Definition and Prevalence
Hypertension is a very prevalent disorder affecting about 1 billion people worldwide1 and, as such, it is the most common modifiable risk factor for conditions such as atherosclerosis, stroke, heart failure, atrial fibrillation, diabetes mellitus, sudden cardiac death, acute aortic syndromes and chronic kidney failure and may cause death and disability in patients of all ages.2
It is thought to affect up to 70% of individuals over the age of 65 years. The exact prevalence of hypertension varies with the age, race and the overall health status of the population studied, and also the blood pressure cut-offs points used to define hypertension. Hypertension in elderly patients is a complex cardiovascular disorder that affects women more than men and occurs in essentially all races, ethnic groups and countries. Although it appears to be underdiagnosed in general and particularly among women, minorities and underserved populations, clearly it is also undertreated. Elderly persons are more likely to have hypertension and isolated systolic hypertension (ISH), target organ damage (left ventricular hypertrophy, renal impairment and albuminuria, hypertensive retinopathy) and clinical cardiovascular disease (CVD), to develop new cardiovascular (CV) events and are less likely to have hypertension controlled.
An international consensus exists about the limits of normal values for brachial blood pressure at 140/90 mmHg.3 All define a blood pressure of 160/100 mmHg as requiring therapeutic intervention and 200/120 mmHg as very high risk requiring immediate management. There is less consensus on the cut-offs for blood pressure measured by other techniques. Many groups are now beginning to recommend the use of ambulatory blood pressure monitoring (ABPM) and the recent UK NICE guidelines have suggested that it has a primary role in the diagnosis of hypertension given its superior predictive value for CVD events compared with rather variable brachial measurements and its ability to counter stress-induced or ‘white coat’ hypertension.4
The US guidelines5 introduced the concept of pre-hypertension, representing a systolic blood pressure (SBP) of 120–139 mmHg or diastolic blood pressure (DBP)of 80–89 mmHg, previously classified as ‘normal’ or ‘high normal’ blood pressure. Other guidelines recognize pre-hypertension as a potential risk factor but stress the role of CVD risk assessment and risk calculation as the primary guide to a requirement for any intervention—lifestyle or therapeutic. Pre-hypertension was introduced, in part, on findings of the Framingham Heart Study (FHS) suggesting that normotensive individuals at age 55 years have a 90% lifetime risk of developing hypertension.6
The recommendation was based on the results of 30 worldwide clinical trials conducted in 1997 and a report estimating that the risk of cardiovascular mortality doubles with each 20/10 mmHg rise in blood pressure, starting at levels as low as 115/75 mmHg.7 In addition, evidence has accumulated which classifies individuals with comorbidities and an SBP >130–139 mmHg as suboptimal. These conditions include heart failure and left ventricular dysfunction, diabetes mellitus, chronic kidney disease and established CVD conditions such as coronary artery disease (CAD), peripheral arterial disease (PAD) and carotid artery disease.
A long standing controversy exists about hypertension in the elderly and some argue that usual definitions of hypertension and target BP levels might not be applicable to the elderly hypertensive population. The higher prevalence of hypertension in the elderly partially reflects the increase in the prevalence of arterial stiffening and thus changes in reflection pressure wave timing. The new generation of hypertension diagnostic devices specifically measure pulse wave reflection, velocity and pulse amplification parameters. There is no consensus on target values or optimal measures for pulse wave diagnostics as yet although all studies show that either directly measured or inferred central blood pressures (ascending aortic arch) are better predictors of outcomes than brachial measurements. As this technology is not widely available, older measures of specific subtypes of hypertension are useful.
Pathophysiology
Blood pressure regulation is a complex process, subject to multiple interacting physiological systems, and also lifestyle and genetic factors. In its simplest conceptualization, the cardiovascular system is governed by Ohm’s law, which, when adapted to a haemodynamic system, states that flow (Q) is proportional to the pressure gradient (ΔP) and inversely proportional to the resistance (R) across a conduit.
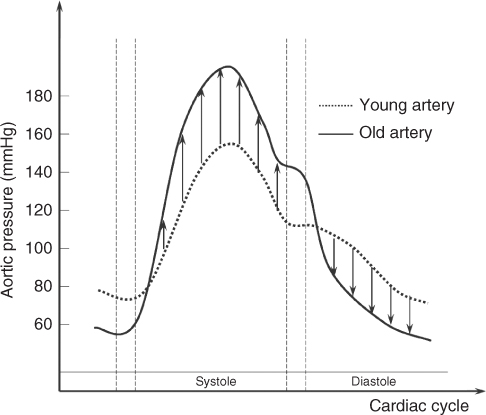
In terms of the cardiovascular system, BP is the product of cardiac output and vascular resistance. Since cardiac output does not increase with age, hypertension in the elderly is, to a large extent, a result of increased vascular resistance. In combined systolic and diastolic hypertension (SDH), the problem arises at the site of the resistance arterioles, the smaller muscular vessels where 80–90% of arterial resistance occurs. Increased constriction at this level affects both SBP and DBP. In contrast, ISH develops as a result of large arteries that have become less compliant and therefore less able to accommodate volume changes. In young normotensive individuals, large elastic vessels contribute little resistance to blood flow. During systole, the aorta and other large arteries expand to accommodate the stroke volume, which attenuates the rise in intra-arterial pressure. During early diastole, elastic recoil of large arteries sustains forward flow, augmenting the DBP despite runoff into arterial branches. Age-related loss of elasticity increases vascular impedance, resulting in a more rapid rise in blood pressure during systole and to a higher level. The higher peak pressure, coupled with diminished elastic recoil, results in rapid runoff to the periphery, resulting in lower DBP (Figure 40.1). A low DBP is not entirely benign. Since myocardial perfusion occurs during diastole, diastolic hypotension may result in subendocardial ischaemia. While other constituents no doubt factor into the pathogenesis of hypertension, age-related loss of arterial elasticity successfully predicts widening of the pulse pressure (PP), ISH and the plateau in DBP that develop with ageing. Figure 40.1 depicts these changes over the course of a single cardiac cycle. Ageing blood vessels undergo a host of structural and functional changes, resulting in decreased compliance and increased resistance to flow. These changes particularly affect the intima and media of large arteries. With age, elastic fibres progressively decrease in number and elasticity and the collagen matrix increases. This fibrous transformation results in arteriosclerosis and is compounded by calcification and an increase in the number and size of vascular smooth muscle cell. The combined effect is a fall in the total cross-sectional area of peripheral vasculature. Furthermore, the dynamic nature of endothelial-derived vasoactive substances that control vascular tone is also affected by age. The delicate balance between vasoconstricting agents (such as endothelin and angiotensin II) and vasodilating agents (such as prostacyclin and nitric oxide) is offset. Nitric oxide (NO), previously termed endothelial-derived relaxing factor (EDRF), is a potent vasodilator that has been extensively studied. An age-associated decline in NO-mediated vasodilatation has been demonstrated.8 A decreased secretion of NO and also a blunted response to NO have further been documented. Endothelial dysfunction, possibly as a direct effect of elevated peak pressure, inhibits secretion of these compounds.9 It remains unclear to what extent the imbalance of endothelial-derived vasoactive compounds is a cause or effect of high blood pressure, but impairment of effective vasodilator agents, in the absence of appropriate compensatory mechanisms, will result in increased vascular resistance. The endothelium also secretes a number of factors that act on smooth muscles in an autocrine manner. These include interleukin-1 and insulin-like growth factor. In vitro, these influence the migration and proliferation of smooth muscle cells, which in turn increase vascular rigidity and decrease lumen size.
Figure 40.1 Blood pressure changes in an old versus a young artery during a cardiac cycle. The arrows indicate increased pressure during systole and decreased pressure during diastole that older arteries experience due to arteriosclerosis.
Despite increased levels of serum norepinephrine that occur in the elderly, the role of the sympathetic nervous system in the pathogenesis of hypertension appears to be more complex than mere overstimulation. The sympathetic nervous system has little clinical impact on older normotensive subjects, even with increased levels of serum norepinephrine. This is due to decreased adrenergic receptor function. Downregulation of β-adrenergic inotropic, chronotropic and vasodilatory response, and also α-adrenergic vasoconstrictor response, has been documented in the elderly. With receptor downregulation in the face of increased norepinephrine release, α1-adrenergic vascular tone is comparable in old and young normotensive subjects. It has been proposed by some experts that older hypertensive subjects have a relatively less degree of suppression of α1-adrenergic relative to β2-adrenergic activity10 and age-related hypertension is in part due to diminishing β-mediated vasodilatation whereas α-mediated vasoconstriction continues relatively unabated. Similar findings have been observed in animal studies. Decreased carotid baroreceptor sensitivity and responsiveness occur with age. Consequently, a larger change in blood pressure is needed to trigger the appropriate compensatory response. The impaired reflex is manifested clinically as wide blood pressure fluctuations in the elderly compared with the young, and also increased susceptibility to clinically significant orthostatic hypotension and postprandial hypotension. The age-related baroreceptor reflex dysfunction is not necessarily limited to hypertensive persons alone, but decreased vascular distensibility at the carotid sinus, as seen in hypertensive subjects, is likely to play a central role in the process and many antihypertensive medications will further exacerbate the condition.
Ageing kidneys undergo multiple changes, which may affect blood pressure regulation. A sodium load is secreted less rapidly and less completely as renal function declines. Similarly, the elderly are more sensitive to free water depletion or repletion than the young. Angiotensin II promotes sodium reabsorption from the distal tubules directly and indirectly through aldosterone release and stimulation of the autonomic nervous system. The renin–aldosterone–angiotensin axis, however, is less responsive with age. There is a decrease in serum renin levels and activity, which may be the result of decreased functional glomeruli and a decrease in serum angiotensin II and aldosterone levels. The net effect of these changes is towards sodium retention. Free water retention ensues to maintain sodium homeostasis. It has been suggested that chronic extracellular volume expansion due to sodium and water retention leads to increased vascular resistance through the mechanism of autoregulation of organ blood flow. These observations are consistent with the high prevalence of salt sensitivity among older hypertensive individuals. Atrial natriuretic peptide (ANP) is released primarily from the atria in response to stretch due to volume overload. ANP acts both as a peripheral vasodilator and as a natriuretic/diuretic hormone. Brain natriuretic peptide (BNP) was initially identified in the brain but is also present in the ventricles. It is homologous to ANP and its serum concentration is normally approximately one-fifth that of ANP. In heart failure, levels of BNP can increase dramatically. A simple serum assay has been devised for the measurement of BNP and is now commonly used in the management of heart failure.
Several variants of ANP and related hormones have been identified. Of note is a hormone with a digitalis-like effect. This putative hormone appears to be ouabain or an isomer of ouabain and binds the digitalis receptor on the sodium potassium adenosine triphosphatase pump (Na-K-ATPase) in an inhibitory manner. This hormone differs from ANP in that it increases vascular resistance. A proposed mechanism is that the Na-K-ATPase inhibitor facilitates renal sodium excretion but also diminishes intracellular sodium release, resulting in increased concentrations of sodium in smooth muscle cells. Passive sodium–calcium exchange subsequently results in increased intracellular calcium and, therefore, vascular tone.11, 12 These mechanisms may explain the high incidence of salt sensitivity in subjects with essential hypertension, but more investigation is needed to determine fully the role that this mechanism plays in the pathogenesis of hypertension. Not all the aforementioned mechanisms have conclusively been shown to be age-related changes, independent of disease and lifestyle influences. In some populations, the incidence of hypertension changes little with age and the overall prevalence is low. To some extent, hypertension is an affliction of modern society. Until very recent history, humans employed the hunter–gatherer lifestyle for survival. Such ‘primitive’ peoples experienced vigorous daily physical activity and a diet rich in potassium and fibre and low in fat and sodium. Patterns of Nature led to periods of diminished food intake and obesity was virtually unheard of in these communities. Modern-day populations who enjoy relatively low incidences of hypertension tend to practice daily routines that more closely resemble the primitive lifestyle of old, particularly with regard to nutrition and physical activity. The blood pressure profiles of immigrants from such regions, however, may change over the course of a few generations to resemble that of the host community. The overabundance of foods rich in sodium, calories and fat in westernized societies, coupled with sedentary levels of activity, without doubt contributes to the epidemic of obesity and hypertension. With the abundance of effective medications available for the treatment of hypertension, these potentially modifiable risk factors receive far less attention than they deserve. Finally, there is a clear genetic role in the development of hypertension in some families. Such individuals are likely to develop hypertension early in life. The genetic contribution is complex, involves multiple interacting genes and is not fully understood at this time. Genetic factors are perhaps the strongest non-modifiable risk factor for hypertension.
Related Clinical Entities
Isolated Systolic Hypertension (ISH)
SBP rises gradually throughout adult life, whereas DBP peaks and plateaus in late middle-age, declining slightly thereafter. Therefore, the proportion of hypertensive patients with ISH increases with age, from 65% of patients with hypertension older than 60 years of age and over 90% in patients older than 70 years of age. The prevalence of ISH is higher in women than in men, whereas the proportion of hypertension attributable to ISH in older adults is similar across racial and ethnic groups. Of note, in decades past, the apparently inexorable rise in SBP with increasing age fostered the view that this was an adaptive response essential to support organ perfusion and an empirical formula ‘100 + age’ was often used to estimate the ‘appropriate’ SBP. However, data from the FHS and other epidemiological investigations provide compelling evidence that SBP is a strong independent risk factor for incident CV events in all decades of life.13 Hence the above formula should be discarded. ISH actually represents the outcome of hyaline change and increased arteriolar tone in the microvasculature with increased collagen deposition, loss of elastin and changes in endothelial function. Changes in endothelial function are driven by classical CV risk factors and some advocate its measurement as a surrogate for atherosclerotic disease burden. ISH also closely corresponds to increased wave reflection and studies of pulse wave parameters including differences between central and peripheral blood pressure may have prognostic and therapeutic consequences.14
Pulse Pressure
After age 70 years, diastolic hypertension accounts for less than 10% of all patients with hypertension. In addition, the relationship between DBP and CV risk is bimodal in older individuals, with DBPs of greater than 90 mmHg associated with similar increased risk as that associated with DBPs lower than about 70 mmHg.15 As a result, at any given level of SBP, CAD risk increases as DBP decreases.16, 17 An important implication of this observation is that pulse pressure (i.e. difference between SBP and DBP), which increases with age and is a measure of the degree of age-related vascular stiffness, emerges as a potent risk factor for CAD events in older individuals. Pulse pressure has been identified as a stronger risk factor than SBP, DBP or mean pressure in older adults in some studies.16, 17 In the FHS, with increasing age, there was a gradual shift from DBP to SBP and then to PP as the strongest predictor of CAD risk. In patients younger than 50 years of age, DBP was the strongest predictor. Age 50–59 years was a transition period when all three BP indexes were comparable predictors, and from 60 to 79 years of age, DBP was negatively related to CAD risk so that PP became superior to SBP.18 However, a falling DBP in the elderly correlating to an increase in PP is a bad prognostic sign.
Special Populations
From the standpoint of epidemiology, pathophysiology and treatment, there are important subgroups with distinctive characteristics, including elderly women, blacks, Hispanics and Asians, that require additional focus. Hypertension prevalence is less in women than in men until 45 years of age, is similar in both genders from 45 to 64 years of age and is much higher in women than men older the 65 years of age.19 Age-adjusted hypertension prevalence, both diagnosed and undiagnosed, from 1999 to 2002 was 78% for older women and only 64% for older men.20
Secondary Hypertension
Although most hypertension (80–90%) is essential, that is, its pathophysiological cause is unknown, secondary causes of hypertension are being increasingly recognized as contributing to morbidity. Renal artery stenosis (RAS) is more common than is usually thought and is often associated with PAD, especially if associated with a reduction in estimated glomerular filtration rate (eGFR), signs of (micro)albuminuria. Although not contributing directly to hypertension as is the case in severe stenotic disease (>85%), it is a risk factor for angiotensin-converting enzyme inhibitor (ACE-I)/angiotensin-II receptor blocker (ARB)-induced nephrotoxicity. Any patient with these risk factors should have renal function assessed two weeks after starting an ACE-I/ARB or clinicians should be wary of slow progressive decreases in eGFR as a manifestation of RAS. Most endocrine causes of hypertension are rare (phaeochromocytoma, Cushing’s disease or Conn’s syndrome) but adrenal mineralocorticoid hyperplasia is common.21 This manifests as aldosteronaemia allied with low renin and its prevalence varies in surveys from 5 to 10% of patients with hypertension. An increased prevalence of low-renin hypertension is found in the elderly, patients with diabetes and West African-derived populations. Most is not caused by adenomas but by generalized adrenal hypertrophy and can be diagnosed by finding a moderately raised aldosterone:renin ratio in a random sample taken in patients not receiving beta-blockade It often responds well to treatment with an aldosterone antagonist.
Resistant Hypertension
Most hypertension is treated with polypharmacy as each individual agent reduces blood pressure by about 10%. Resistant hypertension is formally defined as a BP >140/90 mmHg after treatment with three antihypertensive drugs.5 Most commonly it is caused by poor compliance with polypharmacy, but other causes include ISH and contributory comorbidities including secondary hypertension and neurological hypertension. This can include anxiety states (see white coat hypertension in the section Clinical assessment and diagnosis, below), but also includes dysregulation of central mechanisms of BP regulation. The commonest cause of central dysregulation is sleep apnoea syndrome, which is often associated with obesity and can be diagnosed by oximetry studies and treated with continuous positive airways pressure maintenance (CPAP) allied commonly with weight loss.22
The Effect of Treating Hypertension in the Elderly—An Overview of Clinical Trials
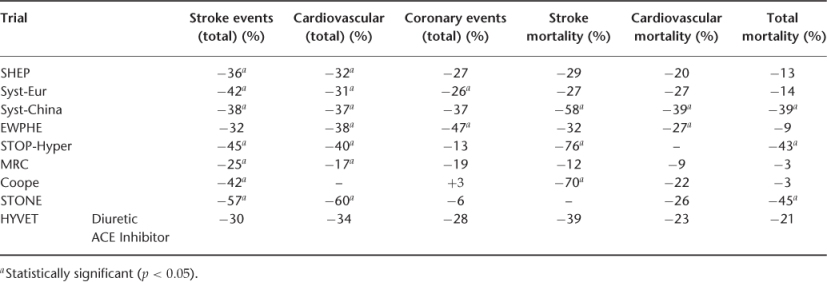
Salient features of the pivotal clinical trials discussed below and a summary of their findings are given in Tables 40.1 and 40.2.
Table 40.1 Characteristics of treatment trials that predominantly involved older hypertensive individuals. Trial acronyms and references are found in the body of the text.
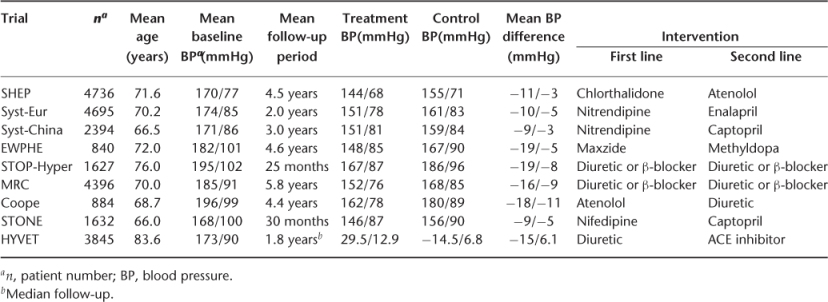
Table 40.2 Outcome of treatment trials. Trial acronyms and references are found in the body of the text.
The benefit of treating hypertension in the elderly was evident as early as 1967. The Veterans Administration Cooperative study, which was published in three parts between 1967 and 1972, documented the benefit of treating severe23 and mild24 diastolic hypertension. In subjects over the age of 60 years, a 70% reduction in the incidence of stroke and 52% reduction in cardiovascular events were observed in the treatment group.25 Similar favourable outcomes were documented in the Australian Therapeutic Trial in Hypertension, where a 33% reduction in stroke and 18% reduction in CAD were noted in the treated subgroup age 60–69 years, compared with the placebo group.26 In the Hypertension Detection and Follow-up Program, there was a 17% reduction in all-cause mortality after a 5 year follow-up period of patients aged 60–69 years, treated for mild diastolic hypertension.27
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








