INTRODUCTION
Louis Pasteur established the germ theory of infectious diseases whilst working near Alès, between 1865 and 1870, following his discovery that the two most prevalent diseases of silkworm were caused by different microbes.
1 This groundbreaking discovery apparently settled a long discussion between two conflicting theories. The first, in which diseases were considered to be intrinsic, had long held sway over the second, in which diseases were considered to be extrinsic. It rapidly became clear, with the successive identification of numerous microbes, culminating in Koch’s discovery of
Mycobacterium tuberculosis in 1882,
2 that this new paradigm accounted for the heavy burden of childhood fever and death that had prevailed throughout human history. About half the children born died of fever before the age of 15, and this death toll could be attributed to microbes.
3 This theory did not explain why rare children survived infectious diseases and assumed that healthy children had remained free from infection. However, the edifice on which this theory was constructed collapsed between 1905 and 1915, with the gradual realization that most infected individuals remained asymptomatic, often throughout their lifetime. Asymptomatic individuals were found to harbor latent microbes—nonreplicating microbes in a dormant state— such as
M. tuberculosis.
4 Even more strikingly, actively replicating microbes were found to cause silent infections in other individuals, such infections being termed “unapparent infections” by Charles Nicolle.
5 The question of interindividual variability in the course of infection therefore became, and has since remained, a key question in the fields of infectious disease and immunology, and is, arguably, one of the most important questions in biology and medicine. The problem in itself suggests that there are, after all, some intrinsic determinants of disease. The first explanation put forward followed on naturally from another ground-breaking discovery by Pasteur in 1880 to 1881: the prevention of infectious diseases and the foundations of immunology, with the use of attenuated microbes to vaccinate against fowl cholera and sheep anthrax.
6 This led to the hypothesis that related, less virulent microbes or smaller amounts of the same microbes had previously immunized the individuals who remained healthy in the course of infection with a microbe virulent enough to kill other individuals. This powerful idea can be seen as an immunologic or somatic theory of infectious diseases. We now know that this acquired immunity (often referred to as adaptive immunity) emerged twice in the evolution of vertebrates, by convergent evolution, that it is lymphoid, and that it involves both genetic and epigenetic components. However, although this theory was considered plausible in adults, and perhaps in teenagers, especially during secondary infections or reactivation from latency, it was less convincing for primary infections in early childhood, which comprised the majority of cases. In this context, a few human geneticists looking at the problem from the complementary standpoints of clinical and population genetics, including Archibald Garrod and Karl Pearson in particular, collected evidence between 1910 and 1930 for strong, germline, genetic determinism, controlling innate immunity against microbes.
7,8 As stated by Garrod, “It is, of necessity, no easy matter to distinguish between immunity which is inborn and that which has been acquired.”
7The development of new vaccines and the discovery of sulfonamides and antibiotics during the 1930s rendered these questions obsolete; it became less pressing to understand a problem that everyone thought would soon be resolved. Paradoxically, antibiotics themselves triggered renewed interest in the question in the early 1950s, when a small group of pediatricians in Europe and America noted that rare children suffered from multiple, recurrent infectious diseases, each of which was treated with antibiotics, lacked a major leukocyte subset or gammaglobulins, and shared this phenotype with relatives, consistent with an inheritable trait.
9,10,11,12,13,14 This was the birth of the field of primary immunodeficiency (PID), a term apparently first coined in 1971
15,16 that remains more frequently used than inborn errors of immunity, which was first used in 1966.
16,17 These children had major immunologic abnormalities, such as neutropenia,
11,14 alymphocytosis,
12,13 or agammaglobulinemia.
9,10 Moreover, their infectious and immunologic phenotypes often followed a Mendelian pattern of segregation within their families. It is, however, important to bear in mind that the definition of PID established in the 1950s was based on an artificial, as opposed to natural phenotype, because these children with multiple life-threatening infections would have died during their first episode of infection before the advent of antibiotics. Moreover, although the infectious phenotype of these patients led to their investigation and the pattern of inheritance was suggestive of a Mendelian trait, PIDs were classified and defined solely on the basis of the immunologic phenotype. There had been previous descriptions of inherited disorders associated with infectious diseases, such ataxia-telangiectasia in 1926 and 1941,
18,19 Wiskott-Aldrich syndrome in 1937,
20,21 and epidermodysplasia verruciformis in 1933
22 (and its viral etiology in 1946
23), but
these disorders were not recognized as PIDs until 1964,
24,25 1959,
26,27 and 2002,
28 respectively. They were long considered from other angles, in the absence of detectable immunologic abnormalities. Autoimmune polyendocrinopathy syndrome with mucocutaneous candidiasis was probably first described clinically between the 1920s and 1940s, but the autoantibodies involved were not described until the 1970s.
29,30 More surprisingly, Chediak-Higashi syndrome (CHS) was first described as an inherited predisposition to infections with detectable leukocyte abnormalities in 1943 to 1954,
31,32,33 but was not recognized as a PID until 1962.
34Severe congenital neutropenia (SCN) and CHS were among the first PIDs to be described, but these and other inborn errors of myeloid cells, such as chronic granulomatous disease (CGD), which was first described in 1966, and complement defects, first described in 1963 (hereditary angioneurotic edema due to an absence of C1 esterase inhibitor),
35 were not included in the first classifications of PIDs, which were restricted to the lymphoid arm of immunity, in 1968,
36 1970,
37,38 1971,
15 1972,
39 1973,
40 and 1974.
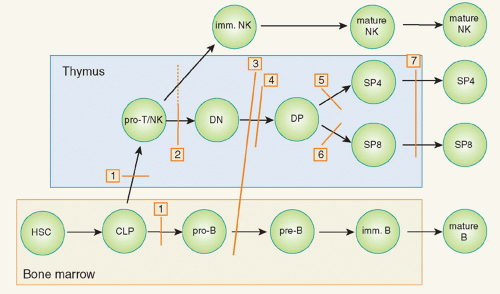
41 Over this period, the fields of immunology and PIDs evolved in parallel, focusing on acquired or adaptive immunity, which is sometimes referred to as adaptive or lymphoid immunity. The lymphoid imprint was so strong that the first report on PIDs even distinguished explicitly between these disorders and myeloid abnormalities. Unsurprisingly, given that these PIDs affected the development or function of B- and/or T-cell immunity, these patients displayed multiple, recurrent infectious diseases that were often opportunistic (ie, not seen in patients with apparently intact immunity). Patients with T- and B-cell PIDs also displayed noninfectious, autoimmune, allergic, and in some cases, cancer phenotypes. Despite the broad infectious phenotypes of the patients with complement and phagocyte disorders identified, the first mention of quantitative and qualitative disorders of phagocytes did not occur until 1974, when it appeared, somewhat amusingly, in a preliminary report,
42 but not in the official report
43 of the second World Health Organization (WHO) international workshop on PIDs. The weaknesses of this definition and classification of PIDs were apparent to some investigators, including Gatti, who ironically compared this system to the ancient Chinese classification for animals.
44 The classification nonetheless evolved, as complement disorders were mentioned in 1976 but phagocyte defects were not,
45 and qualitative phagocyte disorders (including CGD and CHS) appeared in the third (1978),
46 fourth (1983),
47 fifth (1986),
48 sixth (1989),
49 and seventh (1992)
50 WHO classifications, although SCN did not. The full range of PIDs was not covered until the eighth WHO classification in 1999,
51 and has since been dealt with in the 10th (2003),
52 11th (2004),
53 12th (2006),
54 13th (2007),
55 14th (2009),
56 and the most recent (15th
57) WHO International Union of Immunological Societies reports. Meanwhile, two prominent reviews published in 1984 and 1995 made no reference to phagocyte defects.
58,59,60 Some aspects of the history of the field have been covered in at least two reviews.
61,62The common PID classification and the underlying definition of PIDs proved increasingly inadequate and unable to describe the situation in reality, which extended well beyond phagocytic disorders, from the 1990s onwards. The definition and classification of PIDs have always been engaged in an eternal game of catch-up with the reality of the situation on the ground, and this gap between the conservative words used to describe these conditions and the continual discovery of new PIDs, ever increasing the known spectrum of these diseases, has been maintained.
63,64 Phenotypic studies in this field have progressed in at least two ways. First, multiple and diverse new phenotypes have progressively been attributed to PIDs, including, of course, autoimmunity,
30 malignancy,
65 and allergy,
66 but also various other phenotypes, such as autoinflammation,
67 angioedema,
68 hemophagocytosis,
69 and thrombotic microangiopathies.
70 The underlying mutations involve multiple circuits affecting both myeloid and lymphoid cells. Second, patients with a single infectious disease, and often with a single infectious episode, have been shown to display PIDs.
71 Again, the underlying mutations affect both lymphoid and myeloid cells, but they may also, in some cases, concern nonhematopoietic cells. PIDs were initially associated with multiple, recurrent, and often opportunistic infections with an early onset and fatal outcome. They were familial, recessive traits. Exceptions to these rules gradually emerged, beginning with the description of patients with autosomal recessive (AR) defects in the terminal components of complement (C5 to C9), who are specifically susceptible to
Neisseria,
72 patients with X-linked recessive (XR) lymphoproliferative syndrome, who are susceptible to Epstein-Barr virus (EBV),
73 and patients with AR epidermodysplasia verruciformis, resulting in a selective predisposition to infection with skin-tropic, oncogenic papillomaviruses.
74 These studies paved the way for the discovery of new PIDs underlying particular infectious diseases in children who were otherwise healthy and normally resistant to other infectious diseases. Children with mycobacterial diseases were found to carry inborn errors of interferon (IFN)γ immunity.
75 Mutations in the toll-like receptor (TLR) and interleukin (IL)-1R pathway are associated with pyogenic bacterial diseases, whereas mutations in the TLR3 pathway are associated with herpes simplex encephalitis.
76 Finally, inborn errors of IL-17 immunity underlie chronic mucocutaneous candidiasis.
77,78 These discoveries indicated that otherwise healthy children with a single infectious disease can display inborn errors of immunity to primary (in cases of acute disease) or recurrent/latent (for chronic disease) infection.
71,79The definition of PIDs is evolving, thanks largely to the clinical delineation and genetic dissection of new phenotypes. These advances are also leading to changes in the classification of PIDs. PIDs were initially classified into two groups (defects of humoral and cell-mediated immunity), then into four major groups (T, B, complement, and phagocyte disorders). The 2011 WHO classification includes up to 10 (somewhat overlapping) categories of PIDs, despite the contentious omission of certain types of PID.
79a However, there is no consensus about the definition and classification of PIDs.
16 The classification of PIDs principally on the basis of immunologic phenotypes entails a risk of clinical and genetic overlap and of some disorders being ignored. A classification based on clinical phenotype would be more useful at the patient’s bedside, and a classification based
on genotype would be more useful at the research bench. However, the apparent lack of a solution to this problem is not a major concern. Hopefully, the classification will improve with the characterization of more PIDs, the deciphering of their genotypes, the dissection of their molecular, cellular, and immunologic phenotypes. and the description of their clinical phenotypes. Like a jigsaw puzzle, every piece should start to fit into place as we approach the solution. This task may not be as vast as it might initially appear, as there are no more than 25,000 genes for 7 billion individuals reproducing every two or three decades. However, we may never reach the asymptote, as there is no such thing as a distinct disease entity, precisely because of the tremendous germline and somatic genetic variability that makes each disease in each patient unique: there are only patients. There is therefore unlikely to be any satisfactory definition and classification of inborn errors of immunity in the near future. This does not matter so long as rapid progress is made in this field, in terms of awareness, diagnosis, treatment, and above all, in explorations of the genotype and intermediate phenotypes of known and new clinical phenotypes.
Why is it so important for the field of PIDs to thrive? This progress is above all important for the patients. As in other areas of medicine, strategies improving our understanding of pathogenesis constitute the only rational approach to improving the clinical management of patients, in terms of the quality of diagnosis, prognosis, and treatment. The availability of blood samples has made it possible to carry out very careful analyses of the relationships between genotypes, cellular phenotypes, immunologic phenotypes, and clinical phenotypes, as for inborn errors of erythrocytes and platelets, perhaps more thoroughly than in other fields of human genetics and pediatrics. For example, the discovery of new PIDs over the last two decades has made it clear that the 10 conventional warning signs used in PID awareness campaigns are completely out of date and require revision.
80 Another clinical lesson learned in the last 50 years is that most PID-causing genes are associated with high levels of clinical heterogeneity. Remarkable examples include mutations in the
NEMO gene, the effects of which range from death in utero to mild immunodeficiency in adults, reflecting the severity of the biochemical deficit caused by the morbid alleles,
81 and mutations in
RAG genes, the impact of which ranges from life-threatening severe combined immunodeficiency in infancy to combined immunodeficiency in adults.
57 Several genes have even been found to harbor loss-of-function (LOF) and gain-of-function (GOF) mutations. These genes include
WASP, LOF mutations, which underlie Wiskott-Aldrich syndrome (WAS), and GOF mutations, which underlie SCN,
82 and
STAT1, LOF mutations, which underlie mycobacterial or viral diseases, and GOF mutations, which underlie chronic mucocutaneous candidiasis (CMC).
78 Similarly, most, if not all of the known clinical phenotypes are associated with high levels of locus and allelic genetic heterogeneity. For example, several agammaglobulinemia-causing autosomal genes were identified following the discovery of
BTK mutations in boys with XR agammaglobulinemia.
83 A large proportion of the patients with each PID, particularly for the most recently described conditions, do not carry mutations in known morbid genes. It is therefore highly likely that new genetic etiologies will be discovered in the future. The clinical implications of research in this field actually extend well beyond diagnosis and pathogenesis, as the first cases of successful immunoglobulin (Ig) substitution,
9 bone marrow transplantation,
84 transfusion-based enzymatic replacement,
85 and gene therapy
86 all concerned children with PIDs. These children were also among the first to benefit from PEGylated enzymatic replacement
87 and treatment with recombinant cytokines.
88Perhaps of greater relevance to this book, this field has had extraordinary immunologic implications. One of the pioneers in this field, Robert Good, often referred to PIDs as “experiments of nature,” reviving a line of investigation that began with Harvey and was followed by Osler, Garrod, McQuarrie, and Burnet, among others.
89,90 Indeed, physicians and scientists can learn much by deciphering the enigmas posed by the experiment of nature represented by each patient with a PID. No matter how rare a disorder, it can provide considerable insight into the fundamental laws operating in living organisms. More conventional experiments, designed by humans and carried out in animal models, benefit from being carefully thought out and executed in a controlled manner. However, they suffer from the limitations inherent to their experimental nature. Experimental protocols differ from natural processes in many ways (inbred animals, conditions of infection, microbes). Human genetics provides us with a unique opportunity to define the function of host genes in natural, as opposed to experimental, conditions: in a natural ecosystem governed by natural selection.
91,92 Immunity
in natura can be defined by the careful dissection of PIDs and by other related approaches, such as epidemiologic and evolutionary genetics. The differences between mice and humans are often discussed, and rightly so, as these two species differ in many ways, despite the similar architecture of their immune systems. Beyond these multiple, and in some cases large, differences between humans and mice, there may be major differences between the processes used to study phenotypes, infectious and otherwise, in the two models. For example, experimental infections in mice generally involve inoculation with microbes that have not coevolved with these rodents, via artificial routes of infection and at high doses. By contrast, most human infections are natural, although some experimental infections, such as those caused by live vaccines, have played an important role in the development of this field. The experimental triggers of autoimmunity in mice are also different from those operating in natural conditions in humans. The genetic dissection of PIDs thus provides us with a unique opportunity to cast new light on the function of human genes in a natural ecosystem. Over the years, these observations have provided invaluable insights sometimes at odds with the mouse model.
It will not be possible to cover the entire field in this chapter. More than 200 inborn errors of immunity have been characterized genetically.
57,93 Many other PIDs have been described clinically but have no known genetic etiology. Doctors in this field also know that a large fraction of the patients under their care suffer from exceedingly rare
disorders, sometimes apparently limited to a single family, not reported in the medical literature. Moreover, many phenotypes might be due to new PIDs. These phenotypes form a large reservoir for the future dissection of new inborn errors of immunity, as previously illustrated by autoinflammation, hemophagocytosis, angioedema, thrombotic microangiopathies, and isolated infectious diseases.
64 Finally, we know that most known PIDs are associated with tremendous locus and allelic heterogeneity. With about 25,000 known genes and only 8000 known inborn errors, including about 300 PIDs, we can predict that 10,000 inborn errors of immunity, defined by a specific causal relationship between a genotype and a phenotype, currently await discovery. An estimate of 1000 to 2000 PID-causing loci is not unrealistic. Even with the only 300 or so known PIDs, it is clear that we cannot cover even a substantial fraction of these diseases here. We will therefore focus our review on seven topics, focusing in more detail on a specific syndrome or disease for each and discussing its genetic basis. We will pay particular attention to the immunologic lessons that can be drawn from these experiments of nature.