Figure 177.1 Chest radiograph demonstrating diffuse infiltrates in a patient with rheumatoid arthritis with progressive disseminated histoplasmosis following initiation of treatment with a TNF-α inhibitor.
Diagnosis
The gold standard is the recovery of the organism, but this is time-consuming, requiring up to 30 days for identification of the organism.
Sputum cultures are not very useful in the cases of suspected acute pulmonary infection because the inoculum is not high enough and only rarely do patients have productive cough. In patients with acute disseminated histoplasmosis and in those with chronic pulmonary or cavitary infections, sputum cultures are frequently positive. When bronchoscopy and bronchoalveolar lavage are employed with appropriate stains, the sensitivity of respiratory secretions increases. Biopsy of accessible lesions (Figure 177.2) and bone marrow can be used in cases of disseminated infection.
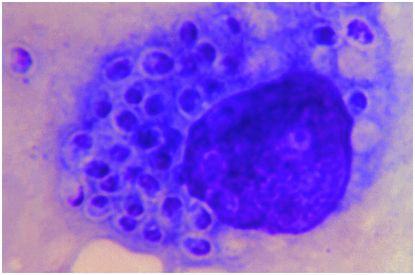
Figure 177.2 Histiocyte containing numerous yeast cells of Histoplasma capsulatum. Giemsa stain. (Public Health Image Library, Centers for Disease Control and Prevention [CDC], Dr. D. T. McClenan.)
Detection of histoplasma polysaccharide antigen in urine or serum offers high sensitivity and rapid diagnosis for patients with large inoculum acute pulmonary disease and those with PDH. Sensitivity for antigen detection is higher in disseminated infections than isolated pulmonary disease. The highest sensitivity of histoplasma antigen testing is in patients with AIDS and PDH when compared to other immunosuppressed or immunocompetent individuals with PDH. Earlier generation tests were characterized by a significantly higher sensitivity of the urine test when compared to serum testing. This does not appear to be the case with the newest generation of testing. As the levels of antigen are highest in the urine for most patients, urine testing is a helpful initial strategy. Antigenemia testing may be particularly useful in anuric patients. Antigenuria levels have correlated with disease severity and have been useful when monitoring treatment, since the levels decrease with successful therapy and increase with relapse.
Serologic complement fixation and immunodiffusion are also helpful in some cases and may be the only means by which an infection can be diagnosed in immunocompetent individuals. In immunocompetent patients, it frequently takes 2 to 6 weeks for the development of detectable antibodies. The use of antibodies for diagnosis of histoplasmosis is most helpful in chronic pulmonary histoplasmosis and for those with persistent symptoms following recent infection.
As in the case of antigen detection there is also clinical correlation between the severity of the disease and the antibody response. In immunosuppressed patients antibody responses may be weaker and in some cases undetectable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





