Figure 5.1 Anatomy of the thyroid gland and oropharynx, demonstrating the relationship to a pyriform fistula, anterior view.
Episodes of AST are often preceded by an upper respiratory infection or another factor (e.g., injury or obstruction of the fistula by food or foreign bodies) that may induce inflammation of a pyriform fistula and thus facilitate transmission of pathogens to the thyroid. Particularly in children, the left lobe is more commonly involved, reflecting the observation that pyriform sinus fistulas predominantly occur on the left.
Infected embryonic cysts of the third and fourth branchial pouches have also been identified as causes of AST. Infectious organisms may also spread directly to the thyroid via a patent thyroglossal duct fistula (Figure 5.2). AST may be caused by spread of microbes from adjacent sites of infection, such as the oropharynx and middle ear, although this occurs infrequently, presumably because the thyroid is encapsulated within its fibrous sheath. Perforation of the esophagus may also result in direct spread of infection to the thyroid gland.
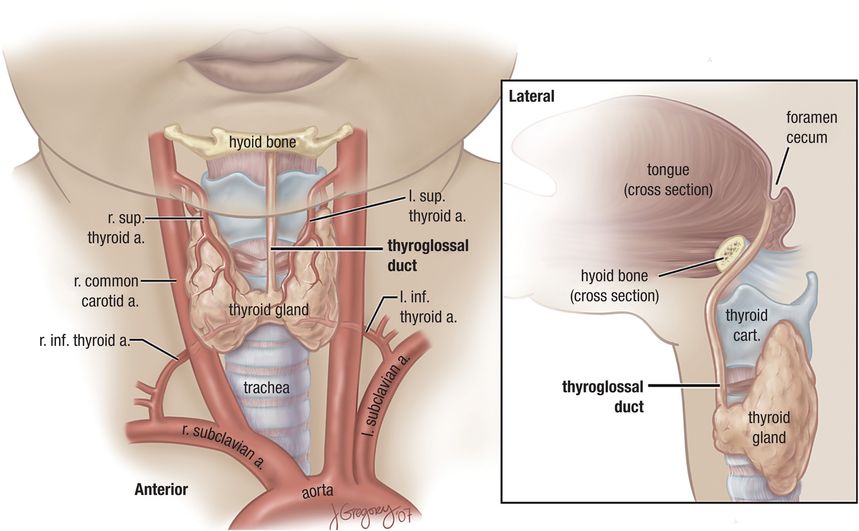
Figure 5.2 Anatomy of the thyroid gland and neck. A thyroglossal duct fistula is shown in frontal and lateral views.
Bacterial AST may also result from trauma to the anterior neck. One of us (SGB) has seen a single case of direct spread of infection to the thyroid from a neck wound. The patient was a mechanic who scraped his anterior neck while working on his back underneath an automobile. The wound appeared superficial, but infection spread to the thyroid with abscess formation. The offending organism was a staphylococcus. Even fine-needle aspiration (FNA) of thyroid nodules has resulted in thyroid infection.
Immunosuppressed patients, such as those with human immunodeficiency virus (HIV) infection or acquired immunodeficiency syndrome (AIDS) or hematologic malignancies, as well as patients with autoimmune diseases or organ transplants treated with immunosuppressive agents, are at risk for suppurative thyroiditis, which can occur as part of a disseminated infectious process. These infections arise when pathogens reach the thyroid hematogenously or through the lymphatic system.
Microbiology
Gram-positive organisms are the most common etiologic pathogens in AST, although a wide variety of bacteria have been isolated as causative agents in case reports (Table 5.1). In a review of 224 cases of thyroid infections reported between 1900 and 1980, staphylococci, found in 23 of 66 (35%) of culture-positive specimens, were the most frequently identified organisms; Staphylococcus aureus was the predominant species. Streptococcus pyogenes, presumably acquired after a recent pharyngeal infection or colonization, Streptococcus pneumoniae, and other streptococci were also commonly recovered. In a subsequent review of an additional 191 cases of AST reported between 1980 and 1997, in which 130 microorganisms were isolated, Yu et al. found that the most common bacterial isolates were gram-positive aerobes (39%), gram-negative aerobes (25%), and anaerobes (12%, mostly in mixed culture).
| Nonimmunocompromised host |
|---|
| Staphylococcus aureus |
| Staphylococcus epidermidis |
| Streptococcus pyogenes |
| Other streptococcal species |
| Klebsiella species, especially in diabetic patients |
| Other Enterobacteriaceae |
| Anaerobic oral flora (foul smell on needle aspiration may give hint of this) |
| Other gram-negative bacteria free-living in water secondary to upper respiratory tract infection |
| Mycobacterium tuberculosis |
| Mycobacterium bovis |
| Actinomyces species |
| Immunocompromised host |
|---|
| Mycobacterium avium-intracellulare |
| Nocardia species |
| Pneumocystis jirovecii |
The true involvement of anaerobic bacteria in AST is unknown because past studies have not used uniform methods for the recovery of anaerobes. Because anaerobes are more difficult to isolate, it is possible that culture-negative cases of AST may represent purely anaerobic or mixed infections, an important consideration when choosing empiric therapy for AST.
The bacterial pathogens implicated in AST in children are similar to those found in adults. S. aureus, S. pyogenes, Staphylococcus epidermidis, and Streptococcus pneumoniae are the most commonly isolated organisms in pediatric cases of AST.
Following bacteria, fungi are the second most common microorganisms to infect the thyroid, representing 15% of cases of AST in the review by Yu and colleagues. Fungal thyroiditis most commonly occurs in immunocompromised patients, such as those with leukemia, lymphoma, and autoimmune diseases and in organ transplant patients on immunosuppressive therapy. In a review of 41 fungal thyroiditis cases published between 1970 and 2005, Goldani et al. found that Aspergillus species (spp.) were the most commonly reported cause of fungal thyroid infection. Thyroid involvement by Aspergillus spp. was found at autopsy as part of disseminated aspergillosis in 13 (62%) of 21 patients, most of whom lacked clinical manifestations and laboratory evidence of thyroid dysfunction. After Aspergillus spp., Candida spp. were the second most common cause; other fungal etiologies reported include Cryptococcus neoformans, Coccidioides immitis, Histoplasma capsulatum, and Pseudallescheria boydii.
Pneumocystis jirovecii (then called Pneumocystis carinii), now classified as a fungus, was not included in the review by Goldani et al.; however, P. jirovecii has been found to be a cause of thyroid infections, almost exclusively in patients with AIDS. Yu et al. identified P. jirovecii as the causative agent in 16 of 19 cases of fungal thyroiditis in their literature review.
Mycobacterium tuberculosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




