Assessment of driving-related skills (ADReS).
History
The first step of a medical assessment for driving ability is a targeted history. Be alert for acute and chronic medical conditions, medications or symptoms that may impair driving skills when taking the patient’s history (Table 51.3). These “red flags” deserve further evaluation and follow-up.[29]
A general driving history should include questions such as those noted in Tables 51.4 and 51.5, which give the patient and caregiver the opportunity to express concerns that might otherwise be too embarrassing to discuss or which might be forgotten. Some providers may wish to provide these questions or use the Physician’s Guide to Assessing and Counseling Older Drivers questionnaire “Am I a Safe Driver?” as a written handout for self-evaluation prior to initiating an assessment.[29] There are additional questionnaires available that are recommended by expert consensus such as the those available online from the Hartford Guide [52, 53] and the Alzheimer’s Association. However, it should be noted that few of these questionaires, except possibly the Driving Behavior Questionnaire,[54] have been validated in the literature as an effective method of identifying unsafe drivers.
1. Do you now drive a car? 2. How many days did you drive this past week? 3. Have you noticed any change in your driving habits in the past year? Please check all that apply. _____Do not drive at night. _____Do not drive on freeways. _____Do not drive in rain/snow, bad weather. _____Do not drive during rush hour. _____Do not drive as far. _____Only drive when I absolutely must. _____Prefer for others to drive. _____Have cut back because of being too sick/tired. 4. In the past year, have you had any of the following events? Please check all that apply. _____Accidents _____Fender-benders _____Near-misses _____Tickets _____Discussions/warnings 5. Have you ever forgotten where you were going? 6. Do others honk at you or act irritated? 7. Have you ever gotten lost while driving? 8. Have others said they are worried about your driving, criticized you, or refused to ride with you? |
1. Does the patient drive? 2. Have you noticed any unsafe driving? 3. Do you feel uncomfortable riding with the patient? 4. Has the patient gotten lost? 5. Does the patient rely on a co-pilot? 6. Does the patient rely on passengers? 7. Do others worry about the patient’s driving? 8. Does the patient forget where they are going? 9. Do others have to drive defensively? 10. Have others refused to ride with the patient? 11. Has the patient changed their driving habits? 12. In the past year, has the patient had any of the following? Please check all that apply. _____ Accidents _____ Fender-benders _____ Near-misses _____Tickets _____Discussions/warnings |
Targeted physical examination
In addition to the general physical exam maneuvers needed to investigate any positive history items found above, the Physician’s Guide to Assessing and Counseling Older Drivers recommends special items recorded on their Assessment of Driving-Related Skills (ADReS-Figure 51.1) to evaluate vision, motor, and cognitive function.
Far visual acuity should be assessed with the traditional Snellen E chart and visual fields can be checked by confrontation testing. Motor function is gauged through assessments of walking, range of motion, and strength. The rapid-pace walk is based on the time (in seconds) it takes the patient to walk a 10-foot path, turn around, and return with a score of 10 seconds or longer scored as abnormal. Range of motion testing using normative tables and/or a goniometer and manual motor strength testing (using a 0–5 scale) are also assessed.
Cognitive screening is performed in part using the clock-drawing test (CDT), where the patient is verbally instructed to draw the face of a clock and to place the hands at 10 minutes past 11 using a blank sheet of paper and a pencil (see Table 51.1).[55] Memory, visual spatial skills, attention, and executive skills are some of the cognitive domains that are tapped during the clock drawing task. Greater than two errors on the CDT is associated with unsafe driving behaviors based on driving simulation performance.[55] The Trail Making Test part B is also recommended, with a time for performance over 180 seconds considered abnormal and meriting intervention. Patients are asked to connect dots in a path in sequence that alternates between numbers and letters, such as “1-A-2-B.” Poor performance has been prospectively linked to crash risk in two studies of older adults who came in for their license renewals.[43, 45] A recent review also noted that there was a strong association with Trail Making B and road test performance validating the 3-or-3 rule (180 second cut-off or three errors).[56] The Trail Making B form and directions for its use are available for free in the Clinician’s Guide to Assessing and Counseling Older Drivers, 3rd Edition which can be downloaded from the NHTSA website.[29]
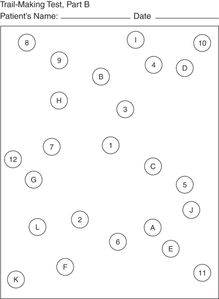
Trail Making Test B.
Interventions
Driving self-assessment and education programs as a prevention strategy
The Driving Decisions Workbook is a self-assessment instrument designed to include medical content, and it has been studied against road test outcomes.[57] Health-care clinicians can recommend driving refresher courses, driving self-assessment, and self-education programs that include the Automobile Association of America’s SeniorDriver program,[58] and the AARP Driver Safety Program.[59] A feature of the AAA program is the Roadwise Review,[60] a CD-ROM or online computer-based home assessment program that includes assessment of leg strength and general mobility, head/neck flexibility, high- and low-contrast visual acuity, working memory, visualization of missing information, visual search, and UFOV. AAA also offers a program to review medications that have the potential to impair driving,[61] in addition to DriveSharp,[16] a CD-ROM or online program to improve visual search and reaction time. ADEPT (Accurate Drivers Education and Professional Training) driver also offers a CD-ROM program to improve traffic safety awareness in older adults.[62] All of these programs could benefit by further validation to determine their efficacy to reduce crash risk.
Referral
Clinicians should try to minimize or compensate for the presence of impairments, so that the patient may continue to drive safely. Additional clinicians who may assist the primary care clinician in assessment of driving skills include ophthalmologists, neurologists, psychiatrists, neuropsychologists, and physical therapists. If the patient’s deficits cannot be medically corrected and do not have further potential for improvement with medical intervention, referral to a driver rehabilitation specialist (DRS) may be necessary. A DRS is often an occupational therapist who undergoes additional training in driver rehabilitation. A DRS should be able to do either driving simulation and/or on-road performance-based testing to specifically determine the patient’s level of driving safety. In addition, the DRS may be able to suggest adaptive equipment (e.g., spinner nob, enlarged side view mirrors, hand controls, left foot accelerator) or training techniques (e.g., enhanced visual search in patients with visual field cuts). A list of certified driver rehabilitation specialists can be obtained from the Association for Driver Rehabilitation Specialists. Patients and health-care providers need to be aware, however, that DRS services are often not covered by health insurance other than state worker compensation and vocational rehabilitation programs.
Also, DRS specialists are often located in urban areas, which may impede referral from rural locations. A local driving school referral or driver education specialist may not be the equivalent of a medical DRS specialist, but may be helpful in the absence of these resources. Health-care clinicians may be called upon to document and verify the presence of impairment to help obtain access and financial support for adaptive equipment, driving rehabilitation, or restricted driving privileges. A list of resources for driving interventions and referrals is listed in Table 51.6.
1. Consider driving (function) in the context of your patient with medical illness(es)
2. For difficult cases, consider referring to a driving rehabilitation specialist
3. For refractory cases, consider referral to your state licensing authority
4. Consider Web resources and/or office handouts
5. Self-help assessment or education
6. Transportation alternatives
7. Office tools
|
Driving cessation
Clinicians should try to limit the adverse consequences for the patient if loss of the ability to drive cannot be prevented, and the patient must stop driving entirely – a circumstance termed driving retirement or cessation. Similarly to work retirement, helping the patient to plan in advance by discussing the eventual need for driving cessation can minimize negative effects and facilitate a smooth transition. The multiple adverse consequences of driving cessation for older adults are well documented and include depression, dependency, caregiver strain, social withdrawal, increased risk of entry into long-term care facilities, and restricted mobility.[63–69]
The health-care clinician’s recommendation for driving retirement should emphasize concern for the patient’s safety and the safety of others as the primary reason for driving retirement. Even so, many patients are understandably upset or angry upon receiving the recommendation, and in the case of cognitive impairment, some may lack the insight necessary to understand the consequences. In addition to allowing adequate time for discussion, it may be helpful to reinforce the recommendation by asking the patient to repeat back to you the reasons for driving retirement, to provide a prescription on which “Do Not Drive” is written, and to help the patient create a plan for alternative transportation. Some patients may also benefit from identifying peer driver behaviors that they consider to be unsafe, and using those examples to set their own threshold for when they would consider themselves unsafe to drive. Identifying a trusted friend or family member whose opinion is honored by the impaired driver may also help to support the recommendation. Keep in mind that a spouse who depends on the patient for transportation may find it difficult to support a recommendation for driving retirement. If the clinician does not have the time or expertise to address this important aspect, then referral to a social worker or gerontological care manager should be considered.
A follow-up letter documenting the recommendation for driving retirement should be sent to the patient, and – if the patient consents – to involved family members. A copy should also be kept in the chart for documentation. Referral to the state department of motor vehicles can be considered in refractory cases.
Clinicians should attempt to see their patients for whom driving is no longer possible soon after driving retirement, both to monitor for compliance with the recommendation to stop driving, and also to check for signs and symptoms of depression and anxiety. Extra care should be taken to assure that travel can be arranged for those who may have difficulty obtaining food, medications, and medical office visits. Finding alternative means of transportation is difficult for older adults, in both rural and metropolitan settings that lack well-developed systems of mass transportation that can accommodate frail older adults. The burden of meeting transportation needs will mostly likely fall on family, friends, and neighbors, some of whom may also suffer from undiagnosed driving impairment. Social agency and volunteer organization referrals for meeting transportation needs are an important part of the patient care plan for driving retirement, often beginning with the area agency on aging.[30] For patients who lack capacity and insight, it is essential for the appointed guardian or caregiver to help the patient comply with the recommendation to stop driving. Many strategies have been employed from placing reminder signage on doors to removing the vehicle altogether.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




