Introduction to Hypothyroidism
Lewis E. Braverman
David S. Cooper
Hypothyroidism is the most common clinical disorder of thyroid function. It is most often caused by a disorder of the thyroid gland that leads to a decrease in thyroidal production and secretion of thyroxine (T4) and triiodothyronine (T3), in which case it is referred to as primary hypothyroidism. Primary hypothyroidism is invariably accompanied by increased thyrotropin (TSH) secretion. Much less often, hypothyroidism is caused by decreased thyroidal stimulation by TSH, which is referred to as central, secondary, or hypothyrotropic hypothyroidism. Central hypothyroidism may be caused by pituitary or hypothalamic disease, the latter causing deficiency of thyrotropin-releasing hormone (TRH). It is usually accompanied by low or inappropriately normal serum TSH concentrations, but a few patients have normal or even high serum TSH concentrations because they secrete TSH that is immunoreactive but biologically inactive. Although serum free T4, T3, and TSH concentrations may be low in patients with nonthyroidal illness, this constellation of laboratory abnormalities is accompanied by few if any clinical manifestations of hypothyroidism (see Chapter 11C). The rare patients with generalized resistance to thyroid hormone may have some residual signs of past hypothyroidism, but usually there are few, if any, symptoms or signs of hypothyroidism when the condition is recognized (see Chapter 58).
Severe hypothyroidism is sometimes referred to as myxedema, but the term “myxedema” also refers to nonpitting edema caused by the accumulation of glycosaminoglycans in subcutaneous and other interstitial tissue that occurs in hypothyroid patients. It is most often present in long-standing or severe primary hypothyroidism (and is rarely seen today). It should not be confused with “pretibial myxedema” (thyroid dermopathy), seen in some patients with hyperthyroidism due to Graves’ disease.
Table 34.1 Causes of Hypothyroidism | ||
|---|---|---|
|
Primary hypothyroidism may result from diseases or treatments that destroy thyroid tissue or interfere with thyroid hormone biosynthesis (Table 34.1). Worldwide, iodine deficiency is the most common cause of hypothyroidism. In areas where iodine intake is adequate, the most common causes are chronic autoimmune thyroiditis, which occurs in both goitrous and atrophic forms, and radiation-induced hypothyroidism. The latter is usually caused by radioactive iodine treatment of hyperthyroidism. External radiation therapy directed to the neck in patients with lymphoma or head and neck cancer can also lead to hypothyroidism. Although central hypothyroidism is rare, some of its causes (e.g., pituitary or hypothalamic tumors) may have disabling and even potentially fatal effects independent of the thyroid deficiency. For this reason, and because primary hypothyroidism may not be due to permanent thyroid destruction, an attempt should always be made to determine the cause of hypothyroidism in an individual patient.
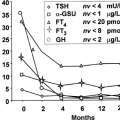
The clinical manifestations of hypothyroidism are largely independent of its cause. It affects persons of all ages and both sexes, although most of the patients are women, whatever the cause. Hypothyroidism may be overt or subclinical. Overt hypothyroidism is defined as high serum TSH concentrations and low serum free T4 concentrations, subclinical hypothyroidism is defined as high serum TSH (usually <10 mU/L) and normal serum free T4 concentrations. Many, but not all patients with overt hypothyroidism have symptoms and signs of hypothyroidism, but the spectrum is broad; at one extreme are those patients who have no or very few symptoms and signs of hypothyroidism, and at the other extreme are those with myxedema coma (see Chapter 44) (1). Patients with subclinical hypothyroidism typically have few or no symptoms or signs of hypothyroidism (see Chapter 47). Recently, it has been found that some healthy older individuals may have serum TSH levels that exceed the upper limit of normal for the younger population, making the diagnosis of subclinical hypothyroidism problematic in the elderly (2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree