| Feature | Frequency (%) |
|---|---|
| Presentation can be subacute (>24 hours) | ~60 |
| Stiff neck is less common | 15–20 |
| Movement disorders (ataxia, tremors, myoclonus) are more common | 15–20 |
| Seizures are more common | ~25 |
| Fluctuating mental status is common | ~75 |
| Positive blood culture is more common | 50–75 |
| Cerebrospinal fluid (CSF) Positive Gram stain is less common Normal CSF glucose is more common Mononuclear cell predominance is more common | 30–40 >60 ~30 |
Brainstem encephalitis (rhombencephalitis)
An unusual form of listerial encephalitis involves the brainstem. In contrast to other listerial CNS infections, this illness usually occurs in healthy older children and adults; neonatal cases have not been reported. The typical clinical picture is one of a biphasic illness with a prodrome of fever, headache, nausea, and vomiting lasting about 4 days, followed by the abrupt onset of asymmetrical cranial nerve deficits, cerebellar signs, and hemiparesis or hemisensory deficits or both. Nuchal rigidity is present in about 50%, CSF is only mildly abnormal, and CSF culture is positive in about 40%; almost two-thirds are bacteremic. Respiratory failure develops in about 4% of cases. Magnetic resonance imaging is superior to computed tomography for demonstrating rhombencephalitis. Mortality is high, and serious sequelae are common in survivors.
Cerebritis and brain abscess
Parenchymal brain infection may occur without true abscess formation and is referred to as cerebritis; concomitant meningitis may or may not be present. Macroscopic brain abscesses account for about 10% of CNS listerial infections (Figure 144.1). Bacteremia is almost always present, and concomitant meningitis with isolation of L. monocytogenes from the CSF is found in 25%; both of these features are rare in other forms of bacterial brain abscess. About 50% of cases occur in known risk groups for listerial infection. Subcortical abscesses located in the thalamus, pons, and medulla are common; these sites are exceedingly rare when abscesses are due to other bacteria. Mortality is high, and survivors usually have serious sequelae.
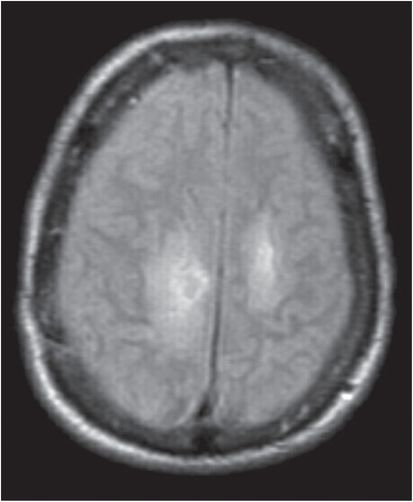
Figure 144.1 A magnetic resonance image (MRI) of the brain showing bilateral frontoparietal lesions with ring enhancement (abscess) on the right. The patient was a 70-year-old man with multiple myeloma who presented with difficulty walking followed by inability to stand and progressive quadriparesis. An aspirate of the abscess grew Listeria monocytogenes.
Endocarditis
Listerial endocarditis may account for as much as 7.5% of adult listerial infections, produces both native valve and prosthetic valve disease, and has a high rate of septic complications and a mortality of 48%. Listerial endocarditis, but not bacteremia per se, may be an indicator of underlying gastrointestinal tract pathology, including cancer.
Localized infection
Focal infections from which L. monocytogenes has been isolated include direct inoculation resulting in conjunctivitis, skin infection, and lymphadenitis. Bacteremia can lead to hepatic infection, cholecystitis, peritonitis, splenic abscess, pleuropulmonary infection, septic arthritis, osteomyelitis, pericarditis, myocarditis, arteritis, necrotizing fasciitis, and endophthalmitis. Complications, including disseminated intravascular coagulation, adult respiratory distress syndrome, and rhabdomyolysis with acute renal failure, have been documented. There is nothing clinically unique about these localized infections; many, but not all, have occurred in those known to be at risk for listeriosis. Joint infection typically involves prosthetic joints in compromised hosts and requires prosthesis removal for cure.
Febrile gastroenteritis
Many patients with invasive listeriosis give a history of antecedent gastrointestinal illness, often accompanied by fever. Although isolated cases of gastrointestinal illness due to L. monocytogenes appear to be quite rare, at least seven outbreaks of foodborne gastroenteritis due to L. monocytogenes have been documented. In the largest outbreak to date 1566 individuals, most of them children between the ages of 6 and 10, became ill after eating caterer-provided cafeteria food at two schools, and 19% were hospitalized. Illness typically occurs 24 hours after ingestion of a large inoculum of bacteria (range 6 hours to 10 days) and usually lasts 1 to 3 days (range 1–7 days); attack rates have been quite high (52%–100%). Common symptoms include fever, watery diarrhea, nausea, headache, and pains in joints and muscles. Vehicles of infection have included chocolate milk, cold corn and tuna salad, cold smoked trout, and delicatessen meat. Listeria monocytogenes should be considered to be a possible etiology in outbreaks of febrile gastroenteritis when routine cultures fail to yield a pathogen.
Diagnosis
Listeriosis should be a major consideration as part of the differential diagnosis in any of the following clinical settings:






