HYPOTHYROIDISM IN THE NEONATE AND CHILD
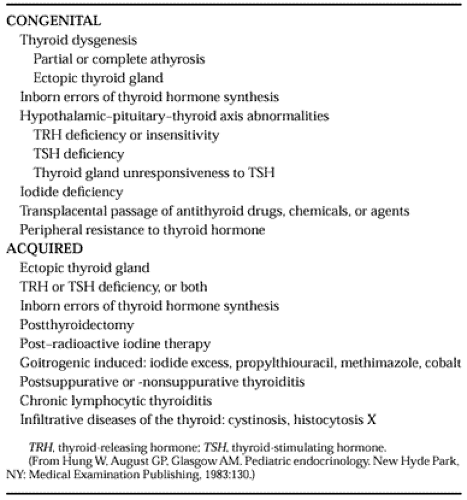
ETIOLOGY
The causes of pediatric hypothyroidism are listed in Table 47-3. Because most of the congenital and acquired causes are similar, they are discussed together. The terms cretinism and congenital hypothyroidism are used for hypothyroidism present before or at birth.
Endemic iodine deficiency may cause congenital hypothyroidism (cretinism) (Fig. 47-1). Thyroid dysgenesis is the most common cause of congenital hypothyroidism in nonendemic areas. The term includes aplasia, ectopy, and hypoplasia of the thyroid gland. It is twice as frequent among women as men. Interestingly, circulating antithyroid antibodies are found in a higher percentage of sera from mothers of nongoitrous cretins than in control mothers. Although these antibodies can cross the placenta, they probably do not destroy the fetal thyroid gland. Thus, the possible role, if any, of circulating or cellular antithyroid antibodies in the causation of congenital athyrosis is not clear. In mothers with Graves disease with or without thyrotoxicosis, TSH receptor-blocking antibodies may cross the placenta and cause transient neonatal hypothyroidism (see Chap. 42).5
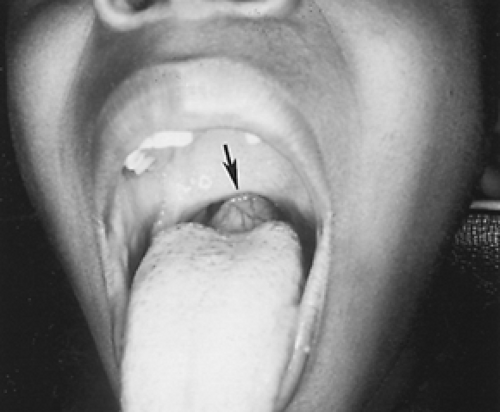
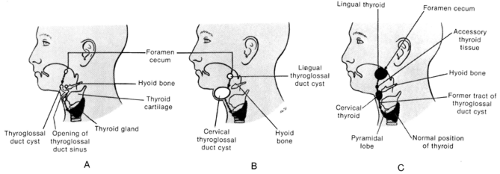
Ectopy of the thyroid gland is an important cause of hypothyroidism. Approximately 75% of patients with lingual thyroid glands do not have any normally located thyroid tissue
(Fig. 47-2 and Fig. 47-3). Usually, the amount of ectopic thyroid tissue is insufficient to prevent hypothyroidism, although it can respond to TSH stimulation. Ectopic thyroid glands must be included in the differential diagnosis of midline lingual and sublingual masses. All children with ectopic thyroid glands should have a trial of full replacement thyroid hormone therapy before surgical excision is contemplated. Thyroid hormone therapy prevents further hypertrophy and hyperplasia. There is no evidence that lingual or sublingual thyroid glands are malignant in the pediatric patient. In infants, the combination of elevated serum TSH and normal or low-normal T4 levels suggests the presence of thyroid ectopy.6 Infants with aplasia or hypoplasia of the thyroid gland also have high serum TSH and low T4 levels.
(Fig. 47-2 and Fig. 47-3). Usually, the amount of ectopic thyroid tissue is insufficient to prevent hypothyroidism, although it can respond to TSH stimulation. Ectopic thyroid glands must be included in the differential diagnosis of midline lingual and sublingual masses. All children with ectopic thyroid glands should have a trial of full replacement thyroid hormone therapy before surgical excision is contemplated. Thyroid hormone therapy prevents further hypertrophy and hyperplasia. There is no evidence that lingual or sublingual thyroid glands are malignant in the pediatric patient. In infants, the combination of elevated serum TSH and normal or low-normal T4 levels suggests the presence of thyroid ectopy.6 Infants with aplasia or hypoplasia of the thyroid gland also have high serum TSH and low T4 levels.
Hypothyroidism may occur because of a hereditary enzymatic deficiency that prevents synthesis of T4 and T3. Hereditary enzymatic defects of thyroid hormone synthesis are the second most common cause of congenital hypothyroidism
(Table 47-4).7 Patients with enzymatic defects may present with hypothyroidism with or without goiter or euthyroidism with goiter. Because the thyroid gland is not always palpable in infants, infants with congenital hypothyroidism caused by an enzymatic defect cannot always be differentiated by physical examination from those with athyrotic hypothyroidism. The diagnosis depends on specific tests of the various steps in thyroid hormone synthesis and release. Pendred syndrome is an autosomal recessive disorder characterized by a goiter resulting from a peroxidase defect, with euthyroidism or mild hypothyroidism and congenital sensorineural hearing loss. The Pendred syndrome gene is mapped to chromosome 7q31 and has been found to encode a putative sulfate transporter.8,9 Mutations have been found in the Pendred syndrome gene.8,9 Congenital hypothyroidism caused by mutations in the thyrotropin-receptor gene has been reported.10 The inherited disorders of thyroid hormone transport, T4-binding globulin deficiency must also be considered in the differential
diagnosis of hypothyroidism (Table 47-5). However, in this condition, the patient is clinically euthyroid.
(Table 47-4).7 Patients with enzymatic defects may present with hypothyroidism with or without goiter or euthyroidism with goiter. Because the thyroid gland is not always palpable in infants, infants with congenital hypothyroidism caused by an enzymatic defect cannot always be differentiated by physical examination from those with athyrotic hypothyroidism. The diagnosis depends on specific tests of the various steps in thyroid hormone synthesis and release. Pendred syndrome is an autosomal recessive disorder characterized by a goiter resulting from a peroxidase defect, with euthyroidism or mild hypothyroidism and congenital sensorineural hearing loss. The Pendred syndrome gene is mapped to chromosome 7q31 and has been found to encode a putative sulfate transporter.8,9 Mutations have been found in the Pendred syndrome gene.8,9 Congenital hypothyroidism caused by mutations in the thyrotropin-receptor gene has been reported.10 The inherited disorders of thyroid hormone transport, T4-binding globulin deficiency must also be considered in the differential
diagnosis of hypothyroidism (Table 47-5). However, in this condition, the patient is clinically euthyroid.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree