nurse navigator plays a key role in reaching out to the patient/family and gathering this information to be available for the team’s review. Other patients who are optimal for multidisciplinary format review and evaluation include patients who are being considered for neoadjuvant therapy, those completing neoadjuvant therapy, patients with suspected or documented recurrence, and any patient for which multidisciplinary evaluation may help in complex decision making. Some of these include patients with genetic mutations that increase the risk of breast cancer, patients with pre-malignant lesions, and patients in whom therapy is not taking the expected course. The goal is to be inclusive rather than exclusive.
Decisions on Testing Prior to and After Multidisciplinary Evaluation
When a patient presents for their multidisciplinary appointment, each member of the team should independently and then jointly review all the available data including available history and physical examination data, radiologic studies, and pathology including prognostic biomarkers. The team should then decide if any additional testing is required to recommend a treatment plan. These decisions may involve the request for additional biopsies of areas not originally sampled, the repeating of marker studies, and additional radiologic studies such as breast magnetic resonance imaging (MRI) to determine the extent of tumor within the breast or axilla, and staging studies such as computed tomography (CT), bone scintigraphy, and positron emission tomography (PET) scanning to determine if local or distant metastatic disease may be present. This may lead to additional studies being requested, such as second-look ultrasound and additional biopsies under MRI or ultrasound guidance. Referral for genetic evaluation and research study participation should also be an integral part of the multidisciplinary evaluation.
High-Risk Patient Evaluation and Management
The appropriate management of patients at elevated risk for developing breast cancer is a complex topic. These patients are appropriate for a multidisciplinary management panel when they have developed cancerous or precancerous findings. The management of these patients at elevated risk and discussion of risk reduction strategies will be covered more fully in Chapter 15 of this book.
Women born and residing in the United States have a breast cancer risk of approximately 12.5% (1:8). This risk increases with age and varies in different ethnic groups. Women considered at high risk are generally assumed to have a breast cancer lifetime risk of 20% on any of the commonly used calculation models (Tyrer-Cuzick, or Gail, or other models). These models utilize patient age; menstrual and pregnancy history; family history of breast, ovarian, and other cancers (and the age at which they were diagnosed); biopsy history (particularly with atypia seen); breast density; and prior exposure to radiation, among others, to calculate a risk score. Genetic evaluation and referral to our family cancer genetics program is offered for those patients whose personal or family history would make them appropriate for genetic testing.
Women who are found to be at high risk are referred to our high-risk breast program and are seen by the physicians and advanced practice clinicians and undergo a more in-depth risk assessment. If they are truly at high risk, then they are counseled about risk-reduction strategies as well as enhanced screening. Those at highest risk begin screening at age 35, or 10 years earlier than their earliest family member developed breast cancer. This enhanced screening includes biannual in-person evaluation and alternating mammogram/ultrasound and MRI at 6-month intervals. Patients are counseled regarding risk-reducing strategies including exercise; diet; healthy living and avoiding obesity, smoking, and excess alcohol; and other behaviors that will further increase their risk. They are also offered risk-reducing anti-estrogen therapies when appropriate. Those at the highest level of risk are offered risk-reducing surgeries (mastectomy and oophorectomy) as appropriate.
When a patient at high risk does develop invasive or in situ breast cancer, they are evaluated in a multidisciplinary setting to discuss appropriate treatment options. The patients are included in this joint decision-making process to allow their input into the treatment options. This complex decision making often needs to take into consideration genetic syndromes that increase the risk of subsequent cancers, patient’s reproductive desires, and their concerns regarding the ability of screening tests to discover other cancers if they should develop. The team assesses the patient’s risks of recurrence, and of developing a subsequent cancer, and makes recommendations based on the best available information. Based on the extent of the cancer, breast-conserving surgery may or may not be recommended or given as an option. Overall, the patient partners with the team to develop the best individual treatment strategy within the parameters of our treatment protocols.
Ancillary Services to Assist the Breast Cancer Patient
Although the implementation and management of care for the patient with breast cancer may largely be driven by the surgical, medical, and radiation oncology specialists, there are several other ancillary services functioning in the multidisciplinary team to improve patient care. Support groups, both in-person and virtual, have been cited as being particularly helpful for navigating the long- and short-term impact of breast cancer. Emotional support benefits of support groups included a feeling of connectedness as well as understanding, which provided hope and healing to participants. Social workers may also help connect patients to support groups and aid with additional resources, including psychosocial support. Furthermore, breast cancer patient navigators are an essential part of the multidisciplinary team to help provide timely access to services and ensure completion of diagnosis and follow-up of care.
Physical medicine and rehabilitation specialists are also important assets to the multidisciplinary team for the patient with breast cancer. Rehabilitation, which may be facilitated by physical and occupational therapists, includes improving strength and cardiovascular conditioning, alleviating pain, and reducing fatigue. Given the increased risk of lymphedema following axillary surgery and radiation therapy for breast cancer, rehabilitation may also help with both its prevention and management. Furthermore, exercise provides an important role to help women physically recover from treatment and potentially prevent cancer recurrence.
Complementary and integrative medicine therapies may be used for supportive care during breast cancer treatment and to manage treatment-related side effects. Specialists who can facilitate such modalities as music therapy, meditation, yoga, and massage may help with depression as well as improve quality of life. Treatment-related nausea and vomiting may be improved by acupuncture and acupressure, and dietitians help with adequate nutrition and weight management during breast cancer treatment and survivorship. Integrative practices may help as effective supportive care strategies for the care of patients with breast cancer.
Shared Decision Making
Once all the information has been reviewed, the multidisciplinary team reconvenes to discuss the treatment recommendations, which usually will involve a recommendation for surgery or neoadjuvant therapy as the initial modality ( Fig. 2.1 ). As you will see in the subsequent chapters, decision making regarding upfront surgery versus neoadjuvant therapy (chemotherapy, immunotherapy, and/or anti-estrogen therapy) is complex and nuanced. Patients with more advanced disease generally will be selected for neoadjuvant therapy along with patients with more worrisome histologic findings including triple-negative and HER-2-neu positive breast cancers.
Summary and Conclusion
Multidisciplinary input in the care of the patient with breast cancer is essential to provide coordinated, evidence-based, and continuous cost-effective care. Using a team-based approach and shared decision making allows the patients and their families a feeling of participation in the process and will allow for greater compliance in the treatment plan. All members of the team contribute to the patient’s treatment and recovery and should be valued for the important contributions they make to the overall treatment process.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree