| Bedside index for severity in acute pancreatitis: within the first 24 hours of presentation: |
| Blood urea nitrogen >25 mg/dL |
| Impaired mental status |
| Presence of SIRS |
| Age >60 years |
| Pleural effusion on imaging |
| A BISAP score ≥ 3 is associated with increased risk of complications |
Computed tomography
Rapid bolus computed tomography (CT) scanning using intravenous contrast effectively and accurately (>95%) detects pancreatic necrosis. It should only be used if the diagnosis of AP is in doubt, and should not be performed until after appropriate volume resuscitation, in order to minimize renal complications. In addition, its use should be restricted to patients who have severe AP, who do not show signs of clinical improvement despite supportive care over several days, or in whom infection is suspected, by either fever or positive blood cultures. The severity of AP can be estimated by the findings on CT scan, such as the presence of necrosis (nonviable tissue) with non-perfused areas of pancreatic parenchyma, pancreatic enlargement, peripancreatic inflammatory changes, and adjacent or parenchymal fluid collections.
Natural history of acute pancreatitis
Since the mid 1990s, it has become evident that there are two phases in the natural course of severe or necrotizing AP. It includes an early vasoactive and toxic phase and a late phase dominated by septic complications. The first 14 days after onset of the disease are characterized by SIRS, resulting in organ system failure. Inflammatory mediators released into the systemic circulation are associated with the development of cardiorespiratory and renal failure, fever, and tachycardia. Organ system failure may resolve or become increasingly severe. In the late phase, infection of pancreatic necrosis develops usually after the first week, peaks in the second and third week after onset of the disease, and is reported in 20% to 30% of patients with necrotizing pancreatitis. Infected necrosis is the single most important risk factor in death from necrotizing pancreatitis, with sepsis-related multiple organ failure as the main life-threatening complication with a mortality rate of up to 70%.
Classification of fluid collections and infections
There are two distinctive forms of infection in AP: that which follows interstitial edematous pancreatitis (IEP) and necrotizing pancreatitis (Table 47.2). In addition, infection is categorized by its timing, either <4 weeks or ≥4 weeks after onset of AP. CT of IEP demonstrates edema manifested by localized, diffuse enlargement with homogenous or minimally heterogeneous enhancement of pancreatic parenchyma. Conversely, there are three forms of necrosis: (1) limited to the pancreas alone; (2) peripancreatic tissue alone; and (3) the combination of the above, which is the most common CT finding. Pancreatic necrosis is graded on CT as being <30% or ≥30%.
| Type of pancreatitis | Fluid collections |
|---|---|
| < 4 weeks after onset | |
| Interstitial edematous pancreatitis | APFC (acute peripancreatic fluid collection): sterile or infected |
| Necrotizing pancreatitis | ANC (acute necrotizing collection) |
| Parenchymal necrosis alone: sterile or infected | |
| Peripancreatic necrosis alone: sterile or infected | |
| Pancreatic and peripancreatic necrosis: sterile or infected | |
| ≥ 4 weeks after onset | |
| Interstitial edematous pancreatitis | Pancreatic pseudocyst: sterile or infected |
| Necrotizing pancreatitis | WON (walled-off necrosis): sterile or infected |
Acute pancreatic fluid collections occur frequently (30% to 50%), and early in the course of interstitial edematous pancreatitis, and most (>50%) reabsorb spontaneously. If they persist > 4 weeks and are encapsulated, they are referred to as pseudocysts, which do not contain non-liquefied necrotic material. Either fluid collection may become infected.
Conversely, in patients with necrotizing pancreatitis, the fluid collection contains non-liquefied necrotic material. The initial collection is variably loculated and nonencapsulated. Over time, liquefaction develops as the necrotic tissue breaks down. Collections that contain non-liquefied necrotic elements are more likely to become infected. On CT, air bubbles within the collection suggest infection, but can also occur as a result of fistulization into the bowel. Subsequently, it may become encapsulated and is then referred to as walled-off necrosis. Similar to above, either fluid collection may become infected.
Pathogenesis
The pathophysiology of infection of peripancreatic necrosis is essentially unknown. Upper gastrointestinal dysmotility has been observed in AP as well as in cholestasis and sepsis. There are several hypothetical mechanisms by which bacteria can enter pancreatic and peripancreatic necrosis leading to the infection and include (1) the hematogenous route via the circulation, (2) transmural migration through the colonic bowel wall to the pancreas (translocation), (3) via ascites to the pancreas, (4) via the lymphatics to the circulation, (5) via the biliary duct system, and/or (6) from the duodenum via the main pancreatic duct. Most pathogens in pancreatic infection are the gastrointestinal gram-negative bacteria, with the bowel seeming to be the main source of pancreatitis-related infections. It is, therefore, possible that bacterial translocation is the most important mechanism for contamination of pancreatic necrosis (Figure 47.1).
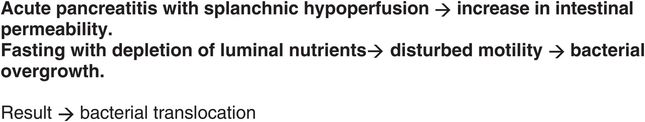
Figure 47.1 Factors possibly leading to bacterial translocation. Adapted from Bakker OJ, van Santvoort HC, Besselink MGH, et al. Curr Gastroenterol Rep. 2009;11:104–110.
Several studies have examined the frequency of bacterial infection of necrotic areas in the natural course of severe AP, without antibiotic intervention. One series showed an overall contamination rate of 24% within the first week of the onset of AP in patients undergoing surgery for severe AP, increasing to 46% and 71%, respectively, in the second and third weeks. Thus, patients with severe AP have the highest risk of pancreatic infection in the third week after onset of the disease. The overall infection rate in this series was 39%.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





