Fig. 3.1
Axial MRI images of the prostate: (a) Axial T2-weighted image of the prostate shows a large decreased signal intensity lesion in the right anterior mid-transitional zone (arrow). (b) DWI ADC map of the prostate shows restricted diffusion within this lesion (arrow). (c) DCE-MRI subtracted contrast image clearly outlines the lesion (arrow). (d) DCE-MRI color map overlay indicates that the lesion is hypervascular with rapid contrast wash-in and wash-out (arrow)
Owing to the detail of T2 imaging, it is the most helpful sequence for assessing local invasion into surrounding tissues. Detection of this local invasion has clinical relevance as it decreases the likelihood of cure from local therapy. Such invasion can be seen most overtly as direct invasion into the periprostatic fat. In addition, other findings suggestive of local invasion are irregularity of the gland margin, capsular bulge, and a low signal area within the seminal vesicles (which normally exhibit very high signal intensity). The results from such local staging predictions are not perfect, however, and absence of findings may occur in the setting of true disease with reports ranging with diagnostic sensitivity of 50–60 % [12, 13].
Diffusion-Weighted MRI
Diffusion-Weighted MRI (DW-MRI) sequences can detect and quantify the Brownian motion of water within tissue in vivo [14]. As this relates to cellular density, cell permeability, and free water diffusion within the interstitial spaces, DW-MRI can assess tissue structural architecture and differentiate benign tissue from malignant tissue. Benign tissue exhibits high signal intensity as it normally allows free water to diffuse with relative ease. In the malignant setting, relative higher nuclear:cytoplasmic ratio and loss of extracellular spaces due to cellular proliferation results in decreased free water diffusion and thus relative decreased signal intensity on DW-MRI [15]. Furthermore, DW-MRI findings have been significantly correlated to underlying histopathologic grade and clinical risk scores [16], which allows some prediction of tumor histopathologic behavior based on radiologic findings. Downsides of DW-MRI include its relatively poor spatial resolution (especially in comparison to T2-weighted MRI) which limits the ability to evaluate staging using this sequence in isolation. In addition, DW-MRI is more challenging to interpret in the central gland as the presence of BPH-associated nodules in this area of the prostate can mimic the low signal intensity of malignant lesions [17]. Despite this, addition of DW-MRI to standard anatomic T2-weighted imaging has been demonstrated to improved diagnostic accuracy [10].
Dynamic Contrast-Enhanced Magnetic Resonance Imaging
Dynamic Contrast-Enhanced Magnetic Resonance Imaging (DCE-MRI) allows assessment of tissue vascular supply. This is accomplished by acquiring T1-weighted images continuously before, throughout, and continuing after the injection of an MRI detectable contrast agent (i.e., gadolinium). Signal increase during this protocol results from blood supply to the tissue of interest. Differentiation between normal and malignant tissue is possible, as cancers have a typical imaging signature owing to their disordered angiogenesis. Malignant tissue is correlated with early uptake and early washout (temporal imaging) of vascular contrast [18]. These changes are most easily seen in larger lesions and in lesions which are of higher grade. In addition, similar to T2-weighted and DWI-MRI, lesions in the central gland are more challenging to differentiate as BPH nodules themselves can show early uptake, though they do not classically have the rapid washout typical of malignant lesions. DCE-MRI has been shown to have higher diagnostic power than T2W sequences alone, especially in lesions larger than 5 mm [19]. Similar to DWI, DCE-MRI sequences have relatively poor spatial resolution (in comparison to T2-weighted MRI) which limits the ability to evaluate staging using this sequence in isolation. However, it is felt to be most useful in assessment treatment effect in settings where the prostate gland remains in situ.
Magnetic Resonance Spectroscopic Imaging
Nuclear magnetic resonance spectroscopy is possible in situ using Magnetic Resonance Spectroscopic Imaging (MRSI) which allows relative quantification of metabolites within the tissue of interest. In this technique, the tissue of interest is divided into discrete areas (volumes of interest) known as voxels. For each voxel, a spectra of EM radiation is acquired which represents a fingerprint of the composition of the volume. This data can be used to differentiate benign from malignant tissue. Benign prostate typically harbors high levels of citrate, which can be detected as a specific peak on MRSI spectra. In the setting of cancer, the increased cellular turnover results in a relatively high concentration of choline, also detectable on the MRSI spectral curve. From this data, the relative concentration of choline:citrate can be calculated, with increased ratios signifying malignant changes. The addition of MRSI has been shown to improve diagnostic accuracy over T2-weighted imaging alone, with especially high specificity [20]. Some challenges to this technique are that inflammation can mimic citrate:choline signal changes, and that spatial resolution (similar to DWI and DCE-MRI) is not as good as T2-weighted MRI in the aid of local staging. In addition, some centers report that it is technically challenging and on some platforms it increases acquisition times limiting its widespread utilization.
MP-MRI: Combining Imaging Parameters for Improved Diagnostic Power
As each individual parameter is capturing orthogonal data, the combination of them has been demonstrated to have improved diagnostic power over each individual in isolation. Using careful histopathologic correlation of radical prostatectomy specimens, it has been demonstrated that a lesion identified has a positive predictive value of 98 %, with excellent sensitivity especially in larger lesions of clinical significance (>5 mm) [20].
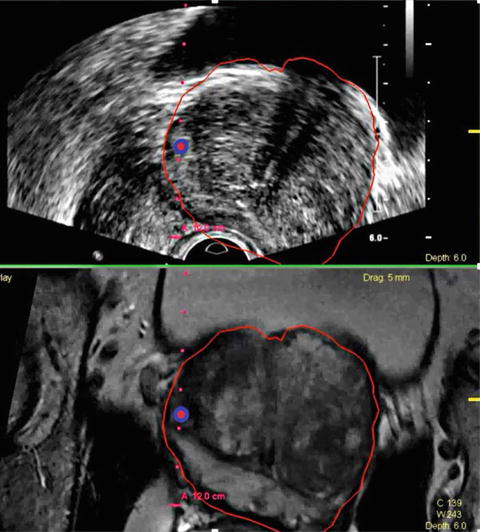
Harnessing the Diagnostic Power of MRI: MRI Targeted Biopsy
A number of strategies have been employed to take advantage of this additional diagnostic information from MRI. While in gantry biopsy has been performed to directly sample areas of suspicion, the added imaging time and need for specialized non-ferrous equipment makes it difficult to implement widely and in a cost-effective manner. Most contemporary strategies target areas of suspicion in an outpatient setting following a priori evaluation of MRI imaging by an experienced radiologist. The most popular methods employ software-based co-registration systems, known as fusion MRI-US biopsy (Fig 3.2). These systems utilize mechanically encoded biopsy arms or electromagnetic tracking to guide the needle to aforementioned areas of suspicion using software calculations which correlate MRI findings with real-time US data. Preliminary reports demonstrate excellent diagnostic power utilizing these strategies with improved sensitivity, specificity, and decreased upgrading rate [21]. In addition, manual targeting has been performed (so called “cognitive” biopsy), and in experienced hands, has been able to approximate the improved diagnostic power of computer-aided fusion-based systems [22].