MATERNAL COMPARTMENT—ENDOCRINE ALTERATIONS AND ENDOCRINE DISEASES ASSOCIATED WITH PREGNANCY
Various maternal adaptations involving the endocrine system occur during pregnancy. Also, many of the diseases of the female endocrine system, if untreated, are associated with infertility and reduced conception rates. If conception does occur, the more serious the disorder (such as diabetes mellitus), the more likely it will affect the fetus adversely (see Chap. 156). Hormones or drugs used to treat the endocrine disorders may be transported across the placenta and alter the environment and development of the fetus.
HYPOTHALAMUS AND PITUITARY GLAND
Little is known of the endocrine alterations of the maternal hypothalamus during pregnancy. Often, tumors of the hypothalamus or functional disorders of the hypothalamus cause infertility secondary to amenorrhea and chronic anovulation. The anterior
pituitary undergoes a two-fold to three-fold enlargement due primarily to hyperplasia and hypertrophy of the lactotropes (prolactin-secreting cells) thought to result from estrogen stimulation (see Chap. 13). Thus, plasma prolactin levels parallel the increase in pituitary size, with a progressive increase throughout gestation. Maternal prolactin levels in plasma are 10- to 20-fold higher at term than in nonpregnant women.111
pituitary undergoes a two-fold to three-fold enlargement due primarily to hyperplasia and hypertrophy of the lactotropes (prolactin-secreting cells) thought to result from estrogen stimulation (see Chap. 13). Thus, plasma prolactin levels parallel the increase in pituitary size, with a progressive increase throughout gestation. Maternal prolactin levels in plasma are 10- to 20-fold higher at term than in nonpregnant women.111
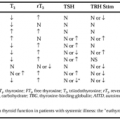
Contrary to lactotropes, the number of somatotrope cells in the pituitary decreases during pregnancy. Maternal levels of GH are low and do not change during pregnancy. The GH responses to insulin infusion appear blunted, suggesting that GH levels are suppressed.112 Maternal levels of LH and FSH are also low during pregnancy. The response of gonadotropins to an infusion of GnRH is blunted severely. The loss of responsiveness to GnRH is thought to be secondary to a negative feedback inhibition from the elevated levels of estrogen and progesterone.113 The levels of TSH are within the normal nonpregnant adult range. Furthermore, the response of TSH to a dose of TRH is similar to that in nonpregnant women.63
Numerous studies have examined the levels of ACTH- and POMC-related peptides in maternal blood throughout pregnancy. The maternal plasma levels of β-endorphin remain relatively low.114 These levels increase with advancing labor, but levels of this hormone in cord blood are similar both in infants delivered vaginally and in those delivered by elective cesarean section from women not in labor. However, fetal hypoxia is associated with significant increases in β-endorphin levels in cord blood.115 The plasma levels of maternal ACTH increase from early to late gestation.116 The slight increases in ACTH levels that appear to occur during gestation might be explained by the increased secretion of placental ACTH that is not subject to feedback control or related to the increased levels of CRH of placental origin. Maternal ACTH rises to very high levels during labor and delivery. The levels of ACTH in umbilical cord plasma parallel those of β-endorphin and, because neither cross the placenta, offer further evidence that in the fetus these two peptides are processed from a common precursor, as is true in the adult.
Maternal plasma AVP levels remain low throughout gestation and are not believed to play a role in human parturition.51 Maternal oxytocin levels are low and do not vary throughout pregnancy but increase during the later stages of labor (see Chap. 25 and Chap. 109).
Women with idiopathic hypopituitarism who lack one or more pituitary hormones will continue to require replacement therapy (thyroid hormones and glucocorticoids) throughout pregnancy. Because the size of the pituitary as well as its vascularization increases, vascular accidents are more likely than in nonpregnant women. Spontaneous pituitary necrosis, which is rare, occurs most commonly in diabetic women. The principal clinical feature is a persistent midline headache. The diagnosis is often difficult but can be confirmed by pituitary testing with TRH or CRH. Once the diagnosis is confirmed, adequate replacement will usually not be associated with further fetal or maternal morbidity. In some women, hypopituitarism develops after a postpartum hemorrhage, in which an acute ischemic necrosis of the pituitary may occur and cause hormone insufficiency (Sheehan syndrome; see Chap. 11 and Chap. 17). Finally, diabetes insipidus is a rare complication of pregnancy. Pregnant women who are treated with vasopressin replacement regimens appear to have no complications, and most treated women undergo spontaneous labor and delivery. Lactation occurs in some.117,118
The most common pituitary problem associated with pregnancy is growth of pituitary tumors, most commonly prolactinomas. Occasionally, women with small prolactinomas will become pregnant without treatment, but most will experience amenorrhea, galactorrhea, or infertility. Treatment with bromocriptine will increase the pregnancy rate in women with microprolactinomas or macroprolactinomas (see Chap. 13 and Chap. 21). After conception, most women with these disorders exhibit no problems during the remainder of pregnancy.119,120 The principal complications are headaches or visual disturbances secondary to tumor expansion, which usually respond rapidly to bromocriptine. The use of bromocriptine to induce ovulation or reinstitution of the drug during pregnancy does not appear to affect the fetus adversely.121
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree