CHAPTER 34 Leprosy
Epidemiology
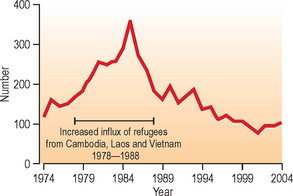
The US National Hansen’s Disease Programs (NHDP) registers approximately 150 new cases per year (Fig. 34.1), the majority of whom are immigrants from endemic countries, although native-born cases are reported from Texas and Louisiana, in particular.1
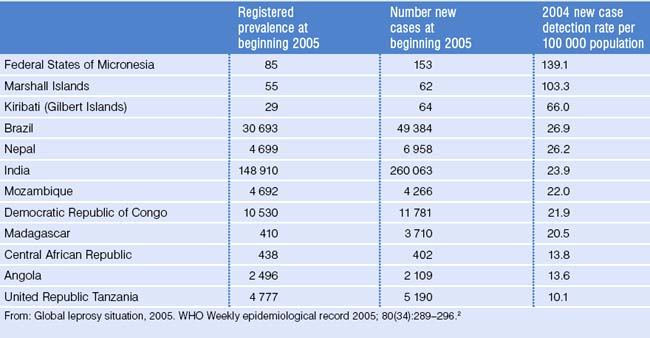
As a result of widespread implementation of multidrug treatment programs and policy changes that remove individuals from the roster of patients to be followed (both promulgated by the World Health Organization [WHO]), the available figures indicate a sharp decline in the prevalence of Hansen’s disease (HD) globally over the last two decades. WHO currently identifies nine major endemic countries (Angola, Brazil, Central African Republic, Democratic Republic of the Congo, India, Madagascar, Mozambique, Nepal, and the United Republic of Tanzania) contributing 84% of the new cases detected during 2004, and 74% of registered cases at the beginning of 2005. Globally, the registered prevalence of leprosy was 286 063 cases and the number of new cases detected during 2004 was 407 791, a 21% decrease comparing 2004 to 2003, mainly a result of a reduced number of new cases detected in India, where the detection declined by 29% as compared with 2003. While the majority of world leprosy cases come from India and Brazil, the most endemic areas remain the Federated States of Micronesia, Marshall Islands, and Kiribati, which continue to have the highest new case rate per population (Table 34.1).2
WHO pursues a public health goal of leprosy ‘elimination’ defined as a registered prevalence rate of less than 1 case per 10 000 population. However, a leprosy case is defined as a patient who has yet to receive a minimum therapeutic treatment, followed by his removal from the national case registry. This approach has led to a new cases rate higher than the annual registry prevalence in some countries. While paucibacillary (tuberculoid) cases may complete treatment by WHO regimens requiring only 6 months of medication, the removal of ‘treated’ patients from national registries has been highly controversial.3,4
Clinical Manifestations
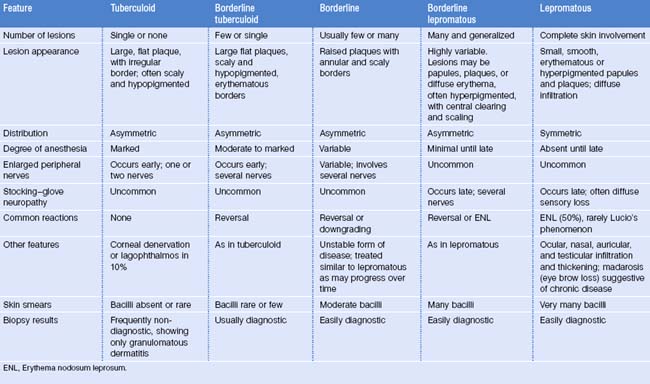
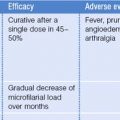
The clinical features of leprosy are a continuum between the tuberculoid and lepromatous forms of disease. There is substantial overlap in the appearance of the different forms, and careful assessment of clinical and histologic parameters is needed for accurate diagnosis. All clinical forms of leprosy must be correlated with findings on biopsies and skin smears. The disease types may be divided into paucibacillary forms (indeterminate, tuberculoid, and borderline tuberculoid) and multibacillary forms (borderline, borderline lepromatous, and lepromatous). These categories are useful for determining appropriate antibiotic therapy (Table 34.2).
Tuberculoid leprosy (TT) is a localized infection in a host with a high degree of cellular immunity. There is usually a single skin lesion or, at most, a few lesions. Lesions are large, flat plaques with well-demarcated, irregular, erythematous, raised borders and an atrophic, scaly center. Hypopigmentation is common, and there is marked anesthesia and anhydrosis of lesions. Plaques are frequently located on the face or extremities. Facial lesions are particularly associated with risk of underlying cranial nerve infiltration and injury, resulting in lifelong disability (Fig. 34.2).

Fig. 34.2 Tuberculoid leprosy: Picture of hypopigmented anesthetic patch on lateral aspect of eye.
(Picture courtesy of Barbara Stryjewska, MD, NHDP, Baton Rouge, LA.)
Neural involvement is usually confined to the area of skin lesions, with palpably enlarged peripheral nerves and motor, sensory, and autonomic deficits (Fig. 34.3). Neuropathy may develop without apparent skin lesions in a subset of tuberculoid leprosy termed pure neuritic. Testicular and ocular infiltration does not occur, although neuropathy can cause corneal denervation, lagophthalmos, and exposure keratitis. Reactional states do not occur in pure tuberculoid leprosy.
Borderline tuberculoid leprosy (BT) patients may closely resemble tuberculoid patients, but have slightly lower host immunity and a higher bacillary load. There are usually several lesions that are smaller and less flat than tuberculoid lesions. Lesions are distributed asymmetrically and are moderately to markedly anesthetic. There may be more than one area of neural involvement. Biopsy shows few bacilli, rather than the rare or absent bacilli characteristic of true tuberculoid cases. Skin smears show few or no bacilli. Reversal (type 1) reactions (movement toward the tuberculoid pole of disease) may occur (Fig. 34.4).

Fig. 34.4 Borderline tuberculoid. Erythematous macular-papular lesions on thigh exhibiting hair loss.
Borderline, or dimorphous, leprosy (BB) is regarded as an unstable form that may move toward either polar form. Patients have moderate numbers of lesions, usually more than 10, of variable morphology. Some lesions resemble the large, irregular, flat plaques of tuberculoid leprosy, while others are smaller and infiltrated or raised. Annular, or ring-shaped, lesions are typical, and lesions are asymmetrically distributed. Neural involvement may occur early or late, involves multiple nerves, and may be severe. Reversal and downgrading reactions may occur with alterations of cell-mediated immunity to M. leprae antigens; they represent changes toward the tuberculoid and lepromatous poles, respectively. The most severe neurologic damage occurs in borderline patients because of the many nerves involved and the tendency for neuritis to occur with reactions. Biopsy and smears show a moderate bacillary load.
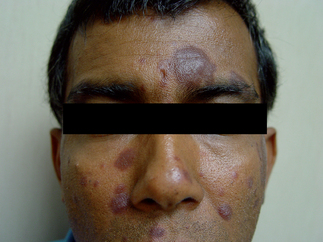
Borderline lepromatous leprosy (BL) patients resemble lepromatous patients but have fewer bacilli and higher immunity. Skin lesions are usually numerous and may be macules, papules, plaques, or nodules (Figs 34.5, 34.7). Some plaques may appear punched out with a sloping outer margin and a steep inner margin. Nerve involvement occurs late and sensation is often preserved. BL leprosy patients are unique in being susceptible to both type 1 reversal reactions and erythema nodosum leprosum (ENL).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree