12.1 Introduction
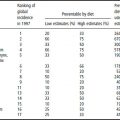
The epidemiology of iodine deficiency disorders (IDD) is currently in a transitional phase because of the great progress seen during the 1990s in the battle against IDD, mainly in the form of national salt iodization programs. In 1999, the World Health Organization (WHO) estimated that, of its 191 member states, 130 had a significant IDD problem, with a total of 740 million people affected by goiter, or 13% of the world’s total population. In 1999, of the 130 countries with IDD, 98 (75%) had legislation on salt iodization in place, and a further 12 had it in draft form. Following the promulgation of legislation on salt and the sensitization of the salt industry, there has been an enormous increase in the consumption of iodized salt, leading to a reduction in the goiter rates. The latest available data on the magnitude of IDD is indicated by the goiter rates in the different regions: 20% in Africa, 5% in America, 12% in south-east Asia, 32% in the eastern Mediterranean, 15% in Europe and 8% in the western Pacific. In 1999, the number of people at risk of iodine deficiency had probably been reduced to approximately 500 million.
12.2 Definition of iodine deficiency
The diagnosis of iodine deficiency should be seen as a group, community or population diagnosis rather than an assessment on the individual level. Although the relevant measurements are done on individuals, the summary data of the group are used for interpretation of IDD status. It is well known that biological variation, due to varying levels of hydration, could occur in the concentration of urinary iodine of different individuals. It is also known that interobserver variation is likely to exist where more than one observer performs palpation of the thyroid glands of a group of individuals. To reduce the effect of interindividual and intraindividual observer variation, sufficient sample sizes and thorough training of observers are required for valid estimates of prevalence rates.
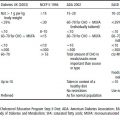
At a consultation by the WHO, the United Nations Children’s Fund and the International Council for Control of Iodine Deficiency Disorders (ICCIDD), held in May 1999 in Geneva, the following outcome indicators were recommended for the assessment of IDD and their elimination.
Table 12.1 Definition of iodine status of a population based on median urinary iodine concentration
| Iodine status | Median urinary iodine concentration (μg/l) |
| Severe iodine deficiency | <20 |
| Moderate iodine deficiency | 20–49 |
| Mild iodine deficiency | 50–99 |
| Ideal iodine intake | 100–200 |
| More than adequate iodine intake: may pose increased risk of iodine-induced hyperthyroidism | 201–299 |
| Excessive iodine intake | >300 |
Urinary iodine excretion
Urinary iodine excretion provides a good indication of recent dietary iodine intake. A sample size of at least 30 individuals will compensate for the individual variation in iodine concentration that may occur. A casual or spot urine sample should be taken in an iodine-free container, tightly sealed and stored until analysis. Great care should be taken to avoid contamination during the whole sample collection and analysis procedure.
Most laboratories use the Sandell–Kolthoff reaction in the analysis of urinary iodine, and it is advisable for laboratories to participate in quality assurance programs to ensure accurate results. It is not necessary to relate the urinary iodine to creatinine excretion. The cut-off points for defining the iodine status of a population according to the median urinary iodine concentration are given in Table 12.1.
As urinary iodine values from populations are usually not normally distributed, the frequency distributions are necessary for correct interpretation of data, and the median value should be used rather than the mean value.
For the elimination of iodine deficiency it is required that the median urinary iodine concentration should be 100 μg/l or more and not more than 20% of samples should be below 50 μg/l.
Thyroid size
The size of the thyroid gland changes inversely in response to alterations in iodine intake, with a lag interval which varies from a few months to several years depending on factors such as the severity and duration of iodine deficiency, the effectiveness of iodine intervention and possibly goitrogenic factors.
For many years thyroid size has been determined by inspection and palpation. This method appears attractive because it enables observers to examine a large number of people in a short time without the use of expensive equipment. However, there is concern about the accuracy of diagnosis with this method. Ultrasonography provides a more accurate and objective method of determining thyroid size, but it requires expensive equipment and thorough training, and the measurement takes more time.
It is important to choose an appropriate target group for determination of thyroid size. Because of the small size of the thyroid gland of neonates and preschoolers, it is neither feasible nor practical to assess goiter in this group, not even by ultrasonography.
The preferred target group is school-aged children between 6 and 12 years, and if possible, 8–10-year-old children, to avoid the rather small thyroid glands of the young children and pubertal effects in the older ones. Schoolchildren are often used for goiter studies because of their accessibility and vulnerability to iodine deficiency (Figure 12.1). Pregnant women are a prime target group for IDD control activities because they are especially sensitive to marginal iodine deficiency and are relatively accessible given their participation in antenatal clinics.
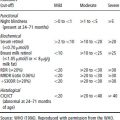
Thyroid size by palpation
Determination of thyroid size by palpation requires careful training and initial collaboration with an experienced observer. After visual inspection of the thyroid gland, the gland is palpated by gently sliding the finger along the side of the trachea (windpipe) between the cricoid cartilage and the top of the sternum. Both sides of the trachea should be palpated. The size and consistency of the gland are carefully noted. If necessary, palpation may be slightly enhanced by asking the subject to swallow to make the thyroid move up. A thyroid gland with lateral lobes each having a volume greater than the terminal phalanges of the thumbs of the subject being examined will be considered goitrous.
The size of the thyroid gland is categorized into one of the following grades:
- grade 0: no palpable or visible goiter
- grade 1: a mass in the neck that is consistent with an enlarged thyroid that is palpable but not visible when the neck is in the normal position, but moves upwards in the neck as the subject swallows; nodular alterations can occur even when the thyroid is not visibly enlarged
- grade 2: a swelling in the neck that is visible when the neck is in a normal position and is consistent with an enlarged thyroid when the neck is palpated.
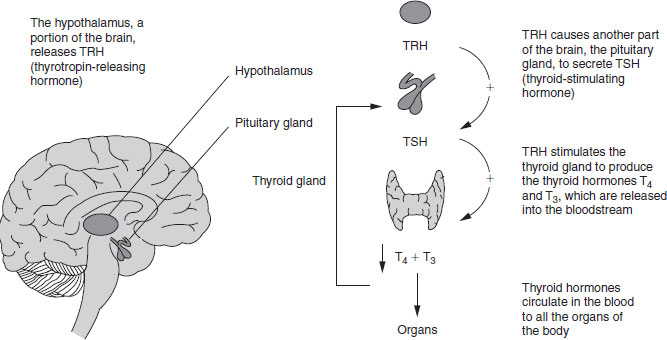
Figure 12.1 Role of the thyroid gland, pituitary gland and hypothalamus in the synthesis and release of thyroid hormones.
This classification system based on grades replaces one based on stages. In that system grade 1 was divided into stage Ia (detectable only by palpation) and stage Ib (visible when neck fully extended; can also include nodular glands even if not goitrous), while grade 2 was divided into stage II (visible with neck in normal position) and stage III (very large goiter recognizable at a considerable distance). The total goiter rate is calculated as the sum of grades 1 and 2. When this rate exceeds 5% in 6–12-year-old schoolchildren the population is said to have a public health problem, except in the short term after the introduction of an iodization program. Usually the iodine deficiency is corrected rapidly with an effective iodization program, but the goiter rates take longer to return to an acceptable level.
Thyroid size by ultrasonography
Ultrasonography is a safe, noninvasive, specialized technique, which provides a more accurate measurement of thyroid volume than palpation. The increased accuracy of ultrasonographic measurement is particularly useful in distinguishing between goiter grades 0 and 1, in situations where the prevalence of visible goiter is small, and in monitoring iodine control programs where thyroid volumes are expected to decrease over time.
Portable instruments are available on the market and should be used with a 7.5 MHz transducer by a trained and standardized operator. No universal normative values for the thyroid volume of iodine-replete children are available, except for thyroid volumes in European schoolchildren aged 6–15 years as a function of age, gender and body surface area. Normative values for populations under investigation should be established.
Thyroid-stimulating hormone and thyroglobulin
Thyroid-stimulating hormone (TSH) and thyroglobulin can be used as indicators to assess IDD, or as surveillance indicators, under certain circumstances. Blood spots on filter paper or serum samples can be used to measure TSH, using the highly sensitive analytical assay. TSH concentrations increase in iodine deficiency as part of the feedback system involving the thyroid-related hormones. However, the increase is not great unless the deficiency is moderate or severe. Therefore, the TSH concentration in school-aged children and adults is not a good indicator for iodine deficiency, and its use in school-based surveys is not recommended. Blood-spot TSH in neonates is a valuable indicator for iodine deficiency because the neonatal thyroid has limited iodine stores and even mild iodine deficiency may increase TSH secretion. Blood can be taken either from the cord at delivery or by heel prick after birth (usually after 72 h). Usually the primary purpose of screening for neonatal TSH is to detect congenital hypothyroidism, but it can also be used as an indicator of community iodine nutrition. For this reason the screening must be universal, and must not omit children born in remote or low socioeconomic areas.
When the thyroid is enlarged in iodine deficiency larger amounts of thyroglobulin are released, increasing the thyroglobulin levels in the circulation. The laboratory technique is similar to that for TSH and other immunoassays. It has been successfully applied to blood spots, but not yet developed commercially.
Other indicators of iodine deficiency
Cretinism provides an indication of the magnitude of the IDD problem only when it is severe. The condition is comparatively rare and difficult to diagnose (particularly the more subtle cases), cases are often hidden away, and since the life expectancy of cretins varies, incidence data may be more appropriate than prevalence data.
Determining serum concentrations of the thyroid hormones thyroxine (T4) and triiodothyronine (T3) as indicators of iodine deficiency is usually not usually recommended as these tests are cumbersome, more expensive and less sensitive than other indicators. In iodine deficiency the serum T4 concentration is typically lower, and the serum T3 concentration higher, than in normal populations, but the overlap reduces the usefulness of these hormones in assessing IDD.
12.3 Clinical features
A suboptimal dietary supply of iodine results in insufficient synthesis of thyroid hormone and in hypothyroidism, which is responsible for the wide range of abnormalities collectively known as IDD.
An enlarged thyroid, or goiter, is the most apparent manifestation of iodine deficiency, and serves as a biological marker for the potential existence of other IDD. A person is regarded as having goiter when the thyroid gland is enlarged to such an extent that the lateral lobe is bigger than the terminal phalanx of the thumb of the individual being examined. A goiter of this size is not visible but can be palpated.
When the thyroid gland is further enlarged, it becomes visible and it is estimated that in 1990 over 200 million individuals, mostly in developing countries, had visible goiter. The prevalence and severity of goiter increase with increasing severity of iodine deficiency, and become almost universal in populations where iodine intake is less than 10 μg/day. In general, goiter is not particularly serious. If the thyroid gland is large, it may be regarded as unattractive, with such consequences that is difficult to find a husband or wife. Fashions change: in the past in Europe, goiter was regarded as somewhat attractive, just as obesity was. Large goiters sometimes develop nodules, which can exert undue pressure on the trachea and esophagus, thus causing difficulty with breathing and swallowing.
12.4 Iodine metabolism
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree