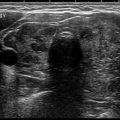
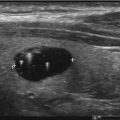
Fig. 2.1
The thyroid gland is inferior to the thyroid cartilage anterior to the tracheal rings. A pyramidal lobe is seen in approximately 50% of the population [5]
Postpartum : The thyroid gland’s final anatomical location is anterior to the trachea and caudal to the thyroid cartilage. The adult thyroid gland consists of a right and left lobe, bridged together by a thin and often impalpable strip of thyroid tissue called the isthmus.
Thyroid nodules are common in the general population and have a reported prevalence of 70% by imaging studies [7, 8] and 7% by palpation [9–12]. Thyroid nodules are typically nonfunctional, frequently discovered incidentally, with environmental and genetic conditions predisposing them to malignancy. To properly identify malignancy risks, work-up should include a thorough history, a physical exam, and thyroid imaging.
History: Since most thyroid nodules are detected incidentally by exam or imaging and most nodules are benign, directed questions can assist in determining malignancy risk and aggressiveness of follow-up and therapy. For instance, an adult patient with palpitations, heat intolerance, tremor, anxiety, diarrhea, and a thyroid mass is suspect of a toxic nodular thyroid, a benign process. The same findings in a 13-year-old should raise concern of malignancy due to a 26% malignancy risk in those under the age of 17 regardless of the functionality of the nodule [13, 14]. Other risk factors for malignancy in a patient’s history include a personal history of head and neck irradiation, family history of thyroid cancer, age of puberty, and history of thyroid disease [15, 16].
A review of systems may also give important information of the aggressiveness of a tumor and the need for immediate surgical, radiotherapy, or chemotherapeutic intervention. For instance, symptoms of dysphagia, odynophagia, hoarseness, or aspiration of liquids are suggestive of recurrent laryngeal nerve involvement [17], while cough, dyspnea, hemoptysis, and stridor are suggestive of tracheal invasion [18]. Though very aggressive thyroid malignancy is rare, it is important to identify these patients as their prognosis is typically poor [19, 20].
A family history identifies genetic conditions linked to thyroid malignancy . These include conditions such as familial nonmedullary thyroid cancer (FNMTC) [21, 22], multiple endocrine neoplasia 2 (MEN2) [23], Cowden syndrome (PTEN hamartoma tumor syndrome) [24], Gardner syndrome [25], and familial adenomatous polyposis (FAP) [26, 27]. The detail of questioning should be determined by the patient’s risk factors. For instance, if the patient does not possess a family history of thyroid malignancy, questions related to MEN2 or FNMTC may be excessive. On the other hand, a patient with a family history of colon polyps should be questioned about Gardner syndrome or FAP, due to the increased risk of thyroid malignancy as noted in Table 2.1.
Table 2.1
Familial conditions which are associated with thyroid malignancy and the associated risk of malignancy
Condition | Risk of thyroid malignancy | Predominant thyroid cancer type |
|---|---|---|
MEN2 [23] | 90% | Medullary |
Cowden syndrome [24] | 38% | Follicular |
3–15% | FCD | |
0.4–12% | Papillary | |
Gardner syndrome [25] | 2% (predominantly women) | Papillary |
Physical Examination
To our knowledge, studies comparing the efficacy of different palpation techniques to identify thyroid structural disease have not been done. Palpation techniques typically develop through reading or from previous training. Regardless of which method is used, there are three key features of the physical exam: knowledge of neck anatomy, the examiner’s training, and the experience and comfort with his/her approach to the exam.
Anatomy: The normal adult thyroid gland is located inferior to the thyroid cartilage and anterior to the second and fourth tracheal rings. The gland is posterior the sternohyoid and sternothyroid muscles (also known as the strap muscles) and medial to the internal jugular vein and carotid artery bound by the pretracheal fascia (Fig. 2.2). Included within the pretracheal fascia is the thyroid gland, trachea, and esophagus. The gland is highly vascularized permitting direct hormone secretion into circulation. The recurrent laryngeal nerve and external branch of the superior laryngeal nerves innervate the vocal cords and are a source of morbidity during surgical thyroidectomy [28]. The four parathyroid glands, typically found posterior to the thyroid gland, are also a source of morbidity during thyroidectomies [29].
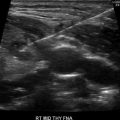
Fig. 2.2
Ultrasound image of the thyroid gland. T trachea, R right thyroid lobe, L left thyroid lobe, I thyroid isthmus, A carotid artery, SCM sternocleidomastoid muscle, E esophagus, V jugular vein
The thyroid has two lobes connected in the midline by an isthmus. The average anterior to posterior thickness of each lobe is <20 mm with a superior to inferior length of about 40–60 mm. The average weight of the thyroid gland is between 15 and 30 g in adult males and slightly heavier in females due to enlargement associated with menstruation and pregnancy. Thyromegaly is defined when the anterior/posterior or traverse lengths exceed 20 mm or when the parenchyma extends anterior to the carotid arteries.
Inspection: Inspection is typically more useful with large glands. The subject is told to tilt the head slightly upward which will better expose the neck and possible substernal glands. Thyroid size, shape, texture, mobility, and presence of visible nodularity should be observed and documented. A scar superior to the sternal notch, known as a necklace scar, indicates prior thyroid or parathyroid surgery. The gland should be viewed from the front and side of the patient. Shadows cast by light manipulation can exaggerate thyroid borders and texture. Sips of water by the subject cause a cephalad movement of the gland confirming its structure.
Palpation : Two different palpation techniques include thyroid examination facing the patient or from behind the patient. The subject should be warned prior to the procedure that a choking sensation may be felt, while the thyroid gland is palpated. If unable to tolerate, ultrasonography is an alternative to the physical exam.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree