Molecular Prognostic Markers of Lung Cancer
Sanja Dacic
Many studies have examined potentially prognostic genetic changes in lung carcinoma using different methodologies from immunohistochemistry to gene expression profiling. However, no clinically useful prognostic gene markers were found. This chapter will review some of the most commonly investigated prognostic markers.
CELL CYCLE REGULATORS
p53
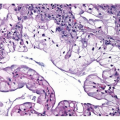
A tumor suppressor gene, p53, is the most studied gene in all types of cancer, including lung cancer. A prognostic significance of this gene in lung cancer is contradictory. This is probably caused by different detection methods used to identify p53 alterations. Immunohistochemistry can detect missense mutant p53 proteins but may not detect the protein products of nonsense, deletion, or truncation mutants.1,2,3 and 4 The frequency of p53 mutations or positive IHC staining is higher in squamous cell carcinoma (60%-70%) than in adenocarcinoma (50%-70%).5 p53 mutations are unique in NSCLC of smokers with an excess of G:C to T:A transversions. Lack of prognostic significance of altered immunoexpression of p53 in NSCLC was more frequently reported. Several studies using p53 mutation analysis found a poorer prognosis for NSCLC with p53 mutations. Studies using both approaches, IHC and mutational analysis, failed to demonstrate a prognostic significance. Overall, conflicting results preclude the use of p53 gene alterations as prognostic markers for NSCLC in clinical practice.
Ras-Raf-Mek
The Ras proteins are members of a large superfamily of GTP-binding proteins involved in signal transduction regulating cell growth. The Ras-Raf-Mek pathway is involved in signaling downstream from EGFR. Activating KRAS mutations are present in up to 30% of lung adenocarcinomas.5 Most KRAS mutations in lung adenocarcinomas are smoking-related G:T transversions and affect exon 12 (in 90% of patients) or exon 13.5 KRAS point mutations may occur in never smokers (about 15%) and they are unrelated to tobacco carcinogens, typically G12D.6 A recent metaanalysis demonstrated that NSCLC patients with KRAS mutations have a worse overall survival.7 KRAS has the potential to be used as a predictive marker for the efficacy of EGFR-TKI therapies and as a prognostic marker in NSCLC.
ERCC1
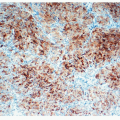
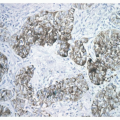
ERCC1 is 1 of 16 genes that encode the proteins of the nucleotide excision repair complex. The nucleotide excision repair pathway recognizes and repairs cisplatin-induced DNA adducts. Small, retrospective clinical studies have repeatedly reported an association between low levels of ERCC1 mRNA in several cancers and improved clinical outcome among patients treated with platinum-containing regimens, particularly in advanced NSCLC.8,9 Recently, the International
Adjuvant Lung Trial (IALT) demonstrated that patients who had NSCLC with no detectable ERCC1 by immunohistochemistry had longer disease-free survival after cisplatinum-based chemotherapy than patients with ERCC1-positive tumors.10 Median overall survival was 14 months longer in ERCC1-negative tumors treated with chemotherapy than in those not receiving chemotherapy. There were no differences in survival between ERCC1-positive tumors in respect to chemotherapy treatment. Another recent study also showed that ERCC1 expression as measured by automated quantitative analysis of immunofluorescence is a determinant of survival in stage I NSCLC. These findings suggest that ERCC1 expression could be potentially used as a prognostic marker.
Adjuvant Lung Trial (IALT) demonstrated that patients who had NSCLC with no detectable ERCC1 by immunohistochemistry had longer disease-free survival after cisplatinum-based chemotherapy than patients with ERCC1-positive tumors.10 Median overall survival was 14 months longer in ERCC1-negative tumors treated with chemotherapy than in those not receiving chemotherapy. There were no differences in survival between ERCC1-positive tumors in respect to chemotherapy treatment. Another recent study also showed that ERCC1 expression as measured by automated quantitative analysis of immunofluorescence is a determinant of survival in stage I NSCLC. These findings suggest that ERCC1 expression could be potentially used as a prognostic marker.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree