Introduction
Clinics specifically for the diagnosis and management of early dementia were first developed in the USA in the late 1970s. These were primarily research based, linked to developing Alzheimer’s disease (AD) and ageing research centres and acted as a focus for expert assessment, investigation, treatment and advice.1 Initially described as ‘dementia clinics’, the terminology soon changed to the more acceptable name of ‘memory clinics’ or ‘memory assessment clinics’. Although the new titles are less stigmatizing, they run the risk of serving as a euphemism, avoiding an open and honest approach to the reality of dementia.
Predominantly service-oriented memory clinics were set up in the UK in the early 1980s,2, 3 offering multidisciplinary, outpatient-based assessment and diagnosis for mainly older people with memory and other cognitive problems, in an acceptable and accessible environment. At first, many of these clinics were funded from outside the National Health Service and were based mainly in university departments of geriatric medicine or old age psychiatry. Existing services tended to consider memory clinics to be a luxury, allowing academics to indulge their narrow clinical interests away from the reality of budgetary considerations and the priorities of practical dementia care. However, this reflected the concentration of service provision on dealing with the behavioural and psychological symptoms of advanced dementia and on crisis intervention and institutional-based management. The first memory clinics played an important role in raising awareness of the value of elective intervention and interdisciplinary care for people with early dementia and acted as a focus for the development of specialist knowledge and expertise in early diagnosis and management of people presenting with cognitive impairment.
Most of the early UK clinics were also very actively involved in research, especially recruitment into clinical trials of the emerging anti-dementia drugs. Largely thanks to the work of these centres, specific drug treatment for AD became available in the late 1990s and the focus of activity shifted towards the provision of an effective clinical service for patients presenting with memory disturbances and best use of medication, together with psychosocial interventions and patient and carer support and education.4 The evolution of hospital-based memory clinics into more community-based memory teams was the natural consequence, working alongside or as an independent part of traditional mental health teams for older people.
Initially criticized for being too academic and isolated from mainstream practice, and ill-equipped to provide care after diagnosis, memory clinics have now become an integral part of quality dementia assessment and care services. The clinical guideline on the management of dementia published by the UK National Institute for Health and Clinical Excellence (NICE) and the Social Care Institute for Excellence (SCIE) in 2006 recommended the development of memory assessment services as the single point of referral for all people with a possible diagnosis of dementia.5 They were seen as providing a responsive service to aid early identification, including a full range of assessment, diagnostic, therapeutic and rehabilitation services and an integrated approach to the care of people with dementia and the support of their carers, in partnership with local health, social care and voluntary organizations. The National Dementia Strategy in England, published in 2009,6 suggested that memory clinics might form the core of new services for early diagnosis and identification of dementia in ‘every town and city’ in the country.
Although most memory clinics focus on the diagnosis of early dementia and mild cognitive impairment (MCI), some have a broader remit, whereas others target people with purely subjective memory loss or younger people with early-onset dementia or people with learning disabilities. Many concentrate on diagnosis and assessment with a view to best use of available medication and those in academic centres continue to conduct a lot of research, including clinical trials of newer drug treatments. The emphasis on assessment for drug treatment should not detract from the importance of providing the holistic, multiprofessional and multiagency approach to dementia care that should be central to the activity of all clinics.
Referral may be open access (those willing to see all-comers) or restricted to secondary or tertiary referrals or to selected individuals who meet predetermined criteria. In general, patients referred by their general practitioners (GPs) seem more likely to have dementia than self-referrals, although the reassurance given to those without organic disease (the ‘worried well’) should not be underestimated.7 Memory clinics should never be merely rebranded old age psychiatry outpatient clinics or community-based services solely monitoring anti-dementia drugs.
Developments Around The World
Memory clinics are now a feature of health services for older people in centres around the world, but they vary in terms of case mix, types of activity undertaken, whether they are primarily based in neurology, psychiatry or geriatric settings and their interface with other relevant agencies. Nearly all involve multiprofessional assessment, often with everyone coming together to share results in a diagnostic consensus meeting. The subsequent input into long-term support and follow-up can be very different, with some clinics seeing diagnosis and immediate care as the limit of their responsibility and others taking on the role of planning optimal long-term management. Memory clinics are sometimes the centre of a broad model of care, with preliminary home visits by a nurse and/or psychologist before clinic attendance and further home visits afterwards to discuss assessment results and plan future management.
In some countries, sometimes with government support, networks of clinics have developed to coordinate clinical, research and educational activity related to dementia. For example, in The Netherlands, memory clinics are well established and have led to the development of quality markers to facilitate description and comparison of activities and quality standards.8 Most Dutch clinics actively involve the general practitioner, routinely provide a home assessment visit and have a strong research emphasis. In France, the national Alzheimer Plan has supported a major effort to ensure that each health district has its own memory unit (Consultation Mémoire) for dementia diagnosis and follow-up, building upon the expert memory clinics developed in the 1990s. At a regional level there are specialist Centres Mémoire de Ressources et de Recherche (CMRR), providing diagnosis in the most complex cases and delivering research and training. Other initiatives have included use of standard assessment and follow-up documentation, common educational projects and multicentre clinical research projects.
In Switzerland there is a collaborative group of memory clinics, enabling an active programme of education and training for health professionals and clinical research. The primary care doctor plays an important role in initial assessment before comprehensive diagnosis and treatment recommendations are made in the memory clinic, including memory training and caregiver support activities. There is also close involvement with the national Alzheimer’s Association. The limited number of memory clinics in Germany and Austria are mainly university based and research oriented and are not covered by statutory health insurance, so have yet to become a standard component of local dementia care. In rural and isolated areas in Europe, the structures necessary to provide services are often lacking and novel approaches are therefore needed. For example, in Lapland there is a memory clinic bus which tours around offering memory testing and counselling services.
In the southern hemisphere, memory clinics providing multidisciplinary assessment and management for community-living people with dementia are developing in every continent, although still mainly based within the private sector or university centres in the larger cities. In Australia, a government-funded regional network of Cognitive, Dementia and Memory Services (CDAMS) were established in the 1990s across the state of Victoria, although elsewhere in the country the development of memory clinics has been more sporadic. The multicultural nature of Australian society presents particular challenges to ensure equity of assessment, service provision and utilization and highlights the need for clinics to be sensitive to the needs of people from a range of cultural and linguistic backgrounds,9 a challenge also being addressed in many clinics in North America and Southeast Asia.
Why The Need?
The worldwide growth in memory clinics has largely developed because of increasing demand and expectations of patients and families, frustrated by the difficulties of obtaining informed diagnosis and advice from existing services. They are not a replacement or alternative to these, but rather a more focused service providing a consistent approach to assessment, more specific diagnosis and a single resource for expert information and support (Table 72.1). Demographic changes are rapidly leading to greater numbers of patients with age-related cognitive disorders and there is appropriate reluctance to attribute forgetfulness merely to age. The growing awareness that memory failure is not inevitable and that effective intervention is available has led to a desire for comprehensive assessment, diagnosis, advice and treatment to be provided by professionals with specific expertise.
Table 72.1 Potential benefits of memory clinics.
| Benefits for patients and families |
| Non-stigmatizing, specialist resource breaking down potential barriers to recognition/diagnosis |
| Increases choice and improves patient experience and engagement |
| Expert multidisciplinary assessment and diagnosis of cognitive disorders |
| Ensures treatable conditions are not overlooked |
| Early identification of dementia and intervention |
| Anti-dementia drugs are effectively targeted, monitored and stopped as appropriate |
| Education and practical support for patients and carers |
| Empowers people with dementia while they are still able to maintain control over their lives |
| Provides advice on memory aids and memory training |
| Opportunities for counselling and psychosocial management |
| Improves quality of life by promoting and maintaining independence for as long as possible |
| Continuing care in the community may reduce need for institutionalization |
| Access to research studies |
| Benefits for service provision |
| Addresses growing demand for specialist diagnosis and treatment |
| Encourages earlier referral and multidisciplinary management |
| Develops awareness of dementia in primary care |
| Cost-effective way of significantly increasing the number of people able to be seen |
| Provides standardized assessment and diagnosis |
| Gateway to services |
| Efficient targeting and monitoring of scarce resources (including medication and psychosocial interventions) |
| Expertise in legal and ethical issues |
| Facilitates audit, planning and evaluation of services |
| Elective decisions may help to avoid crises in care |
| May reduce hospitalizations and lengths of stay |
| Postponement of institutionalization may reduce costs |
| Focus for professional education and research activity |
In many areas, existing services for diagnosis and management of memory disorders have been inadequate, with no clear professional responsibility and a widespread lack of specialist expertise and experience. There is a growing appreciation of the complexity of the needs of these patients and that optimal assessment and management requires a multidisciplinary rather than a monodisciplinary approach.
Even in expert hands, assessment and management of mild cognitive disturbance are not always straightforward, with a difficult differential diagnosis ranging from the trivial to the very serious and from the easily reversible to the irreversible. Not all forgetful old people have dementia and not all demented old people have AD (Table 72.2). Comprehensive assessment reduces the chances of inappropriate labelling. There is a multiplicity of available assessment tools and investigations and, without access to the definitive diagnostic test of histopathology, some informed selection needs to be made. Once a working diagnosis has been reached, there is also a wide spectrum of available medical, psychological and social interventions that require tailoring to the individual.
Table 72.2 Diagnoses to be considered in people presenting to memory clinics.
| Neurodegenerative dementias |
| Alzheimer’s disease |
| Dementia with Lewy bodies |
| Parkinson’s disease dementia |
| Fronto-temporal dementia |
| Frontal variant |
| Primary progressive aphasia |
| Semantic dementia |
| Parkinson’s-plus syndromes |
| Progressive supranuclear palsy |
| Corticobasal degeneration |
| Multiple system atrophy |
| Huntington’s disease |
| Mild cognitive impairment (MCI) |
| Amnestic single-domain MCI |
| Amnestic multi-domain MCI |
| Non-amnestic single-domain MCI |
| Non-amnestic multi-domain MCI |
| Vascular cognitive impairment |
| Single stroke |
| Strategic infarct |
| Multiple cortical infarction |
| Multiple subcortical lacunes |
| CADASIL |
| Cerebral amyloid angiopathy (CAA) |
| Haemodynamic dementia |
| Neurological |
| Tumour |
| Normal pressure hydrocephalus |
| Multiple sclerosis |
| Motor neurone disease |
| Paraneoplastic |
| Mitochondrial encephalopathies |
| Learning disability |
| Post-traumatic |
| Subdural haematoma |
| Post-head injury |
| Dementia pugilistica |
| Functional/psychiatric |
| Depression |
| Anxiety |
| Stress and overwork |
| Adjustment disorder |
| Delusional disorder |
| Alzheimer phobia |
| Drugs/toxins |
| Prescribed medication |
| Alcohol-related |
| Substance abuse |
| Endocrine/metabolic |
| Hypo-/hyperthyroidism |
| Hypo-/hyperparathyroidism |
| Hypo-/hyperadrenalism |
| Hepatic failure |
| Renal failure |
| Vitamin B12 deficiency |
| Thiamine deficiency/Korsakoff syndrome |
| Inflammatory |
| Rheumatoid cerebrovasculitis |
| Lupus cerebrovasculitis |
| Neurosarcoidosis |
| Infection |
| Post-encephalitis |
| HIV/AIDS |
| Neurosyphilis |
| Prion dementia (CJD) |
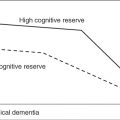
The availability of specific drug treatment for AD and some other dementias and the need to identify suitable patients and to monitor drug efficacy are the most obvious justifications for early diagnosis. However, the emphasis on a medical model of care and the perceived influence of the pharmaceutical industry in driving forward the expansion of memory clinics should not detract from the broader psychosocial benefits of early recognition and intervention.
Although reversible dementia is uncommon, nearly all patients will have problems that can be helped and appropriate intervention can be instigated at a stage when it is likely to be most effective. A positive diagnosis reduces the risk of inappropriate management and avoids wrong assumptions being made. It empowers people with dementia to become involved in decision-making while they are still able to do so. The opportunities for forward planning may improve the psychosocial health of carers and also help to lessen the risk of crises in care at a later stage. Certainly a proactive approach is likely to be more efficient and also more humane than one that is crisis driven.
Are They Effective?
In common with most health service developments, the rapid growth in memory clinics has occurred despite lack of evidence of effectiveness from randomized controlled comparisons with usual care. However, lack of evidence does not mean that they are ineffective and, given growing societal pressures and the considerable evidence on the effectiveness of the individual elements of memory clinics, the odds are in favour of their benefit.10 A recent model suggested that memory services need only achieve a modest increase in average quality of life of people with dementia, plus a 10% diversion of people with dementia from residential care, to be cost-effective.11 There is certainly evidence that community-living older people with cognitive impairment have fewer hospitalizations and nights hospitalized if their problem is diagnosed, compared with those who have never received such a diagnosis.12
Two completed randomized controlled trials have looked at the benefits of diagnosis of dementia in a memory clinic. A cluster randomized trial in The Netherlands showed that in comparison with usual care, an integrated multidisciplinary approach to dementia diagnosis in a hospital-based memory clinic setting increased health-related quality of life of the dementia patients for at least 12 months.13 An Australian trial looked at the quality of life for carers of community-dwelling patients with mild to moderate dementia, who were randomized to attend a memory clinic or act as a control group. Those carers attending the memory clinic were found to have significant improvement in psychosocial health-related quality of life, particularly in the domains of alertness behaviour and social interaction, which was maintained at 12 months. However, there was no significant improvement in carer burden or knowledge of dementia.14 The ongoing AD-Euro trial is comparing the clinical and cost effectiveness of post-diagnostic dementia guidance and treatment by memory clinics to usual care.15
Luce et al.16 compared consecutive referrals to the memory clinic in Newcastle upon Tyne with referrals to the traditional and well-established old age psychiatry service in the same city. Memory clinic patients were younger, had lower levels of cognitive impairment and a wider range of diagnoses, with those diagnosed as having dementia being at least 2 years earlier in the course of the disease than those seen in the standard service. The authors concluded that memory clinics target a distinct patient group compared with traditional old age psychiatry services, identifying cases of dementia much earlier and having the potential to make valuable contributions to patient care in terms of access to treatments, services and support networks and in terms of obtaining information and preparing for the future.
Another British study in the more rural area of Dorset17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree