EXOGENOUS GONADOTROPINS
Part of “CHAPTER 97 – OVULATION INDUCTION“
Initially, injectable gonadotropin used for ovarian stimulation was produced from animal pituitary extracts, but patients rapidly developed antibodies that eventually neutralized their clinical efficacy. Investigators then turned their attention to the
use of postmortem human pituitary gonadotropin (hPG), but lack of adequate amounts of pituitaries and the identification of Creutzfeldt-Jakob disease caused hPG to be banned from clinical use.29,30 Gonadotropins (in a 1:1 ratio of LH to FSH) can be produced from the urine of menopausal women. Although one pituitary gland contains as much FSH as 2 to 5 liters of menopausal urine, the urinary extraction technique has been perfected. In 1962, three pregnancies were reported in women taking hMG after 16 cycles of use.31 Since 1987, urinary-derived gonadotropins have been purified to significantly increase the percentage of FSH (uFSH). As the purification process has improved, the removal of other antigenic contaminants has allowed SC administration.
use of postmortem human pituitary gonadotropin (hPG), but lack of adequate amounts of pituitaries and the identification of Creutzfeldt-Jakob disease caused hPG to be banned from clinical use.29,30 Gonadotropins (in a 1:1 ratio of LH to FSH) can be produced from the urine of menopausal women. Although one pituitary gland contains as much FSH as 2 to 5 liters of menopausal urine, the urinary extraction technique has been perfected. In 1962, three pregnancies were reported in women taking hMG after 16 cycles of use.31 Since 1987, urinary-derived gonadotropins have been purified to significantly increase the percentage of FSH (uFSH). As the purification process has improved, the removal of other antigenic contaminants has allowed SC administration.
The advent of the availability of recombinant FSH (rFSH) products allows FSH receptor stimulation in the absence of LH. Production of rFSH takes place by the transfection of an ovarian cell line from the Chinese hamster with the genomic clone containing the complete human FSH-β coding sequence together with the α subunit minigene. Carbohydrate moieties, which are added after translation, make the product different from endogenous FSH. No differences have been noted between uFSH and rFSH in terms of rates of ovulation and pregnancy achieved.31a
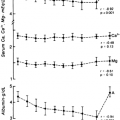
In the early follicular phase of the menstrual cycle, exogenous gonadotropins directly stimulate the ovaries in an attempt to “rescue” from degeneration some of the 20 to 40 follicles with sufficient granulosa-cell FSH receptors. Because of this direct stimulation, follicular development is more pronounced, and estradiol levels are higher; therefore, the risk of multiple births and ovarian hyperstimulation syndrome (OHSS) is increased. When ultrasonographic monitoring demonstrates a lead follicle measuring 16 mm, hCG is given at a dose of 5000 to 20,000 units to mimic the LH surge and produce final follicular maturation and oocyte release. The suggestion has been made that FSH is needed only early in the follicular phase to “rescue” follicles and that a combination of LH and FSH (or LH alone) can be added subsequently to control follicular development more precisely.32
INDICATIONS FOR TREATMENT
If patients with hypothalamic hypogonadism (WHO type I) do not respond to or refuse the use of pulsatile gonadotropin, exogenous gonadotropins can be used to induce ovulation. Because these patients have inadequate LH production, a combination of LH and FSH should be administered. The LH in this preparation allows the production of the androgen precursors needed for adequate estradiol production. When FSH alone is given to these individuals, follicular growth takes place, but inadequate estradiol production probably correlates with poor oocyte and endometrial development.33,34 Ovulation is noted in up to 90% of these patients who use hMG, and the pregnancy rate is 25% to 30% per cycle, with a cumulative pregnancy rate of 70%.35,36 Spontaneous abortions are noted to be as high as 25%, however, perhaps due to poor corpus luteal development. The use of luteal-phase progesterone or hCG administration 1 week after ovulation may be useful in decreasing pregnancy loss.
Anovulatory patients with PCOS (WHO type II) who do not ovulate with the use of clomiphene can be treated with exogenous gonadotropins. These women are very sensitive to gonadotropins, however, and step-up protocols (progressive increase in the number of ampules administered) should be used, with a starting dose of one ampule of hMG or FSH (75 IU). The dose of gonadotropins should be increased until a dominant follicle is seen to emerge from the multiple antral follicles associated with this disease state. A step-down protocol can also be used in which initial dosing with two ampules of gonadotropins is given, and the dose is then reduced to one ampule when two to three follicles begin to progress in development. The IV administration of gonadotropins at a dosage of 6 to 9 IU every 90 minutes has been used, but no advantages in ovarian stimulation have been observed compared with intramuscular delivery.37,38 The use of urinary and rFSH would theoretically be ideal for patients with hyperandrogenic anovulation because of the absence of the androgen stimulation, but clinical studies have not shown FSH to be more beneficial than hMG in this group of patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree