Fig. 4.1
Diagnostic approach to adolescent hyperandrogenism
Table 4.1
Causes of adolescent hyperandrogenism
1. Polycystic ovarian syndrome |
2. Idiopathic hirsutism |
3. Nonclassical congenital adrenal hyperplasia |
4. Obesity |
5. Transient/idiopathic hyperandrogenism |
6. Adrenal: ovarian tumors |
7. Hyperprolactinemia |
8. Drugs |
Ovarian disorders, such as PCOS, hyperthecosis, ovarian tumors, and enzymatic defects such as 17-keto-reductase deficiency
Adrenal disorders, such as NCCAH, Cushing’s disease, or adrenal tumor
A mixed origin, such as hyperprolactinemia, stress, anorexia nervosa, and elite sport
A peripheral origin, such as obesity or idiopathic hirsutism
For the last 15 years, we have managed a cohort of 178 adolescent girls with HA in our pediatric endocrinology clinic. The causes of HA were as follows: PCOS (34 %), NCCAH (15 %), abdominal obesity (10 %), idiopathic hirsutism (9 %), elite sport (10 %), anorexia nervosa (6 %), transitory HA (11 %), 46,XY disorder of sex development (46,XY-DSD) (3 %), hyperprolactinemia (2 %), and endocrine tumors (1 %).
4.3.1 PCOS During Puberty
The long-term sequelae of PCOS are well known and continue to present challenges for endocrinologists and gynecologists, who need to make early diagnoses (in the pubertal period) so that these teenagers can be promptly treated both symptomatically and prophylactically. The striking trend toward adolescent obesity should reinforce our responsibilities. Menstrual irregularities in adolescents in the early postmenarcheal years can be an early sign of PCOS. In obese adolescents who subsequently develop glucose intolerance, there is an overall clinical impression that PCOS has become a prevalent cause of hyperandrogenism and menstrual disorders.
There is currently no consensual definition of adolescent PCOS [2]. We propose to define PCOS in the adolescent as the combination of four of the following criteria comprising the PCOS diagnosis (Fig. 4.2):
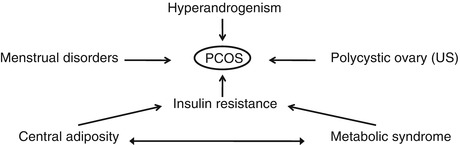
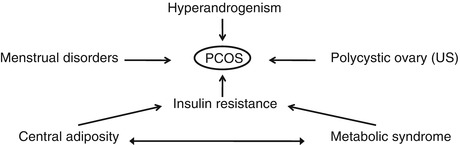
Fig. 4.2
Pathophysiology of PCOS
Clinical HA: persistent and severe acne and hirsutism (Ferriman score >10)
Oligo- or amenorrhea persisting 2 years postmenarche
Biochemical evidence of HA: T >50 ng/ml, along with dysovulation (LH/FSH ≥2)
Insulin resistance and hyperinsulinemia: visceral adiposity, acanthosis nigricans, and impaired glucose tolerance
Polycystic ovarian morphology on ultrasound
There are several clinical expressions of PCOS during adolescence [3]:
Postmenarcheal PCOS, the most common expression.
Premenarcheal PCOS.
Familial PCOS.
PCOS that occurs in adolescents previously diagnosed with central precocious puberty (CPP).
PCOS that occurs in adolescents previously diagnosed with intrauterine growth retardation (IUGR) and/or precocious pubarche.
Early metabolic expression: hyperinsulinism and insulin resistance are present in early puberty.
In certain elite sports, we have observed PCOS-like symptoms in a significant percentage of adolescent athletes (50 % vs 22 % in the control group) [4].
We propose screening for PCOS in all adolescents with oligo- or amenorrhea that persists 2 years after menarche, with particular attention given to those girls presenting obesity and a history of IUGR, premature pubarche, CPP, or familial history of PCOS.
Diagnosis of PCOS should be based on several criteria (Fig. 4.2):
Get Clinical Tree app for offline access

1.
Medical history
Birth weight (high or low)
Ethnic origin
Family history
Adrenarche = premature pubarche?
Lifestyle factors
2.
Physical examination
Degree and type of acne
Degree and type of hirsutism
Fat distribution (WHR: >70)
3.
Laboratory evaluation
Androgens: T, DHEAS
17-OH progesterone
LH (±FSH)
Fasting glucose/insulin
4.
Radiologic imaging