Abbreviations
| CT: | computed tomography |
| GIA: | gastrointestinal anastomosis |
| IVC: | inferior vena cava |
| SMA: | superior mesenteric artery |
Extended multivisceral resections involving the liver contribute to the armamentarium of an experienced liver surgeon.1 From to time-to-time the experienced liver surgeon is faced with a large tumor that requires an aggressive approach for complete resection.2 Each particular tumor that requires this type of resection is different with respect to the precise anatomy necessary to consider.3 This chapter presents four such radical resections which we have encountered in our Department of Surgery. We hope that depicting these resections in some detail might help assist other experienced liver surgeons in thinking through aggressive approaches to the resection of similar tumors in other patients. In other words we do not recommend that anyone necessarily follow the precise details of any of the descriptions below. Instead, we are providing only some organized approaches for particular cases.
 Preoperative Evaluation
Preoperative Evaluation
Initial evaluation of patients with large hepatic tumors should be aimed at determining the extent of invasion into adjacent structures and organs. In our institution we prefer the use of a spiral CT scan with i.v. contrast. We are usually able to determine vascular extension without further need for extra testing. In selected cases we complement this with a staging laparotomy and the use of intraoperative ultrasound.
We do not consider vascular invasion as a criterion for unresectability4; but it may determine the planned procedure: extensive resection versus transplantation. The evidence of multicentric disease that precludes an en bloc dissection is used as a contraindication for surgery.
Preoperative testing is particular to each institution but we recommend obtaining a baseline hemoglobin, liver function test, and coagulation profile. The evaluation of hepatic function is critical in patients with underlying cirrhosis. Severe liver disease (Child-Pugh’s class C) is considered a contraindication for major partial hepatic resection. We acknowledge that without the possibility of liver transplantation some of these resections will be impossible to perform and this may be a limiting factor in some institutions.
Special attention should be taken to correct any underlying coagulopathy. Blood, fresh frozen plasma and platelets should be available at the time of surgery. Extensive pulmonary and cardiac evaluation may be required at times and a good review of systems and past medical history are fundamental in making this determination.
 Surgical Technique
Surgical Technique
 Resection of Hepatic Tumor Involving the Vena Cava
Resection of Hepatic Tumor Involving the Vena Cava
This is a challenging problem that we have encountered with certain frequency. Even though their numbers may be small as a general group, in a very busy liver practice it may be encountered once or twice a year. This section describes the technique used in a young patient with a large hepatocellular tumor, which was invading the liver substance and the vena cava. We can’t emphasize enough the importance of good preoperative evaluation.
The patient is placed in a supine position. A right subcostal incision extending 2.5–3.0 cm above the xiphoid is performed. The incision can be extended to the left subcostal area if necessary. One of the most common mistakes made is limiting the exposure, which is why we advocate a generous incision. We very rarely use a thoracic extension, but this is a consideration for reoperative surgery or removal of tumors that extend above the diaphragm (Fig. 7.1).
Once the incision is made, we recommend a meticulous exploration to rule out extrahepatic disease or other concomitant pathology.
We usually remove the gallbladder as an initial maneuver; this facilitates the approach to the portal hilum and prevents the possibility of a second operation for gallbladder related problems in a scarred right upper quadrant.
The liver is subsequently mobilized. This begins with the division of the falciform ligament. The right and left triangular ligaments are divided as well, detaching the liver segments from the diaphragm. These maneuvers allow exposure to the suprahepatic vena cava, facilitating further vascular control when indicated. Care should be taken when incising the ligaments near the suprahepatic cava; the hepatic veins and diaphragmatic veins may be encountered superficially within these ligaments. Special attention should be directed to the examination of the gastrohepatic ligament when mobilizing the left lateral segment. Very often a large left hepatic artery originating from the left gastric artery can be found (Fig. 7.2).
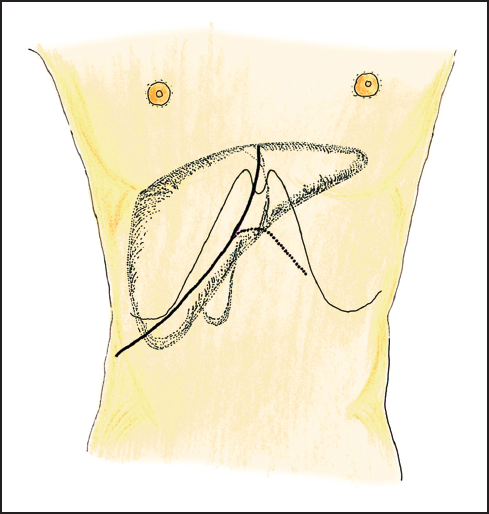
Fig. 7.1 Initial sub-costal incision for extended liver resection. The xiphoid extension may be optional.
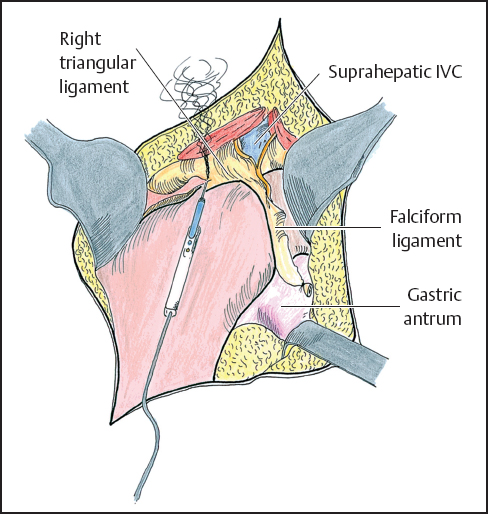
Fig. 7.2 The liver is mobilized dividing the triangular ligament and lateral attachment.
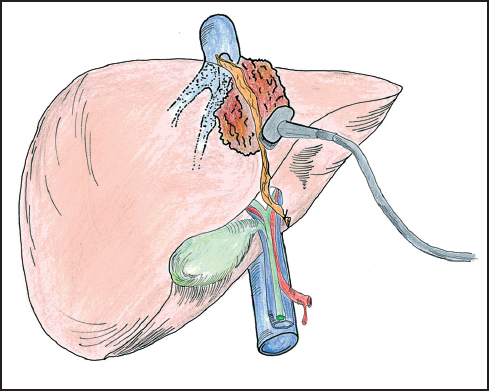
Fig. 7.3 Intraoperative ultrasonography is performed to localize the tumor and its relationship with the major structures.
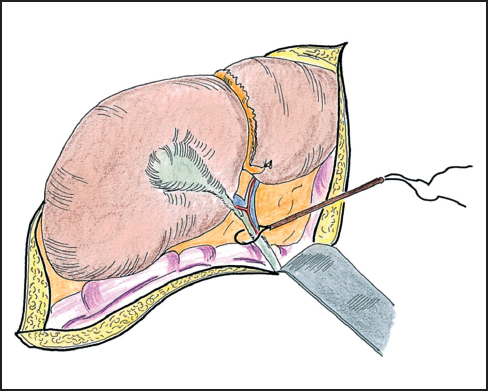
Fig. 7.4 The portal triad is secured using a Rummel tourniquet.
Once the liver is fully mobilized we evaluate the liver using intraoperative ultrasound. It is very important to determine the exact location of the tumor and its relation to the vascular structures. Tumors invading the IVC often arise from the posterior segments. Intraoperative ultrasound is more sensitive than any preoperative evaluation to determine the extent of these relationships and subsequent degree of invasion (Fig. 7.3).
We proceed to obtain control of the portal triad. This is a simple maneuver that should be performed without difficulty. The foramen of Winslow is identified and by placing a finger in the foramen and out through the gastrohepatic omentum, the portal triad is encircled. We prefer to use an umbilical tape to secure the portal triad. This procedure provides access for the subsequent Pringle maneuver when indicated. Traction can be applied using a Rummel tourniquet (Fig. 7.4).
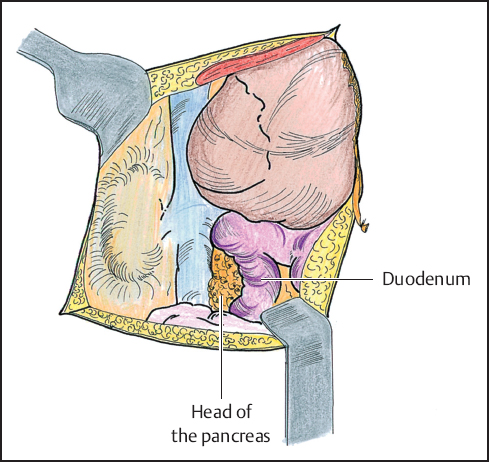
Fig. 7.5 A Kocher maneuver is performed to facilitate control of the IVC.
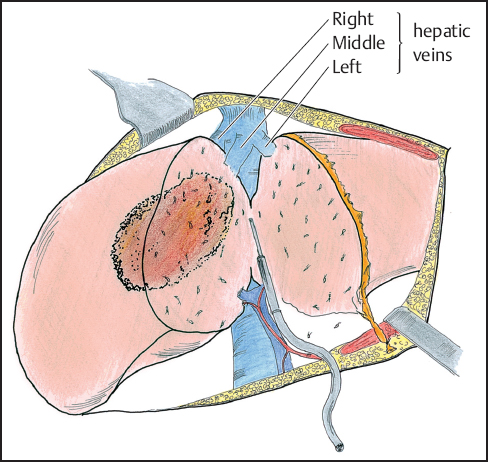
Fig. 7.6 The liver is divided using the ultrasonic dissector; at least 1 cm of margin is preserved around the tumor.
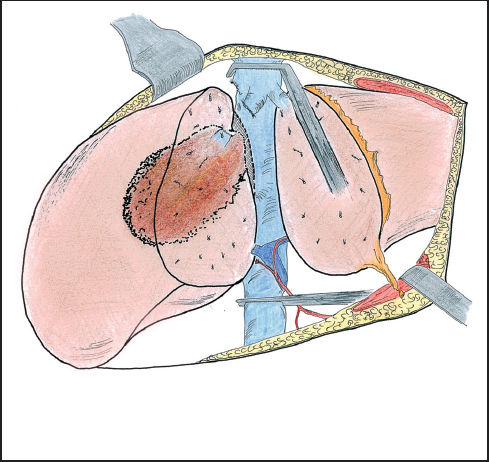
Fig. 7.7 The IVC attached to the tumor is removed en bloc.
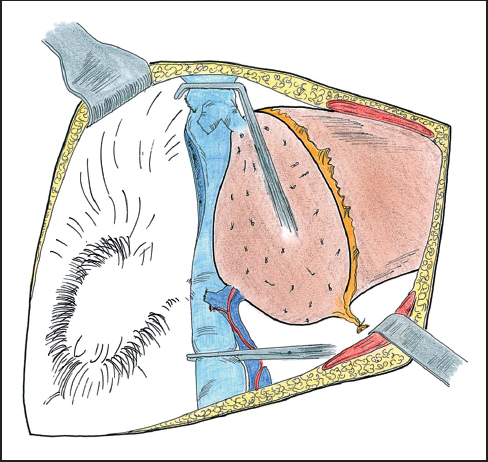
Fig. 7.8 Surgical field after specimen is removed.
In order to facilitate exposure and subsequent control of the infrahepatic vena cava a Kocher maneuver is performed. The IVC is exposed and suprarenal control is obtained (Fig. 7.5).
Once we have complete vascular control we are ready to start our hepatic dissection. This is going to be determined by the size of the tumor and its anatomic location within the different segments of the liver. We try to preserve as much healthy parenchyma as possible. We prefer to use the Cavitronic Ultra Sonographic Aspirator (CUSA) for our dissection, but finger fracture, clamp crushing, and the harmonic scalpel have been used. The intermittent Pringle maneuver can be used to limit bleeding and control bleeding vessels within the liver parenchyma. We limit portal occlusion to 15 to 20 minutes reserving its use only if necessary. This dissection can be meticulous and requires considerable practice. We try to preserve at least a 1 cm margin around the tumor (Fig. 7.6). We reserve the dissection of the tumor involving the IVC for the end. Once the entire tumor is dissected from the liver and it is only attached to the IVC, after performing the Pringle with the previously placed tourniquet, we proceed to perform proximal and distal clamping of the IVC. At this point the IVC is opened and the part attached to the tumor is resected. Any residual thrombus is removed as well (Fig. 7.7). The specimen is passed off the field and sent for pathologic examination. The surgical field is inspected (Fig. 7.8).
Depending on the size of the defect in the IVC, this can be primarily closed with continuous running 3–0 Prolene suture or equivalent suture. Attention should be taken not to narrow the lumen of the inferior vena cava but some degree of narrowing is acceptable (Fig. 7.9). Large defects can be repaired with a femoral or saphenous vein patch or synthetic material. Once the patch is sutured in place with nonabsorbable suture the proximal and distal control of the IVC is released.
Haemostasia of the remaining liver parenchyma is assured and any bleeding vessels are ligated. Cryoprecipitate glue or hemostatic agents may be used to reinforce hemostasis. A careful search for bile leakage is also accomplished. Drains are left in place and the incision is closed in layers (Fig. 7.10). We have seen some postoperative biliary leakage from the cut surface even after this was not detected at the operation. Severe leakage is usually treated expectantly with drains left in place as long as necessary.
 Resection for Tumors with Extensive Vascular Involvement using Autotransplantation
Resection for Tumors with Extensive Vascular Involvement using Autotransplantation
We describe below the resection of a large peripheral cholangiocarcinoma originating from the right hepatic duct but involving portal structures, inferior vena cava, and key structures of the left lateral segment. The patient mentioned was suffering from severe abdominal pain. Even though the cell type surprised us, nonetheless the relatively well differentiated tumor, as well as her young age seemed to warrant an aggressive approach. We currently perform similar autotransplantations safely.
The approach we choose for this resection is to perform the dissection on a back table after the liver has been completely removed. This technique requires a venovenous bypass while the liver is explanted or extracorporeal.
Similar to the previously described procedure the patient is placed in a supine position and a generous right subcostal incision extended above the xiphoid and into the left subcostal space is performed (Fig. 7.10). The liver is completely mobilized as is done for an extensive hepatic resection (Fig. 7.11).
The left axillary and left femoral region are also prepared and the left axillary vein and left femoral vein are exposed and cannulated in preparation for the venovenous bypass (Fig. 7.12).
The porta hepatis is dissected and the common bile duct is identified and divided with a 2.0 cm long stump (Fig. 7.13). The hepatic artery is dissected from the bifurcation to the take off of the gastroduodenal artery. Attention is paid to identify replaced right or left hepatic arteries. A generous segment of the portal vein is dissected as well. The supra- and infrahepatic vena cava are dissected. The latter is isolated between the adrenal and the renal vein (Fig. 7.14).
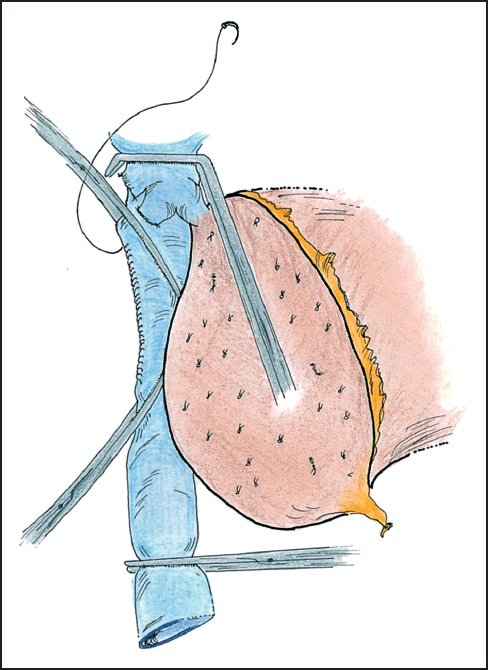
Fig. 7.9 The IVC can be primarily closed with Prolene suture. A large defect can be repaired with a synthetic or venous patch.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


