Estimated diagnoses of HIV infection by age, 2011, United States.
Screening and diagnosis
Missed opportunities for screening: is it HIV or is it aging?
Detection of HIV infection is the obvious starting point for prevention and treatment. However, older individuals are less likely to be screened for HIV infection compared to younger people, and as a consequence they present later and with more advanced disease.[5, 6] The diagnosis is also obscured when symptoms and signs of immunodeficiency in older adults mimic normal aging or other medical problems that are common in the elderly.[7] Awareness of symptoms and signs associated with HIV infection, both acute and chronic, increases the likelihood of proper testing being performed, and the identification of patients who will benefit from early treatment, counseling, and other interventions to avert further transmission.
Routine HIV testing
The CDC and the US Preventive Services Task Force recommend routine, voluntary opt-out HIV screening for all adults ages 13–64 regardless of risk factors.[8, 9] Although there remains an important role for a detailed sexual and substance use history, screening independently of risks improves identification of HIV-infected individuals. It is notable that these recommendations do not include routine testing in persons 65 years of age or older despite the hesitation of adults and their providers to correctly appreciate risk factors for infection.[5, 6] Many experts (these authors included) recommend extending routine HIV screening beyond the age of 65 years. Clinicians must appreciate that older persons can be sexually active, and should be comfortable and adept at taking a sexual and substance use history from older patients.[10]
HIV testing relies on detection of antibodies to HIV, the virus itself, or both.[11] The fourth-generation assay that is now recommended by the CDC for universal use is a combination HIV antibody and antigen (p24 antigen) assay that detects antibodies to both HIV-1 and HIV-2. It is commercially available and in wide use. This test reduces the window period from acquisition of HIV to laboratory detection of infection to 4–12 days (Figure 24.2). Negative results can be considered conclusive unless a potential exposure to HIV occurred within the two weeks prior to the test. If the antibody/antigen screen is positive, follow-up testing including a nucleic acid test for HIV RNA is performed.
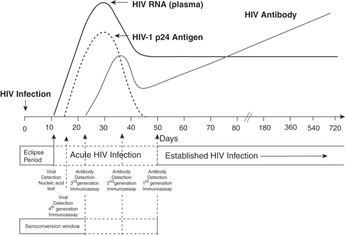
Sequence of appearance of laboratory markers of HIV-1 infection.
Acute HIV infection is symptomatic in most cases and may present as fever, generalized lymphadenopathy, viral exantham, and severe fatigue. As these are nonspecific symptoms especially during flu season, a careful history should be taken to assess for possible HIV exposure. Although the fourth-generation HIV Ag/Ab test reduces the window period between infection and test positivity, when acute HIV is suspected, an HIV RNA test is most appropriate.
Clinical characteristics
At diagnosis, older adults present with characteristics of more advanced or severe HIV disease compared with younger adults.[12] They consistently have a lower median CD4+ cell count at the time of diagnosis, and a greater proportion have an acquired immune deficiency syndrome (AIDS)-defining diagnosis at or within three months prior to presenting for HIV care.[13] Delayed testing due to a low clinical suspicion for HIV infection contributes to advanced presentation at time of diagnosis. While HIV disease can present in myriad ways, certain clinical situations should prompt HIV testing (Table 24.1).
Infections
A number of opportunistic infections are associated with the immune deficiency that characterizes progressive HIV disease. Development of any of these is a clarion call for HIV screening. Among these are oral or esophageal candidiasis (thrush), varicella zoster infections, bacterial pneumonia, and pyomyositis. More pathognomonic for AIDS are rarer conditions such as pneumocystis pneumonia, cryptococcal meningitis, toxoplasmosis encephalitis, cytomegalovirus (CMV) retinitis or enteritis, and disseminated mycobacterium avium complex. Pneumocystis pneumonia is associated with late diagnosis of HIV/AIDS and may be unrecognized, with catastrophic consequences. It classically presents with progressive symptoms of cough (productive of scant, white/gray sputum), dyspnea, hypoxia, and diffuse pulmonary infiltrates, although radiographic findings can be minimal even in the face of severe respiratory compromise.
Recurrent bacterial pneumonia, skin and soft tissue infections with MRSA or other bacteria, and perirectal abscess or fistula may also be the presenting manifestations of HIV infection.
In most of the world, tuberculosis is the most common and lethal opportunistic condition complicating AIDS. All patients with either active tuberculosis or latent infection, as determined by a positive purified protein derivative (PPD) test or blood interferon gamma release assay, should be tested for HIV infection. Those diagnosed with other sexually transmitted infections such as gonorrhea, chlamydia, syphilis, hepatitis C virus (HCV), and hepatitis B virus (HBV) are almost by definition at risk for HIV infection.
Neurologic conditions
Neuropathy and dementia, although common in elderly patients, are also prevalent in those with HIV infection.[14–16] HIV-associated dementia classically presents with early behavioral changes and occasionally includes focal neurologic findings such as isolated weakness or aphasia. Peripheral neuropathy in the setting of HIV can present as a painful distal sensory process, or may appear almost indistinguishable from diabetic neuropathy. Early antiretroviral medications have left a legacy of peripheral neuropathy that produces burning, persistent pain and loss of sensation, posing risks for foot sores and infection; newer medications are less likely to cause nerve disease.
HIV-related toxoplasmosis, progressive multifocal leukoencephalopathy, bacterial and viral meningitis, and acute HIV headache continue to pose diagnostic and management challenges.
Malignancies
The immune system provides surveillance not only for infectious pathogens but also malignant cells. As such, deficiencies in immune function are associated with increased risk of neoplasm, particularly those that have a viral etiology.[17] In the setting of HIV, a number of cancers are more common, including non-Hodgkin’s lymphomas, lung cancer, central nervous system lymphomas, testicular cancer, and Kaposi’s sarcoma. Cancers due to human papilloma virus (HPV) – including those involving the anus, vulva, or mouth – are also seen more commonly in men and women with HIV infection. Detection of any of these malignancies should prompt HIV testing.
Other conditions
Symptoms of acute HIV: fatigue, headache, weight loss, diffuse lymphadenopathy …
A number of dermatologic conditions are associated with HIV infection, including severe psoriasis, seborrheic dermatitis, common warts, condylomata acuminata, molluscum contagiosum, and purigo nodularis. Oral hairy leukoplakia is a viral mediated nonmalignant condition affecting the lateral aspects of the tongue and presents as a shiny white tiger-striping that is not easily removed. Leukoplakia and erythroplakia are oral premalignant conditions that should prompt monitoring and referral.
Laboratory abnormalities
Common but nonspecific laboratory findings in persons with advanced HIV infection include anemia, thrombocytopenia, and leucopenia, specifically lymphopenia. An increase in globulin is often seen in HIV-positive patients.[18] Isolated thrombocytopenia can be seen in persons with HIV infection and/or advanced viral hepatitis.
Aging process and HIV infection
There is growing concern that HIV-infected persons experience aging differently than those without the virus.[19] A number of studies document comorbidities and frailty rates that are higher among HIV-infected men and women compared to uninfected controls.[19–22] In a comparison of a large cohort of HIV-infected and uninfected patients receiving care at two Boston hospitals, those infected with HIV had an almost twofold greater risk of acute myocardial infarction than uninfected patients, with the difference between the groups increasing at older ages.[23] Other studies have demonstrated an increase in carotid artery intima-media thickness, coronary artery calcium deposition, and non-calcified coronary plaque (increased risk of rupture compared to noncalcified plaque) in HIV-infected persons.[24, 25] HIV-infected men and women have also relatively high rates of diminished bone density and nontraumatic fractures, as well as neurocognitive impairment.[26, 27] An analysis of data collected during the Men’s AIDS Cohort Study (MACS), a large multi-center longitudinal observational study of HIV-infected and uninfected men who have sex with men (MSM) in the United States, found significantly higher rates of frailty (defined as having ≥3 of the following: low grip strength; slow four-meter walking speed; low physical activity; exhaustion; and unintentional weight loss of >10 pounds) among the HIV-positive men at each decade of life past 50 years of age.[28]
That HIV-infected individuals experience conditions associated with aging at rates that exceed those uninfected should not be a surprise, given the higher rates of smoking, substance abuse, poverty, and similar factors among those living with the virus. Studies that adjust for such confounders typically find that the associations between HIV and comorbidity are attenuated.[25] However, several lines of data strongly suggest that HIV infection and its treatment do have a direct role in age-related disease. In general, markers of immune activation are elevated in HIV-infected patients, as are those that assess inflammation.[29, 30] Such markers of inflammation, including C-reactive protein (CRP), interleukin 6 (IL-6), and D-dimer have been associated with mortality and non-AIDS morbidity in HIV-positive cohorts.[31] Similarly, altered gut integrity has been demonstrated in HIV-infected persons, leading to microbial translocation – an additional contributor to the inflammatory state.[32] Common coinfections in HIV-infected patients, such as hepatitis C virus (HCV) and CMV, may also play a role by triggering additional immune activation and inflammation.[33] Further, there is evidence that traditional risk factors for disease, such as smoking, may have a greater impact on cardiovascular and pulmonary health among HIV-infected patients than those uninfected.[34]
HIV therapies have led to profound improvements in survival and quality of life but may have long-term consequences. LDL cholesterol and triglyceride levels are increased by many commonly used antiretrovirals; abacavir and protease inhibitors have been associated with an increased risk of CVD in some but not all large cohort studies.[35, 36] Renal complications develop in a small but significant minority of patients treated with tenofovir; it can also reduce bone density. Tenofovir can rarely cause Fanconi syndrome, but it can also exacerbate preexisting renal disease. All patients who take this very effective antiretroviral should be monitored with serum creatinine and urine protein/creatinine ratio every three to six months. The renal effects of tenofovir are magnified because it is excreted by renal tubules and can accumulate and cause additional toxicity if renal function is impaired. Despite these concerns, accumulated data, including examination of treatment interruptions, make clear that uncontrolled HIV itself presents a greater risk for CVD, renal, hepatic, and other end-organ diseases, trumping any contributions by ART.[37, 38]
Management considerations
With HIV-infection now a long-term chronic condition for most patients, the management of this disease has started to shift toward primary care providers. Although many patients rely on their HIV specialist to attend to their general health needs, or see both a specialist and a primary care clinician, others have their HIV care provided by their primary care clinic. The clinician responsible for managing HIV, whether specialist or generalist, must be well versed in HIV care including relevant guidelines regarding HIV treatment and opportunistic infection prophylaxis.[47] Clinics providing HIV care must also be prepared to handle psychosocial aspects of HIV management.
Regardless of specialty of the clinician, the provision of HIV care must address HIV and related diseases as a syndrome, in the method familiar to geriatrics. Implementing geriatric principles in HIV care has a particular role in managing treatment regimens and polypharmacy. Older patients require close surveillance for liver, renal, metabolic, endocrine, and hematologic abnormalities while on ART, with special attention paid to drug interactions between ART and medications for other conditions (Table 24.2).
|
|
|
|
|
|
Select conditions of particular importance in the management of the aging HIV-infected patient are discussed later in the following paragraphs. In addition, more general health maintenance of older patients, such as cancer screening and immunizations, must also be attended to.
Cardiovascular disease
As described earlier, HIV-infected adults are at increased risk for CVD, including heart disease and stroke, and have increased subclinical CVD related to age-matched controls. The etiology for this is unclear, but traditional and HIV-related risk factors are likely at play. Given that advanced age is a well-recognized risk factor for CVD, additional subclinical disease suggests the need for awareness of CVD risk in HIV-infected persons.
The management of risk factors for CVD can reduce clinical disease incidence for HIV-infected patients. A recent study from investigators at Kaiser Permanente in California found that over the past several years, the rates for stroke and myocardial infarction for HIV-positive patients has approached that of uninfected members – a reduction attributed to more aggressive risk factor management and earlier initiation of ART to control viremia.[39] Overall, these are reassuring outcomes for HIV-infected patients and punctuate the need to address well-recognized risk factors associated with cardiovascular disease such as obesity, hypertension, tobacco and substance use, and dyslipidemia.
Some underappreciated risks include renal disease, depression, and toxic levels of stress and trauma. In a Veterans Aging Cohort Study (VACS) reviewing 81,000 patients with HIV, renal disease (GFR <30) was associated with a hazard ratio of 5 for development of heart failure.[40] This group has also highlighted the importance of anemia as a harbinger of very poor outcomes among HIV-infected patients.[41] In another study from the VA, depression, which has increased prevalence in HIV-infected patients,[42, 43] was independently associated with heart failure and myocardial infarction, with a 31% increased risk above other known risk factors.[44] In addition to depression, stress and psychological trauma, both common in the HIV population, have been linked to adverse health outcomes and may influence CVD risk.[45, 46]
At present, the recommended management of CVD risk follows that for those without HIV infection, although some HIV clinicians favor a more aggressive approach. Drug–drug interactions, especially between statins and ART (e.g., lovastatin and simvastatin are contraindicated with protease inhibitors), must be recognized and drug selection and dosing adjusted accordingly.[47]
Renal disease
The 2009 Medical Monitoring Project evaluated the prevalence of chronic kidney disease (CKD) in the HIV-infected population and emphasized the importance of recognizing impaired renal function. These data estimated that age older than 60 years was associated with a hazard ratio (HR) of 7.8 for development of CKD, defined in this study as glomerular filtration rate (GFR) <60 mL/min/1.73 m2 using the MDRD.[48] Other risk factors for CKD were female gender (HR: 1.4), longer duration of HIV infection (HR: 1.4), CD4 <350 cells/mm3 (HR: 1.6), and AIDS (HR: 2.1). Causes of renal impairment in the setting of HIV infection include the virus itself. HIV replicates in the kidney, and moderate HIV-associated nephropathy improves with the start of HIV medications. Tenofovir can cause a Fanconi’s syndrome characterized by proteinuria, glycosuria, and phosphate wasting. This adverse effect accounts for less than 5% of cases of acute kidney injury in HIV-positive patients and is usually reversible.[49] The protease inhibitor atazanavir can crystalize in the urine and form kidney stones.[50] Non-HIV-related etiologies of renal problems include hypertension, diabetes, and nonsteroidal anti-inflammatory use.
Recognition of CKD in the HIV-infected population is important, given the major role of renal function in medication clearance and the resultant risk of drug toxicity from pharmacologic treatment for HIV and other comorbidities.
Liver disease
Hepatitis is an important predictor of mortality in the HIV-infected population; liver disease in HIV-infected patients is associated with increased hospitalization, morbidity, and mortality.[51] Risk for liver disease in HIV-infected patients is multifactorial. Infection with hepatitis B and C, alcohol use, diabetes, and rapid weight gain all contribute. Fatty liver disease is not uncommon. Additionally, older patients are more likely to have end-stage liver disease compared with younger patients due to longer or more rapid courses of hepatitis infection. Hepatotoxicity due to multidrug ART is rare but can occur. Awareness of the presence of liver disease is important for providers when managing complicated medication regimens with hepatic clearance as well as for anticipating prognosis. Referral for treatment of hepatitis C with direct acting agents is essential in HIV patients; staging of disease and vaccination against hepatitis A and B are responsibilities of the primary care physician. Screening for hepatitis B should be initiated as soon as HIV is diagnosed, and management or referral should be initiated as soon as possible, because hepatitis B–related cirrhosis and hepatocellular carcinoma in HIV-infected patients are significantly more common in the older patient. Treatment of hepatitis B in HIV-infected patients requires two nucleoside agents, as compared to only one in most non-HIV-infected patients. Screening for hepatocellular carcinoma (HCC) in the older patient involves liver ultrasound every six months.
Bone health and fractures
Low bone mineral density (BMD) is prevalent in HIV-infected persons. Bone loss may be due to ART, as well as traditional osteoporosis risk factors such as low levels of vitamin D, low body mass, alcohol use, corticosteroids, and proton pump inhibitors. Fracture rates in the HIV-infected population are estimated to be 30%–70% higher than in age-matched controls.[52] In older patients, this can greatly impact function and independence.
ART initiation is associated with a sharp decline in BMD.[53] Patients may experience a decrease in BMD from 2% to 6% over the first two years after initiation of ART, a decline that is similar to that experienced as a result of menopause and is independent of the ART regimen selected. Recent research suggests that supplementation with vitamin D and calcium may attenuate bone loss.[54] In a clinical trial of 165 patients started on efavirenz/emtricitabine/tenofovir, bone loss at the hip was 50% lower in the group receiving 4,000 IU of vitamin D and 1,000 mg of calcium daily. Supplementation with daily calcium (1,000 mg–1,500 mg) and vitamin D (800 IU–1,000 IU) for all HIV-infected patients has been suggested, although this has not been incorporated into treatment guidelines.[52]
Screening for bone disease with dual-energy x-ray absorptiometry (DXA) is currently recommended for women ≥65 years old, men ≥70 years old, and any person with a fragility fracture regardless of age.[55] If additional risk factors are present, DXA scanning should be considered at earlier ages. Currently, HIV infection is not considered a risk factor for bone loss; however, some experts recommend DXA for all HIV-infected postmenopausal women, as well as men ≥50 years old, due to the high incidence of BMD in this population.[52]
Treatment recommendations for bone loss are consistent with those published by the National Osteoporosis Foundation.[55] Briefly, patients who have a T-score at the hip, femoral neck, or lumbar spine less than or equal to –2.5 or have a history of fragility fracture, should be considered for pharmacologic treatment. Patients should be reevaluated every two to five years based on the proximity of their results to treatment thresholds. Fracture risk should be calculated for all patients with osteopenia, using the World Health Organization (WHO) Fracture Risk Assessment Tool (FRAX) to further determine potential candidates for pharmacologic treatment.[56] As with all patients with severe bone disease, rheumatologists and endocrinologists play a significant role in comanaging these patients, in part because HIV is associated with hypogonadism at a higher rate than in non-HIV-infected persons
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




