Hakaru Hashimoto is pictured here at 31 years old. It was at this age that he wrote his most famous work. (Picture is courtesy of The Japan Endocrine Society)
Early Life
Hakaru Hashimoto was born on May 5, 1881, in the village of Midai, Nishitsuge. He was the third son born to a family that had practiced medicine for generations within this small town [1]. Today, this historical village would be considered a part of the larger town of Iga Ueno. This castle town surrounded by mountains in the Kinki district was the birthplace of Iga Ninja and is where the Iga Ninja School was established in the fifteenth century. It was also the hometown of the famous Haiku poet, Basho Matsuo.
Hashimoto spent his childhood in the village of his birth and then left to enter the First Mie Prefectural Junior High School at Tsu [1]. This is around the time when he considered an education in medicine. He was in an environment that seemed to foster these early career aspirations given that many of his friends eventually went on to also become involved in medicine. More specifically, the influence of his grandfather, Gen’i Hashimoto, sealed Hashimoto’s fate as a physician. Gen’i was a well-known physician within the region who had studied Dutch medicine at the end of the Edo era [1] .
Hashimoto went on to attend the National High School at Kyoto, and in 1903, he entered the Department of Medicine at Kyusyu Imperial University in Fukuoka. Hashimoto was in the first graduating class in 1907. Following graduation from medical school, he entered the First Department of Surgery and studied under Professor Hayari Miyake for 4 years. It was here, while he was completing his studies in surgery, that Hashimoto encountered the thyroid glands of four women who had a completely distinct histopathology never before described [1–4] .
Life Overseas
After the publication of his original paper at the young age of 31 years, Hashimoto went to Germany for further study. He had a particular interest in pathology and worked under Professor Kaufman at Goettingen University, but his time in Germany was shorter than planned. After 2 years of living in Germany, he was forced to return to Japan in 1914 as a result of the outbreak of World War I in Europe [5] (Fig. 1) .

Fig. 1
Seen here is the hospital in Dr. Hashimoto’s hometown. This is his place of practice for most of his career and is where he performed his surgical procedures. (Picture is courtesy of The Japan Endocrine Society)
His Return to Japan
Hashimoto returned to Japan and joined his alma mater for a short time. However, due to financial pressures, he soon decided to move back to his hometown to take over the family practice [1]. He began his surgical practice in the spring of 1916 at the age of 35 years. His practice could best be described as that of a private practice surgeon . He became widely known within the area that he served for his impeccable training and generosity [1]. His dedication to his patients was evidenced by the fact that he reportedly would travel great distances using a rickshaw within the countryside to see his patients. He treated all patients irrespective of class or income [1] .
After 4 years in practice, he married at the age of 39. He and his wife eventually had four children: three sons and a daughter. During the prime of his life, Hashimoto contracted typhoid fever very suddenly from one of his patients. He ultimately succumbed to his illness and died at the age of 52 years on January 9, 1934 [1, 3]. His contribution to medicine had gone unnoticed during his lifetime, and he died without the recognition he deserved for his discovery (Fig. 2) .
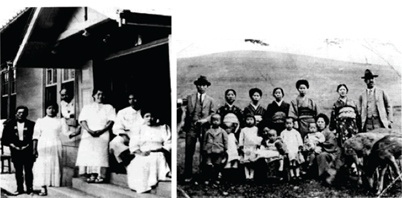
Fig. 2
The picture on the left shows Dr. Hashimoto with other hospital employees posing at the entrance of the town hospital. He is standing third from the left looking out from the window. The picture on the right shows Dr. Hashimoto standing with his family at a picnic. He is the first man on the right. (Pictures is courtesy of The Japan Endocrine Society)
Hakaru Hashimoto’s Discovery
The Initial Description
At the time of his discovery, Hashimoto was finishing his surgical training at the Kyusyu Imperial University . During this time, the primary treatment modality for a thyroid goiter was surgery and thyroidectomies were commonplace. As a result, Hashimoto had the opportunity to study the histology of many resected thyroid specimens. Over the span of 7 years, he came across the thyroid glands of four women who underwent partial thyroidectomy for the indication of goiter. The description of the histology of these glands constituted his most famous piece of work entitled “Zur Kenntniss der lymphomatosen Veranderung der Schilddruse (struma lymphomatosa)” [6]. He decided to publish this article in the German journal Archiv für Klinishe Chirurgie because German was the primary scientific language of the time. Ironically enough, he thought that the information in his article would disseminate most quickly this way .
The article itself was 30 pages long with five sections consisting of the introduction, clinical case presentations, histological description, review of previous reports, and discussion [1, 6]. The bulk of the article involved a very thorough histologic description of the thyroid goiters in the four patients. He explained the extensive lymphocytic infiltration and lymphoid follicles that had not been reported prior. Additionally, he described eosinophilic changes to follicular cells and interstitial fibrosis along with round cell infiltration [1, 6, 7].
The remainder of the article reviewed the reports available at the time differentiating this entity from other known etiologies of thyroid goiter. In meticulous detail, he explained the histological differences of struma lymphomatosa from Riedel’s thyroiditis and the clinical differences of struma lymphomatosa from Graves’ disease [6, 7]. He was confident that this was a new histologic finding within thyroid goiters [6]. Additionally, he made efforts to point out the histological similarities of struma lymphomatosa and Mikulicz’s disease, thought to be Sjögren’s syndrome today. He recognized that histologically this was similar to a modern-day autoimmune disease . He understood that a still unrecognized stimulus was responsible for the histologic changes to these thyroid glands stating, “we can assume that…the lymphocytic elements are stimulated by a certain factor” but that “at present we cannot say anything definite about the cause” [2, 6] .
A Lost Discovery
After publication in 1912, Hashimoto’s work received some recognition in Germany. The next year, in 1913, a German pathologist by the name of Simmonds mentioned Hashimoto’s work, but was unsure whether it was a distinct pathologic entity of the thyroid [8]. Then, in 1914, a German surgeon thought it was a form of chronic thyroiditis [9]. However, during this time, major texts in the British and American literature failed to make mention of Hashimoto or his work when discussing inflammatory disorders of the thyroid gland [2]. Today, many believe the reasons for this relative obscurity were because it was a rare disease compared to endemic goiter; it was harder to access given the need for translation from German, and also because after World War I broke out, the perception of German scientific work on the world stage had changed [2] .
In the 1920s, there continued to be more citations of his discovery limited to German journals. They were also limited to pathology journals [2]. North American and European clinicians continued to fail to recognize his contribution. In 1925, a British pathologist independently described what he thought was a new disease terming it “lymphadenoid goiter.” In his literature review, he failed to identify that it had been described previously [10]. The Western world continued to neglect Hashimoto’s contribution .
Final Recognition
It was not until the 1930s when Allen Graham, a surgeon from the Cleveland Clinic, pointed out that lymphomatous goiter was a distinct histologic type. He confirmed that it was different from other inflammatory conditions of the thyroid, namely Riedel’s thyroiditis [11]. He made a clear connection between Hashimoto’s description and what he had encountered, giving proper credit to him [11, 12]. After these articles were published, surgeons in the USA who had once failed to mention him a decade earlier now included Hashimoto’s work in their textbooks [13]. Hashimoto’s name became attached with the disease process. The British also followed suit, and a surgeon by the name of Cecil Joll admitted his error of not recognizing Hashimoto’s description. He later wrote a paper explicitly describing Hashimoto’s disease and crediting him with its discovery [14] .
By the end of the 1930s, Hashimoto’s thyroiditis had now become a distinct disease within the spectrum of chronic thyroiditis. In fact, the Third International Thyroid Conference in 1938 held in Washington, DC, had an entire session devoted to Hashimoto’s disease. Despite all of these new advancements, Hashimoto’s disease was still considered to be a rare thyroid disorder. Also, the connection between the disease and hypothyroidism still had not been made. Surgical intervention was still the treatment of choice during this time [2] .
The Discovery of an Antibody
Though the scientific community had embraced Hashimoto’s disease as a distinct histopathology of the thyroid gland, physicians still had not recognized its association with hypothyroidism or its etiology. There was speculation that the insulting agent might be a mysterious chemical, but no investigation into why there was lymphocytic infiltration into the thyroid gland had been conducted primarily due to World War II [2]. During the 1940s and early 1950s, this disease remained a strange histology encountered rarely among patients with thyroid goiter [2].
The first inclination that Hashimoto’s disease was an immunologic abnormality was when Fromm and associates detected an elevation of plasma gamma globulin fraction in patients with chronic thyroiditis [15]. This was followed by identification of abnormalities in serum flocculation tests in these patients [16]. Taken together, these preliminary experiments indicated that the disease might be related to a complex autoimmune reaction [17] .
In 1956, the work of two independent groups changed the way physicians understood Hashimoto’s disease. Noel Rose and Ernst Witebsky were immunologists in Buffalo, New York, who showed that when rabbits were immunized with thyroid cells, they would form antibodies to thyroglobulin. When they analyzed the thyroid glands of these animals under the microscope, they found the same lymphocytic infiltration observed by Hashimoto 40 years earlier [18]. They were also able to demonstrate the presence of these autoantibodies in the serum of patients with chronic thyroiditis and published this in a landmark paper [19]. Also in 1956, Ivan Roitt, Deborah Doniach, and colleagues from England were able to demonstrate the presence of antibodies to thyroglobulin in the serum of patients with Hashimoto’s disease [20].
Up until this time, the idea of autoimmunity had existed but was never taken seriously. Now, with these new findings, this concept was a valid theory. This work allowed for a connection to be established between the histology of the thyroid glands that Hashimoto observed and the physiologic underpinnings [2, 3]. Even more impressively, the identification of close to 80 autoimmune diseases affectin g almost every organ of the body began from this work (Fig. 3) .

Fig. 3
Dr. Hashimoto is beloved by the people of his hometown and country of Japan for his contributions. There are numerous symbolic monuments and roads built in his honor. The picture on the right is a monument located in his birthplace of Midai, Nishitsuge, commemorating his life. The picture on the right is a statue of Dr. Hashimoto located in the public hall in the city of Iga. (Pictures is courtesy of The Japan Endocrine Society)
Hashimoto’s Thyroiditis Today
Epidemiology
Early epidemiologic studies investigating the prevalence of this disease in large populations elucidated that Hashimoto’s disease was more common than initially thought with close to 2 % of subjects having overt hypothyroidism, 10–26 % of subjects with evidence of anti-thyroid peroxidase (TPO) antibodies present in their serum, and 7.5–30 % of subjects with elevated serum thyroid-stimulating hormone (TSH) [21–24] . Today, Hashimoto’s disease is considered the most common autoimmune disease, most common endocrine disorder, and the most common cause of hypothyroidism [25]. It exists in populations at a much higher rate than what is diagnosed clinically [17]. The current estimated incidence is approximately 1 case per 1000 persons, and the prevalence is 8 cases per 1000 persons. The prevalence is 46 cases per 1000 when subjects have biochemical evidence of hypothyroidism and thyroid autoantibodies [25].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree