6 Late effects of cancer treatment and survivorship
Medical late effects
Late effects are dependent upon the original cancer, its treatment, the family genetics and the developmental stage of the individual when treated for cancer. Box 6.1 lists some of the major effects that can occur.
Box 6.1
Medical late effects of treatment
| Second malignancy | e.g. leukaemia, sarcoma |
| Chronic health conditions | e.g. breathlessness, fatigue |
| Cardiological | e.g. arrhythmias |
| Neurological | e.g. peripheral neuropathy |
| Pulmonary | e.g. fibrosis |
| Endocrine | e.g. GH deficiency |
| Fertility | e.g. premature ovarian failure |
| Bone | e.g. osteoporosis |
| Renal | e.g. hypomagnesaemia |
Second malignancy
Second malignancies are the second most common cause of death (after the primary cancer) in those diagnosed with cancer, and can either be a solid tumour or haematological (leukaemia or myelodysplastic syndromes). The risk of second malignancy is increased with combinations of chemotherapy and radiotherapy but is also dependent upon the underlying genetics of the individual and the sensitivity of the tissue irradiated (Table 6.1).
Table 6.1 The most common second malignancy after treatment for cancer and some of the identified or proposed causative agents
| Type of secondary malignancy | Identified or potential risk factors |
|---|---|
| Leukaemia | Chemotherapy, e.g. etoposide, anthracyclines |
| Sarcoma | |
| Lung | |
| Breast | Radiotherapy, e.g. mantle or hemithorax especially if given in late teens or early twenties (up to 4–7 times the standardized mortality ratio) |
| Uterine | Tamoxifen (risk 1 in 100,000), increased in those with HNPCC |
| Colorectal | Pelvic or abdominal radiotherapy |
| Bladder |
In general secondary solid tumours arise in sites of previous radiotherapy, especially if chemotherapy was also given. The total dose of radiotherapy delivered as well as the type and energy of the treatment and treated volume determine the risk. The tissues most likely to give rise to a secondary malignancy following radiotherapy are bone marrow, thyroid, breast and soft tissues (sarcomas) (Box 6.2).
Box 6.2
Learning points
Leukaemias and myelodysplastic syndromes have been found to relate to previous chemotherapy treatment, especially with etoposide, anthracyclines and alkylating agents. These leukaemias are characterized by a chromosomal abnormality at 11q23, tend to occur within 2 years of primary treatment and have a poor prognosis. Intensive regimens for Ewing’s sarcoma or rhabdomyosarcoma have a risk of up to 20% at 20 years of secondary haematological malignancy. Myelodysplastic syndromes have been associated with previous alkylating agents.
Example box 6.1
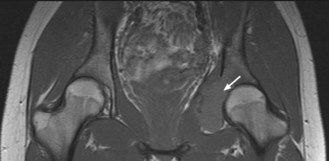
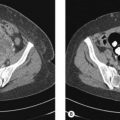
A 21-year-old woman was treated for Ewing’s sarcoma of the right pelvis with neoadjuvant chemotherapy, debulking surgery, radiotherapy and further chemotherapy. She had a good response to treatment with only a small mass remaining which remained stable on CT scans for 5 years. With increasing symptoms of pelvic and groin pain at 8 years an X-ray then MRI was performed which showed a mass in the left acetabulum (Figure 6.1). The appearance of the mass was not typical for a Ewing’s sarcoma and a biopsy was performed. The pathology showed an osteosarcoma. Despite staging showing no distant disease and treatment with chemotherapy, the tumour progressed rapidly, lung metastases developed and the patient died within a year.
Infertility
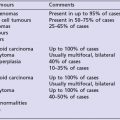
Infertility as a consequence of cancer or its treatment remains a significant issue for young people who have not yet completed their families (Figure 6.2). The risk depends on the gender of the patient and the type of therapy administered as well as the type of cancer (Box 6.3). Overall the fertility of childhood cancer survivors when compared with their siblings is 0.76 for men and 0.93 for women.
Box 6.3
Risk of infertility in cancer survivors
The greatest risk to fertility in adult survivors is
In the UK, guidelines have been developed by a working party to highlight possible management strategies and risks of infertility with different cancer treatments (Box 6.4). These are available from the Royal College of Radiologist website (http://www.rcr.ac.uk/publications.aspx?PageID=149&PublicationID=269).