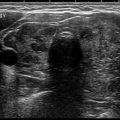
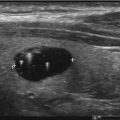
Fig. 3.1
Thyrotropin-releasing hormone (TRH) is secreted by the hypothalamus which stimulates thyrotropin-secreting hormone (TSH); TSH secretion by the pituitary gland stimulates thyroid hormone production. The thyroid gland produces thyroxine (T4) and triiodothyronine (T3) in the approximate proportion of 80% and 20% respectively. All circulating T4 is produced in the thyroid gland while most T3 is produced peripherally. T4 and T3 inhibit further secretion of TRH and TSH, by a negative feedback system, preventing excessive production and secretion of these hormones thus maintaining homeostatic balance
The thyroid gland possesses two different cell lines. Follicular cells produce T4 and T3, while parafollicular cells (C cells) produce calcitonin. T4 and T3 are critical for many bodily functions including the cardiovascular system, linear growth, thermoregulation, nutrient and hepatic metabolism, and fluid balance [10]. While T4 is exclusively produced in the thyroid gland, the majority of T3 (~80%), the biologically active form of thyroid hormone, is produced by extrathyroidal tissue by monodeiodination of T4 [11–13]. Serum concentrations of T4 and T3 modulate the secretion of TRH and TSH in a negative feedback fashion leading to a homeostatic balance of circulator hormones (Fig. 3.1).
Calcitonin assists in lowering elevated circulating serum calcium levels by directly inhibiting osteoclastic bone resorption [14] and inhibits intestinal calcium absorption and renal tubular calcium reabsorption [15].
Laboratory Monitoring
TSH
Thyroid hormones, the major determinant of the basal metabolic rate, are tightly regulated [16]. To maintain balance, TSH , which stimulates production of T4 and T3, is steadily secreted with minimal fluctuations in a normal individual [17, 18]. This stable state is known as the “set point” [19, 20] and thought to be genetically linked [21, 22]. While stable within an individual, a wide variability is seen among different individuals with each having his/her own set point [17] explaining the wide TSH reference range seen in laboratories (Table 3.1). A healthy individual will therefore maintain a “personalized” TSH target concentration for optimal metabolic activity [23].
Table 3.1
Reference rages for thyroid function tests
Age | Reference limits | |
|---|---|---|
TSH | Adult | 0.4–4.0 mIU/dL |
Total T4 | >Or = 20 years | 58–160 nmol/L (4.5–11.7 mcg/dL) |
Total T3 | >Or = 20 years | 0.9–2.8 nmol/L (80–200 ng/dL) |
Free T4 | >Or = 20 | 10–23 pmol/L (0.9–1.7 ng/dL) |
Free T3 | >1 year | 3.5–6.5 pmol/L (2.8–4.4 pg/mL) |
When evaluating patients with thyroid nodules, serum TSH, a sensitive and accurate test of thyroid function, should be the initial test [24]. Assays used to measure TSH have improved significantly over the decades. The original radioimmunoassay (RIA) method [25–27] was unable to measure lower limits of TSH required to identify hyperthyroidism and was abandoned for the newer “ultrasensitive” immunometric assay (IMA) , able to detect TSH levels to 0.01–0.02 mIU/L [28]. The IMA method, able to detect the hyperthyroid state, is currently employed in most labs today.
There are different non-thyroid-related medical conditions and drugs which can influence TSH levels. Some of these drugs include glucocorticoids, somatostatin, and dopamine agonist which can suppress TSH secretion, with or without causing changes in thyroxine levels [29, 30]. Table 3.2 gives a list of some medications that affect TSH measurements [29–32]. Medical conditions such as pregnancy can also affect TSH levels in the first trimester due to human chorionic gonadotropin (hCG) stimulation of the TSH receptor, which eventually normalizes later in pregnancy [33–35]. Therefore, knowledge of current medications and medical conditions affecting TSH should be taken into account when evaluating TSH levels.
Drugs | Effect on thyroid-stimulating hormone (TSH) |
|---|---|
Glucocorticoid | Suppress TSH stimulation with or without causing clinical central hypothyroidism |
Dopamine/bromocriptine | |
Somatostatin | |
Rexinoid | |
Amphetamine | |
Metformin | Decreases TSH in those with TSH > 2.5mIU/L |
Metyrapone | Leads to increased TSH without effect on T3 or T4 levels |
Amiodarone | Increased TSH by up to 2.7× the normal level with and elevation in T4 and slight fall in T3 |
TSH normal limits are also an area of debate. While many laboratories give a reference range between 0.5 and 5.0 mUI/L, population studies suggest that TSH levels can be affected by ethnicity, iodine intake, gender, and body mass index [36]. The National Health and Nutrition Examination Survey (NHANES) III, a United States (US) population-based study, showed that the serum TSH upper limit of normal was lower in African Americans (3.6 mIU/L) than in Mexican Americans (4.2 mIU/L) [36] and that the upper limit of normal for those 20–29 years old was lower (3.5 mIU/L) than in those over 80 (7.5 mIU/L) [37]. Based on the NHANES III study, it was also suggested that 95% of the US population, without self-history or family history of thyroid disease, had a normal serum TSH concentration between 0.45 and 4.12 mIU/L [36]. The National Academy of Clinical Biochemistry (NACB) , on the other hand, states that the upper limit of normal TSH is around 2.5 mIU/L and that values between 2.5 and 4 mIU/L are likely individuals with incipient autoimmune thyroid disease who should undergo ultrasonography to further characterize the thyroid gland [24, 38]. Some recommend using a lower upper limit of serum TSH, as it will better identify incipient hypothyroidism [39], while others feel the current upper limit, while potentially missing incipient disease, does not correspond to adverse health consequences if left untreated, thus not justifying adjusting current limits [40]. While an age-based TSH reference is ideal, in its absence, the American Thyroid Association (ATA) and the American Association of Clinical Endocrinologists (AACE) recommended the use of a normal TSH reference range between 0.4 and 4.0 mIU/L [41, 42] as noted in Table 3.1.
In terms of nodular disease, a patient with a TSH within the normal reference limits does not require further laboratory work-up but will need an ultrasound, possibly followed by FNA to further characterize the nodule. When initial TSH is either elevated or suppressed, further work-up to distinguish between overt disease (free T4 (FT4) above or below normal limits) and subclinical disease (FT4 within normal limits) is necessary. This is accomplished by measuring serum FT4 and, in some instances, serum T3 concentrations.
T4 and T3
In circulation, T4 and T3 are predominantly bound to thyroxine-binding globulin (60–75%) (TBG), transthyretin (15–30%), and albumin (~10%) [43]. These proteins assist in distributing the hormones evenly throughout the body [44, 45], buffer tissues from possible sudden influx or cessation of hormone secretion from the thyroid gland [46, 47], and are capable of increasing or decreasing affinity to thyroid hormone at specific sites depending on tissue demand [48]. While T4 is found in serum concentrations around tenfold higher than T3 [10], the vast majority of T4 is protein bound with 0.02% circulating in the unbound, free form compared to 0.2% of free T3 [47]. Theoretically, it is much easier to measure circulating total T4 (TT4) (free + bound T4) and total T3 (TT3) (free + bound T3) due to higher nanomolar concentrations compared to the significantly lower picomolar concentrations of FT4 and FT3 (Table 3.1) [49–51]. TT4 and TT3, measured using liquid chromatography-tandem mass spectrometry (LC-MS/MS) methods , are fairly accurate, precise, and specific [52], but not always reliable as stand-alone tests due to factors disrupting binding protein concentrations [53]; thus, reports may be falsely above or below reference ranges, inaccurately suggesting thyroid disease. A list of different medications and pathophysiologic conditions leading to high or low TBG levels can be found in Table 3.3. For this reason, if measuring TT4, testing should include TBG levels or an estimate of binding proteins to calculate a free hormone index to account for possible binding protein effects [54–56]. For this reason, total T4 is less frequently used nowadays.
TBG increase | TBG decrease | |
|---|---|---|
Drugs | Estrogen | Androgen |
Tamoxifen | Anabolic steroids | |
Mitotane | Glucocorticoids | |
Heroin | Nicotinic acid | |
Nicotinic acid | Lithium | |
Phenytoin | ||
Propranolol | ||
Pathophysiologic conditions | Pregnancy | Hyperthyroidism |
Hypothyroidism | Critical illness | |
Acute/chronic liver disease | Sepsis | |
Adrenal insufficiency | Nephrotic syndrome | |
AIDS | Diabetic ketoacidosis | |
Chronic alcoholism | ||
Acromegaly | ||
Cushing’s syndrome | ||
Familial/congenital conditions | TBG excess | Familial TBG deficiency |
Since the free or unbound hormone is responsible for the cellular biological activity [57], free hormone levels should reflect biological effects better than total hormone levels. Unfortunately, due to very low serum concentrations, accurate testing of FT4 and FT3 has proved technically difficult with modern day testing methods. Currently, two methods are available to measure free hormone levels (Table 3.4): the direct method (i.e., equilibrium dialysis, ultrafiltration), which physically separates free hormone from protein-bound hormone [58, 59], and estimate testing (i.e., two-test index method, free thyroid hormone immunoassay method), which physically separates free hormone from protein-bound hormone before measuring free hormone levels by sensitive immunoassay, or, antibody is used to immunoextract a proportion of free hormone out of the specimen before quantitation [60–62]. While these tests are widely used, neither method is free of problems. The direct method can be influenced by endogenous binding protein inhibitors, dilution, and temperature [63, 64] leading to falsely elevated or suppressed results, while estimate testing is protein dependent and prone to over- or underestimation if a significant abnormality exists in binding proteins [61, 60, 65]. Drugs, such as those noted in Table 3.5, can also affect FT4 measurements [66–68]. Thus, a single test method has not been universally validated for all clinical situations. Currently, laboratories use automated immunoassays to estimate FT4 and FT3 levels. Direct free hormone testing methods need special request and should be ordered when FT4 immunoassay reports seem discordant with TSH.
Table 3.4
Current methods used in different laboratories to measure free thyroxine (FT4) and free triiodothyronine (FT3)
• Estimation FT4/FT3 testing |
Two–test index method: |
– TBG immunoassay |
– Thyroid hormone-binding ratio/“uptake” test |
– Isotropic index method |
Free hormone immunoassay method: |
– Two-step, labeled hormone/back titration FT4 and FT3 method |
– One-step, labeled hormone-analog FT4 and FT3 method |
– Labeled antibody FT4 and FT3 method |
• Direct FT4/FT3 testing |
– Equilibrium dialysis |
– Ultrafiltration |
– Gel absorption |
In the ambulatory setting, when evaluating someone with a thyroid nodule, FT4 is more often ordered than TT4 due to the risk of binding protein effects in TT4 measurements (Table 3.3). Thus, a low TSH, suggestive of hyperthyroidism, should be followed by FT4 measurement which, if elevated, suggests thyrotoxicosis. When associated with thyroid nodular disease, diagnosis may include either an autonomous functioning nodule, a toxic multinodular goiter, or a hyperfunctioning gland with non-functional nodules. A radioisotope scan and uptake will help distinguish one from the other [69].
Thyroperoxidase Antibody (TPO)
While an elevated TSH suggests hypothyroidism, FT4 will differentiate between overt (high TSH/low FT4) and subclinical hypothyroidism (high TSH/normal FT4). Thyroperoxidase antibody (TPOAb) is an autoantibody targeting the immunodominant region of the globular glycoprotein, thyroperoxidase, expressed on the apical surface of thyrocytes. TPOAb is helpful in identifying autoimmune-mediated disease and is rarely associated with thyroid malignancy [70]. Thus, TPOAb should be tested in subjects suspected of autoimmune thyroid disease (Hashimoto), especially in the setting of a nodular goiter, and not to assist in determining malignancy risks [71]. Higher values indicate more active and more extensive disease.
An association between Hashimoto’s thyroiditis (HT) and papillary thyroid cancer (PTC) has been the subject of long-standing debate [72–79]. More notably, aggressive disease (i.e., regional lymph node metastasis) has been suggested in patients with concurrent HT and PTC [80, 81], but not uniformly reported [82, 83]. One theory behind the connection of HT and PTC is the high expression of oncogenes (i.e., RET/PTC) found in patients with HT [82, 84] and in those with PTC [85]. Recent studies show this to be an unlikely association [86, 87], and we therefore recommend against routine screening of all subjects with nodular disease for HT, unless evidence suggests a concurrent autoimmune thyroid disease.
Some reports show that higher TSH levels are associated with an increased risk of malignancy in thyroid nodules in the absence of autoimmune disease [88–90]. It should be noted, however, that serum TSH tends to increase with age [36, 37, 91] and that approximately 3–16% of individuals over the age of 60 have elevated TSH with normal FT4 (subclinical hypothyroidism) [92]. A US population study showed that those over the age of 80, without thyroid disease, can have a normal upper TSH limit of 7.5 mIU/L [37]. Thus, in the elderly, additional information (i.e., ultrasound features) should be considered when determining malignancy risks and the need for biopsy. It should be emphasized that elevated TSH increases the risk of nodular malignancy in the pediatric population [93], and since this group possesses a higher risk of malignancy [94], an elevated TSH should be followed with biopsy in the setting of a nodular thyroid gland.
Thyroglobulin (Tg)
Serum thyroglobulin (Tg) , a dimeric protein produced by thyroid follicular cells, is measured by automated IMA in many centers (though the older isotopic RIA is still in use) and correlates with iodine intake and thyroid volume rather than the nature or function of a nodule [95]. While a useful marker in patients with differentiated thyroid cancer post-thyroidectomy, it offers no diagnostic value when evaluating malignancy risks of a nodular thyroid and, thus, should not be measured during the routine evaluation of a thyroid nodule.
Calcitonin (Ct)
Serum calcitonin (Ct) , a 32-amino acid linear polypeptide hormone produced by thyroid parafollicular (aka C cells) in response to elevated calcium levels, is a useful marker for medullary thyroid carcinoma (MTC) and correlates with tumor burden [96]. MTC is found in 3–10% of all thyroid malignancies [97, 98]. Studies attempting to show value in routine screening for MTC with Ct have not been convincing. For example, a study screening for MTC by Ct in over 10,800 subjects with nodular thyroid disease identified an MTC prevalence of 0.4% [99]. Another screening study of 5817 subjects found a similar MTC prevalence of 0.3% [100]. Stimulation by pentagastrin, a synthetic polypeptide, was used in these studies to increase specificity but is unavailable in most countries nowadays. Caveats of these studies is that though while they detected MTC at earlier stages of disease, they also detected C-cell hyperplasia (CCH) , a preneoplastic lesion in familial forms of MTC, but not shown to undergo malignant transformation in sporadic forms of MTC [100, 101]. The prevalence of CCH in one study of 57 subjects without thyroid malignancy was found to be as high as 50% [102]. Thus, CCH detection increases risks of false positives leading to unnecessary thyroidectomies. Ct has also been shown to be elevated in a variety of nonthyroidal diseases (i.e., pulmonary endocrine tumors, renal failure, hypergastrinemia, alcohol use, and smoking [103, 104]), which should be considered if Ct is used to screen for MTC.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree