Absolute contraindications
Relative contraindications
Previous neck surgerys
Previous neck irradiation
Large goiter
Large adenoma (<3.5 cm)
Parathyroid carcinoma
Lack of preoperative localization
MEN and familial pHPT
12.3 Preoperative Evaluation
An exhaustive preoperative biological evaluation is necessary to confirm the diagnosis of pHPT, as well as in open surgery.
Once the diagnosis is established, a correct preoperative localization of the lesion is generally considered mandatory before performing a MIVAP, as well as any other minimally invasive approach to pHPT. The localization can be based either on an ultrasound examination or on a double phase 99mTc-labeled sestamibi scan. In many cases both imaging studies have already been performed before being referred to the surgeon. Personally we prefer an ultrasound examination using a linear transducer (8–13 mHz) with color-Doppler capability. Indeed, in our experience ultrasound has two important advantages with respect to scintigraphy. It is much more accurate in giving anatomical details, in defining the position of the adenoma and its relationships with vascular structures. It also allows an exact evaluation of its size. It is important to underline that lesions exceeding 30 mm must be very carefully evaluated. Large adenomas are sometimes difficult to remove endoscopically, even in the most experienced hands.
12.4 Patient Preparation
In the case of acute severe hypercalcemia (calcemia >3.5 mEq/L) preoperative saline infusion and diuretic administration may be useful. If the operation is delayed, diphosphonate should be used to treat patients before surgery.
General endotracheal anesthesia is usually performed but also a less invasive anesthetic technique can be successfully used in order to perform MIVAP: a bilateral superficial cervical block in association with a laryngeal mask and sevoflurane. Ropivicaine (Naropine) (7.5 mg/mL) is injected along the medial border of the sternocleidomastoid muscle: 20 mL are generally sufficient to obtain the analgesic block. Inhalatory induction is achieved with O2-sevofluorane and then it is maintained with a gas mixture of O2/N2O (50:50) and sevoflurane (end-tidal: 1–1.3%) with spontaneous breathing through a laryngeal mask. This kind of anesthesia, in our experience, proved to not adversely affect operative time and was very well tolerated by patients who can be discharged earlier than after a general endotracheal anesthesia.
12.5 Operative Technique
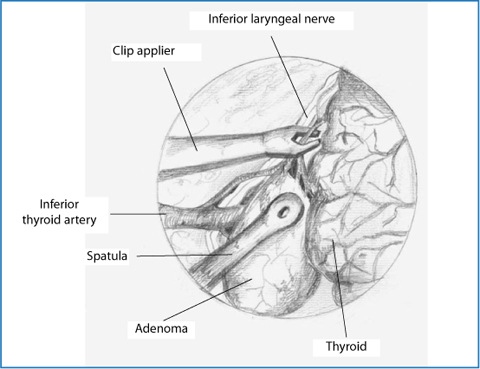
The patient is placed in the supine position; the neck is not hyperextended so as to avoid the reduction of the working space under the strap muscles. The surgical field, covered by a transparent dressing, is prepared to allow conversion to the traditional cervicotomy. A 15-mm horizontal skin incision is performed 2 cm above the sternal notch, then the linea alba is vertically incised so as to prepare the operative space between the strap muscles and the thyroid gland. A 30° 5-mm endoscope is now inserted through the incision and two conventional retractors are applied, one retracting the thyroid lobe medially, the other one pulling the muscles and the carotid artery laterally (Fig. 12.1); the thyrotracheal groove is now well exposed. Needlescopic surgical instruments (spatula for dissection, suction spatula and 2-mm forceps) are inserted through the main access. Videoscope magnification (30×) allows very easy identification of the adenoma and the other relevant neck structures (Fig. 12.2). Once the tumor is visualized, gentle and precise manipulation is mandatory. The gland has to be excised without disrupting its capsule so to avoid the spillage of parathyroid cells with the subsequent risk of parathyromatosis. The use of monopolar cautery is postponed at least until the inferior laryngeal nerve that generally lies right under or above the parathyroid gland, is visualized. Usually there is no need for hemostasis while freeing the adenoma from the fascia. Later on, when the hylus of the gland is reached, vessels ligation can be easily obtained by means of two conventional 3 mm vascular clips (Fig. 12.3). Finally the adenoma is removed and retrieved through the incision, which is then closed while the surgeon is waiting for the results of the intraoperative quick parathyroid hormone assay (qPTHa).
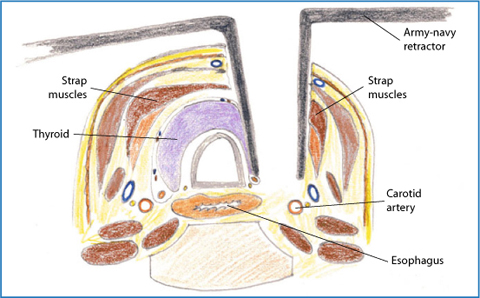
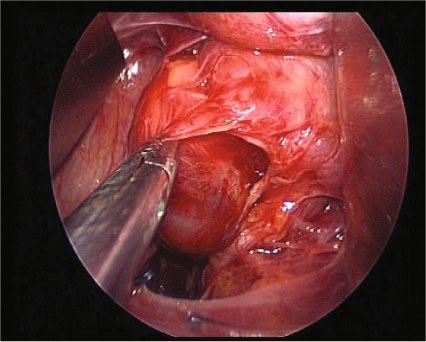
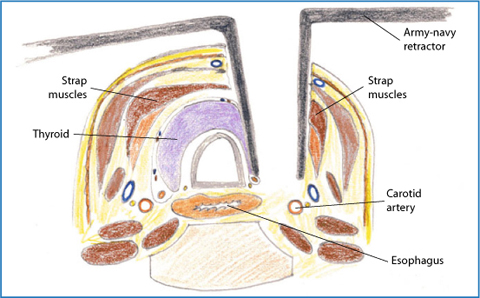
Fig. 12.1
Operative field is maintained by means of conventional “army-navy’ retractors: one retracting the thyroid lobe medially, the other one pulling the muscles and the carotid artery laterally
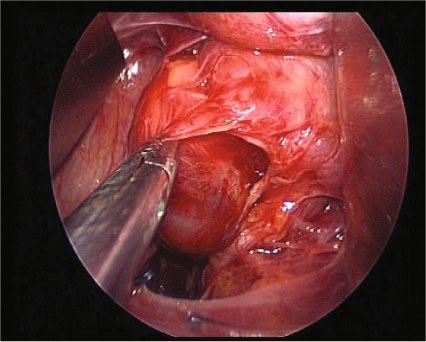
Fig. 12.2
Intraoperative view. The magnification of the endoscope allows a very easy identification of the parathyroid adenoma, as well as of the recurrent nerve