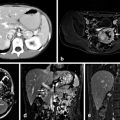
Fig. 1
a and b Necrolytic migratory erythema. (Photos courtesy of Dr. Janice Pasieka and Dr. Steve Urbanski)
It typically originates in the perineum and lower abdomen, but may also present in the perioral area or lower extremities, especially the feet. Involvement of the thorax and upper extremities is rare. It also commonly causes angular cheilitis and glossitis, with “vermilion discoloration” of the tongue [5].
At the time of its initial appearance, the rash appears as a slightly raised, erythematous patch, which spreads within several days. Initially, it resembles an area of scalded skin, with overlying dead epithelium. Often the rash is mistaken for psoriasis, pemphigus, or eczema. Because it causes significant skin fragility, the epidermis is easily rubbed off, leaving raw, weeping surfaces. Especially prone to this, are areas of high friction, such as the perineum and feet. Other affected areas may develop superficial blisters and crusting. It is frequently painful and pruritic .
Typically, as the edge of the lesion spreads, the central areas heal with hyperpigmentation. The migrating edge of the rash tends to have a very well-demarcated appearance that is slightly raised. The process of spreading with central healing takes on a cyclical pattern lasting 7–14 days. There do not appear to be any exacerbating factors [11].
In some instances, the rash follows a more indolent pattern, with a smoldering central necrosis that becomes secondarily infected, usually with Candida or Staphylococcus aureus [12]. Perineal involvement in women causes urethral inflammation leading to urinary tract infection. In intertriginous areas, the rash becomes more lichenified and psoriaform due to the repetitive friction [13] .
The histologic changes of necrolytic migratory erythema are pathognomonic. The findings are confined to the epidermis, where there is necrosis and necrolysis in the most superficial half of the epidermis. Vessicles or bullae form as the dead layer separates from the deeper viable layer. Neither evidence of an immune basis for the rash nor evidence of an ischemic origin has been established. The light microscopic patterns described by Kheir et al. include (1) superficial epidermal vacuolization and necrosis, (2) subcorneal pustule formation, (3) vascular dilatation of the papillary dermis, and (4) psoriaform hyperplasia with confluent parakeratosis [11, 14]. The findings may mimic those of acrodermatitis enteropathica, pellagra, kwashiorkor, fatty acid deficiency, and hypoalbuminemia. On electron microscopy, there is cytoplasmic vacuolization with degeneration of nuclear structures. There is widening of intercellular spaces, and the cells are smaller and have pyknotic nuclei [11].
Several theories as to the cause of the rash include activation of lysosomes in the middle layer of the epidermis, or as a result of abnormal keratinization. In order to successfully make the diagnosis, a biopsy must be taken from the edge of a fresh lesion so as to avoid the secondary changes seen in the areas of infection [15, 16].
Oral ulcers, angular cheilitis, and tongue involvement have been reported with variable frequency. In one of the first series by Mallinson, they were present in almost 90 % of patients, but more recent studies suggest their prevalence in 30 % [7, 8, 9]. Uncommon dermatologic findings include nail dystrophy, onycholysis, and paronychial swelling, as well as blepharitis and alopecia [12, 13].
Diabetes
The majority of patients will have impaired glucose tolerance, which may occur before the rash develops, by months or years. It is often mild, and able to be controlled through diet or oral agents . Diabetic ketoacidosis is not a feature. The typical peripheral and systemic manifestations of diabetes have not been documented in glucagonoma patients . These patients have a degree of hyperinsulinemia, which is thought to counteract the hyperglucagonemia, and they may have a normal glucose tolerance test until very late in the disease [17].
Anemia
Virtually all patients will have a normochromic normocytic anemia. Its severity correlates with the extent of disease, worsening with tumor progression, and the development of hepatic metastases . The degree of anemia also fluctuates with the activity of the rash, often approaching normal levels when the rash is quiescent. The exact cause of the anemia is unclear, and it does not seem to be related to iron deficiency. Bone marrow exams in these patients have not revealed abnormal erythropoiesis. Some have suggested a direct bone marrow suppressive effect of glucagon [8] .
Venous Thrombosis
Weight Loss
Weight loss is a common finding in most patients with glucagonoma, much more so in those with hepatic metastatic disease, as would be expected. It has been reported in 56–91 % of patients [8, 19–22]. It is thought that the catabolic effects of glucagon are responsible for this finding. As with the anemia , weight seems to improve when the rash recedes.
Depression
Uncommon Symptoms
Other symptoms that have been documented in these patients, but are not typical, include intermittent diarrhea. There are no commonly detected electrolyte abnormalities, and urinary 5-hydroxyindoleacetic acid (5-HIAA) levels are normal. Anorexia can be seen as well as abdominal pain. As with other pancreatic neuroendocrine tumors, the islet cells are capable of secreting more than one hormone. Those that have been documented with glucagonomas include insulin, gastrin, 5-HIAA, pancreatic polypeptide, chromogranin, vasoactive intestinal peptide, calcitonin, adrenocorticotropic hormone, and somatostatin [8, 9].
While most glucagonomas are sporadic, there have been rare reports of them occurring as part of the multiple endocrine neoplasia type I (MEN-I) syndrome. [8, 9, 25] These patients generally present at a younger age, and often do not suffer from the classic manifestations of the glucagonoma syndrome, possibly due to earlier detection [11].
There is a subset of patients with glucagonoma who do not develop NME. They present only with severe diabetes and a pancreatic neuroendocrine tumor . Interestingly, these patients also do not develop the other manifestations of the disease.
Diagnosis
The average time from initial presentation until diagnosis is roughly 2 years. Once the diagnosis is suspected, testing should begin with a plasma glucagon level . Circulating glucagon is comprised of several different sized molecules, all sharing the same amino terminus. The larger molecules are felt to represent pro-hormones that are later cleaved. While normal glucagon levels range from 10 to 120 mmol/mL, levels in glucagonoma patients have been reported to range from 500 to 6000 mmol/mL. While certain physiologic conditions such as burns, trauma, and diabetic ketoacidosis can elevate plasma glucagon, they do not approach the levels seen in patients with glucagonoma. Box 1 lists many of the conditions in which hyperglucagonemia can be seen, and thus these need to be ruled out as possible causes. If the level exceeds 1000 pg/mL without an obvious secondary cause, the diagnosis of glucagonoma is highly likely.
Box 1. Causes of hyperglucagonemia [11]
Other islet cell tumors
Cirrhosis
Pancreatic disease
Chronic renal failure
Myocardial infarction
Fasting
Diabetic ketoacidosis
Familial hyperglucagonemia
Celiac disease
Sepsis
Trauma
Cushing’s syndrome
Danazol therapy
There is a significant variability over time. Plasma insulin levels are often elevated, as is fasting blood glucose. An oral glucose tolerance test should be performed, and is expected to be abnormal.
Of historical note, several agents have been shown to stimulate an abnormal rise in plasma glucagon levels . These include oral glucose, intravenous tolbutamide, and intravenous arginine; however, these maneuvers are not part of current clinical practice.
There is a consistent finding of reduced plasma amino acids, which is unique to this disease. It was first reported by Mallinson in 1974 [7]. The reduction is felt to be a direct consequence of the catabolic effect of hyperglucagonemia [26]. The hormone binds to receptors on hepatocytes and adipocytes, and regulates carbohydrate, protein, and fat metabolism. Normally it stimulates gluconeogenesis and glycogenolysis, which ordinarily aids in the maintenance of blood glucose levels during fasting, exercise, and stress [26]. At pathologic levels, glucagon promotes amino acid mobilization from tissues to serve as substrate for gluconeogenesis. Subsequent protein degradation leads to the low amino acid levels seen in patients with glucagonoma syndrome, and this in turn may lead to cellular necrosis in the epidermis. This is one theory on how hyperglucagonemia directly leads to NME [7].
Tumor location and characteristics: Glucagonomas are tumors of pancreatic neuroendocrine origin, specifically alpha-2 islet cells. Primary tumor sizes ranging from 2 to 25 cm have been reported [8]. They are derived from the embryonic dorsal lobe of the pancreas [5]. The majority are located in the neck, body, tail, and superior part of the head of the pancreas.
Once an elevated glucagon level is documented, radiologic studies, beginning with a pancreatic protocol computed tomography (CT) scan are indicated. Today’s thin cut CT scans are highly sensitive, and will also provide images of the liver. Due to its improved sensitivity and noninvasive nature, CT scan has replaced celiac angiography, which was once a common localization technique.
Octreotide scanning has been extensively studied, and was early on the most utilized method of localization. That role has been supplanted by CT, however there is still a place for radioisotope scanning, when searching for suspected disease in CT negative patients, or when the question of miliary type hepatic metastases exists.
On histological analysis, cells are of varying sizes. Cells are pleomorphic, and may be arranged in a glandular trabecular pattern similar to normal islets, or more of a disorganized array with areas resembling rosettes and follicles. There are few mitoses, and the cytoplasm is acidophilic and finely granular [27]. Electron microscopy reveals the numerous dense round secretory granules. Immunofluorescence is confirmatory that an islet cell tumor indeed is glucagon containing. They stain positively for both glucagon and pancreatic polypeptide. Of the islet cell tumors, only glucagonomas are found to contain substantial levels of glucagon, but these levels may not be significantly higher than those found in normal pancreatic tissue. Most are well vascularized.
Thus, definitive pathologic diagnosis depends on the histologic finding of an islet cell tumor which contains secretory granules that stain positively for glucagon. Determination of malignancy, as is the case with most pancreatic neuroendocrine tumors (PNETS), depends on the finding of local tumor invasion or the development of metastases. Upwards of 70 % of glucagonomas display malignant behavior [8, 9, 28]. Those that are classified as benign simply may not have had the time to develop metastases.
Treatment
As with other pancreatic neuroendocrine tumors , small lesions confined to the pancreas can often be enucleated, or removed with a partial pancreatectomy. Since a large percentage of these tumors are malignant, once a diagnosis is made, the goal should be to resect the primary lesion, in a timely fashion. While surgical dogma has traditionally deemed metastatic tumors unresectable, newer studies suggest benefit for many PNET patients, who are candidates for resection of the primary tumor, and resection or debulking of hepatic metastases [29].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree