Cardiovascular
Congestive heart failure
Prolonged QT interval at ECG
Cardiomyopathy
Neuromuscular inability
Chvostek’s and Trusseau’s sign
Paresthesia
Muscle cramps and paresthesia
Laryngeal and bronchial spasms
Tetany
Seizures
Tremor
Neurological signs
Psychoneurosis
Personality disturbance
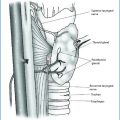
16.4 Hungry Bone Syndrome After Parathyroidectomy
The term “hungry bone syndrome” (HBS) defines a prolonged (more than 4 days postoperatively) and profound (serum calcium <8 mg/dL or 2.1 mmol/L) hypocalcemia after parathyroidectomy for severe hyperparathyroidism. HBS is usually associated with skeletal manifestations due to the high preoperative indices of bone turnover, osteitis fibrosa cystica and brown tumors [13].
The prevalence of HBS is highly variable among studies and has been reported to be 13–87% [13, 18, 19] but may rise dramatically in more severe forms of hyperparathyroidism, such as in patients with ESRD or kidney transplant recipients, in whom HBS may complicate up to 95% of parathyroidectomies [1, 13, 18, 20–23].
Bone surface is the site of a continuous process of remodelling, in which the damaged bone is removed by osteoclastic bone resorption process, and replaced with a new one through the process of osteoblastic bone formation. During this process, a disparity may be created between the total amount of bone that has been reabsorbed by osteoclasts and the bone not yet reformed by the osteoblasts, during the delay between the resorption and formation. This delay is considerably increased in primary hyperparathyroidism, leading to mineral depletion of bone and hypercalcemia [13, 24, 25]. Successful parathyroidectomy leads to a reduction in the activation of new remodeling sites and activates an increased skeletal usage of calcium, with immediate arrest of bone resorption in the face of continuing bone formation, leading to a profound and sometimes prolonged reduction of serum calcium, phosphate and magnesium.
Severe hypocalcemia in HBS may present with mild symptoms, including weakness, perioral parasthesia, and Chvostek sign, to life-threatening conditions with cardiac arrhythmias and generalized convulsions, which can lead to pathological fractures [1–3, 13] and finally, if left untreated, to coma and even death (Table 16.1).
As reported above, data on the risk factors for the development of HBS are still conflicting. With regard to age, older age at the time of surgery seems to be a risk factor for HBS [16, 26] due to the vitamin D deficiency and lower dietary calcium intakes, but other studies stated that younger age at the time of surgery may be a risk factor for HBS, especially in ESRD patients [1, 18, 21]. In patients who developed HBS, the removed glands had a larger volume and weight, and these patients had higher preoperative levels of serum calcium, PTH and alkaline phosphate compared with patients who had an uncomplicated course after parathyroidectomy [13, 16], although data are conflicting [18, 27]. Of interest, radiological evidence of hyperparathyroidism-induced bone disease, such as brown tumors, multiple fractures and osteitis fibrosa cystica, has been reported to be an important risk factor for the development of HBS, with an incidence of 25–90% [13, 23].
As expected, serum calcium and phosphate levels decrease rapidly after parathyroidectomy within the first 3–4 days, but may decrease further after the fourth day in patients with HBS [15], although minimal levels of calcium were detected even 3 weeks after surgery, underlining the importance of intensive “long-term” monitoring of patients for up to 3 weeks after surgery [21].
The treatment of HBS is aimed in the short term, primarily, at replenishing the circulating calcium deficit, and in the long term at normalizing bone turnover and remineralizing the skeleton.
Patients with severe hypocalcemia and symptoms of seizures, tetany or laryngospasm should be treated aggressively with intravenous calcium administration. Electrocardiographic monitoring is mandatory to avoid cardiac arrhythmias as a consequence of too rapid correction of hypocalcemia. By contrast, asymptomatic patients or those who have only mild symptoms of hypocalcemia (perioral numbness, paresthesia) can be treated with oral calcium and vitamin D. Among the different available oral preparations, calcium carbonate should be preferred, due to the highest percentage of elemental calcium (40%) and because of its capacity to bind dietary phosphate and consequently inhibit its absorption [11, 17]. Hypomagnesemia should be treated with intravenous infusion of magnesium sulfate or magnesium oxide orally, since hypocalcemia does not resolve until the magnesium deficiency has been corrected [11, 15, 17].
All patients should receive vitamin D supplements, since vitamin D depletion is associated with an increased risk of developing postoperative hypocalcemia and HBS [11, 28, 29].
Bisphosphonates are widely used in the management of osteoporosis and bone disorders, due to the ability to inhibit osteoclastic bone resorption and to increase the mineralization of bone [30]. In this context, bisphosphonate treatment may have a beneficial effect on the severity and duration of HBS, but may exacerbate postoperative hypocalcemia by reducing bone resorption [30]. Although some small series reported encouraging results [31, 32], data on the preoperative use of bisphosphonates are conflicting and there are no randomized trials addressing the preoperative use of bisphosphonates in patients with hyperparathyroidism.
References
1.
Mittendorf EA, Merlino JL, McHenry CR (2004) Post-parathyroidectomy hypocalcemia: incidence risk factors, and management. Am Surg 70:114–120PubMed
2.
Hamouda B, Ben Dhia N, Aloui S et al (2013) Predictors of early post-operative hypocalcemia after parathyroidectomy for secondary hyperparathyroidism. Saudi J Kidney Dis Transpl 24:1165–1169CrossRefPubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree