CHAPTER 35 Loiasis
Epidemiology
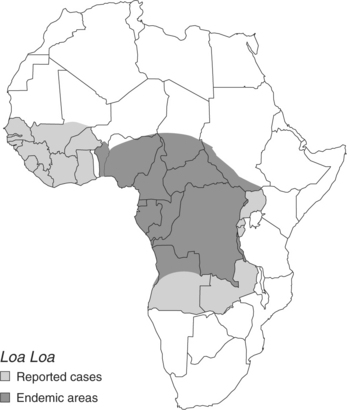
Loiasis occurs only in Africa, primarily in rainforest areas of Central and West Africa. Isolated cases have been reported in West Africa from Ghana to Guinea, and in Uganda, Malawi, Ethiopia, and Zambia (Fig. 35.1). Chronic infection may occur in 3–13 million residents of these endemic areas. Distribution of disease is affected by the predilection of the vector flies to reside in the forest canopy and lay their eggs in swamps and at river edges. The flies are attracted by movement, dark colors, and wood smoke. Rain forests, with relatively low canopies and scant undergrowth, seem to constitute a particularly desirable habitat for Chrysops flies.1–3 Infection rates are higher in adults than in children, and, in endemic areas, tend to be higher in males.
Etiology
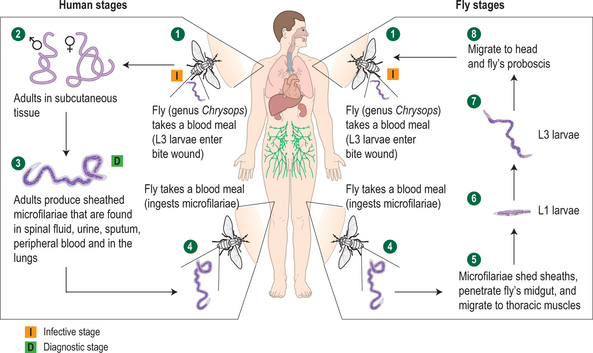
Chrysops silacea and Chrysops dimidiata are the most important vector species. Day-biting females inject larvae and pick up microfilariae of Loa in their blood meals. Larvae develop into adult worms in 6–12 months; adult worms may live up to two decades (Fig. 35.2). Adult worms migrate through subcutaneous tissue. Microfilariae are released into the bloodstream by adult female worms, but are found most commonly at midday, corresponding to the maximal biting time of the vector flies. Microfilaremia is seen less commonly in travelers or expatriates compared to individuals native to endemic areas.4
Clinical Manifestations
Adult worms may migrate under the conjunctiva, giving rise to the name eye worm for this infection. An intense conjunctivitis may accompany this migration, and most episodes resolve without sequelae. Worms may occasionally be seen migrating under the skin. Unlike the slow progress and intense itching of cutaneous larva migrans (caused by dog or cat hookworm larvae) migration of Loa loa is rapid and causes little or no reaction.2 Complications of infection with Loa loa include peripheral neuropathy, encephalopathy, and renal involvement. Peripheral neuropathy tends to occur in association with Calabar swelling and commonly presents as entrapment neuropathy. Encephalopathy occurs most often in the setting of significant microfilaremia and is most often seen following treatment. Microfilariae have been found in the spinal fluid. Encephalitis has also been associated with ivermectin treatment given in mass treatment programs for onchocerciasis.5 Renal involvement, usually hematuria or proteinuria with a clear sediment, occurs in as many as one-third of those infected. Transient worsening may occur with treatment but is almost always reversible; progression to renal failure is rare.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree