Introduction
The positive association between visual impairment and mortality has been well documented in several longitudinal eye studies1–7 although the mechanisms for this association are not as well understood.8, 9 Because visual impairment can predict mortality, a better understanding of the common types of visual impairment and their treatments and risk factors should assist practitioners in providing life prolonging medical care.
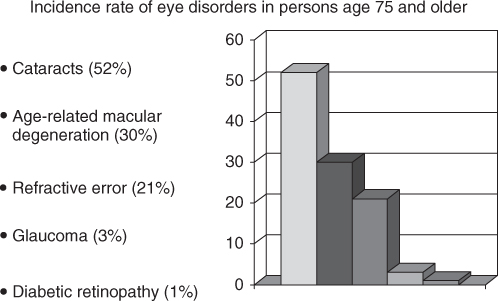
Five major disorders cause the greatest visual disability: cataracts, diabetic retinopathy, refractive error, macular degeneration and glaucoma. Increasing age is a major risk factor for all five of these disorders. The overall prevalence of refractive error resulting from these five causes of visual impairment is remarkably consistent around the world. Figure 85.1 shows average values for the prevalence of these disorders in people aged 75 and over in the American population gleaned from multiple sources of reviewed literature10–13 (http://one.aao.org/CE/PracticeGuidelines/PPP.aspx). These numbers were determined from epidemiological studies done in the 1980s. It is reasonable to expect that these percentages may have decreased somewhat with improved treatment options, especially for diabetes mellitus. However, with the increase in persons now over age 75, the number of persons suffering from these visual impairments is still rising.
Figure 85.1 Over 50% of Americans aged 75 and older will suffer from visual impairment due to cataracts, 30% will lose central vision from age-related macular degeneration, 21% will have uncorrected refractive errors, 3% will report visual field loss due to optic nerve damage from glaucoma, and 1% will suffer vision loss due to diabetic retinopathy
Visual impairment is often described as a person’s most feared disability, and with good reason. In older persons, visual impairment is particularly devastating because it has been associated with dramatic reduction in QOL.14 As vision declines, people are forced to curtail driving. Those who can no longer see clearly report having a reduction in mobility, and having difficulty walking and leaving their homes to participate in social and religious activities. They report a loss of ability to perform activities of daily living (ADL) such as dressing, shopping and getting in and out of bed safely. Poor vision interferes with the ability to take medications properly. It is also a leading risk factor for falls and fractures which, in turn, are risk factors for placement in both non-institutional and institutional extended care and for loss of independence. In addition, other conditions appear to be strongly comorbid with low vision. These include dementia, depression and delirium and other sensory losses, such as hearing and balance deficits. Thus, vision impairment has profound effects on the older person and it is incumbent upon healthcare providers to identify people at risk for leading causes of visual impairment, and to initiate treatments in a timely manner.
Definitions, Treatments, and Risk Factors
Refractive Errors
Refractive error can be described as visual acuity with best lens prescription worse than 20/40. It is the most frequent eye problem and is usually corrected with prescription eyewear. The percentage of people whose visual acuity cannot be improved beyond 20/40 increases dramatically with age: 0.8% for those between 43 and 54 years old, 0.9% for those between 55 and 64, 5% for those between 65 and 74, and 21.1% for those 75 and older. This increasing degree of uncorrected refractive error is due to a number of variables. For example, there is normally an increase in the against-the-rule astigmatism with age and it is often exacerbated during surgery that breaches the conjunctiva such as cataract and glaucoma15 surgeries. The long-term effects of refractive surgeries such as laser-assisted in situ keratomileusis (LASIK) and epi-LASEK that many people are now undergoing for the correction of myopia, hyperopia and presbyopia is being studied.16 Differences in sample sizes, age and sex distributions, length of follow-up and preoperative spherical equivalents have made it difficult to compare results. More follow-up studies are still needed to distinguish the effect of ethnicity on postoperative visual outcomes and standards for reporting surgical outcomes must be set in order to be able to compare efficacy, stability and safety of the different procedures.
The most common refractive error is myopia, or nearsightedness. With this disorder a person has difficulty seeing distant objects clearly. Severe myopia carries with it a large risk of blindness because it is associated with ocular comorbidities such as retinal detachment, macular choroidal degeneration, premature cataract and glaucoma.17 Genetic studies of myopia have identified several loci that are linked to myopia and a key environmental inverse determinant of myopia is total time spent outdoors.18 Clearly there is great value in the next decade to performing research on assessing the role of early-age near work versus outdoor activity on genotypes for myopia. This research would provide valuable insight on how to reduce this worldwide epidemic of myopia and its associated high levels of blindness.
There is also a normal hyperopic shift in older adults that may be altered by cataract surgery.19 Contrast sensitivity decreases with age, in part due to the increased prevalence of dry eye with age, and in part due to the smaller pupil size found in the older person. Dark adaptation also decreases with age and with diseases such as diabetic retinopathy and cancer. Finally, cataracts, yellow lenses and aberrations of the cornea, all of which increase with age, produce glare caused by excess light scattered within the eye. This glare can be debilitating. It can cause difficulty with driving and other tasks conducted in bright light. It can also cause headaches. As people who have been faithful contact lens wearers for decades enter their 70s and 80s, it will be interesting to determine whether the rate of corneal aberrations rises.
There are many risk factors for refractive errors in the older person. Many of the medical and social risk factors are listed in Tables 85.1 and 85.2. Most of these risk factors can be handled with annual dilated fundus eye exams and instructions to seek medical treatment at the first sign of worsening vision. For many persons, that translates into instructions to seek vision care when they notice that they are having more difficulty with their every-day activities due to vision changes.
Table 85.1 Medical risk factors for refractive errors.
|
Table 85.2 Social risk factors for refractive errors.
|
Age-Related Macular Degeneration
Age-related macular degeneration (AMD) is a disorder of the macula characterized by the presence of drusen, hypo- or hyper-pigmentation of the retinal pigment epithelium (RPE), local atrophy of the RPE and choriocapillaris, neovascularization of the macula, and a reduction or loss of central vision.12 AMD is the leading cause of severe, irreversible vision impairment in developed countries. Ninety percent of the AMD cases are of the non-exudative (dry or atrophic) type. Ten percent are of the exudative (or wet) type. Non-exudative AMD is characterized by the presence of drusen and loss of RPE and photoreceptors. Sight in the central visual field is lost gradually. Exudative AMD is characterized by a much more rapid loss of central vision due to neovascularization of the choroid and its accompanying haemorrhages that lead to retinal and RPE detachments and scarring. Although non-exudative AMD is more prevalent, most of the people with severe vision loss have exudative AMD.
The National Eye Institute (2010) lists the risk factors for developing AMD as age over 60, obesity, Caucasian race, smoking, family history, being female20 (although estrogen has not been implicated in increased AMD risk)21 and exposure to sunlight.22 Currently, there are no pharmaceutical treatments for AMD. However, patients with dry AMD should receive regular dilated fundus eye exams and should be encouraged to increase their consumption of antioxidants. They should be educated about how to use an Amsler grid to screen for the progression of dry AMD into wet AMD and encouraged to seek medical attention at the first sign of new symptoms. Dietary consumption of fresh fruits and vegetables is encouraged because they contain antioxidants such as Vitamin C, Vitamin E, carotenoids, selenium and zinc, which are thought to neutralize damage caused by free radicals. Those who have unilateral AMD should be encouraged to take supplements in order to reduce their chances of developing AMD in the other eye. Results from the National Eye Institute Age-related Eye Disease Study (AREDS) showed that supplements containing high levels of antioxidants and zinc significantly reduce the risk of advanced AMD and its associated vision loss.23 (As an aside, it should be noted that the same nutrients had no significant effect on the development or progression of cataract.) If the patient requests it, advice on developing a diet to help maintain a healthy weight and increase consumption of antioxidants should be provided in written form.
Routine examinations for patients with wet AMD should include optical coherence tomography (OCT) in order to monitor changes in retinal thickness due to both the presence of drusen in the retinal pigment epithelium and blood caused by retinal bleeding. OCT allows the structural integrity of the retina to be followed during therapy. In an effort to preserve residual vision, retinal bleeding is currently controlled by laser photocoagulation but this is not a curative therapy.
There are several ongoing research studies on surgical treatments for wet AMD that is no longer responsive to diet and supplements. Wet, or neovascular, AMD is a complex disease. Several studies have looked at the role of angiogenic agents that probably contribute to choroidal neovascularization.24–27 To date, no clear treatment guidelines have been developed for the anti-angiogenic therapies.
Although there are several environmental risk factors for AMD, the future of some treatments may indeed be rooted in the genome. To that end, researchers are looking at genotypic variation for AMD. Although AMD is a complex disease, about 40% of the genetic variance can be explained by variations in five common single-nucleotide polymorphisms (SNPs).28 Other SNPs have been associated with risks for common treatments such as photodynamic therapy or bevacizumab treatment.29 Recent advances in these inexpensive genetic technologies may allow medicine to produce personalized diagnosis and treatment plans for AMD.30
Finally, persons with advanced AMD may be classified as legally blind and often require assistance with ADLs even if the AMD is monocular because contrast sensitivity is affected, thereby reducing visual acuity in the unaffected eye. They are also at significant risk for depression. Vision can often be enhanced by the use of low vision aids such as magnifiers and bright lights. Motivated patients can be taught to read with the peripheral retina. Because functional status and QOL are related, every effort should be made to encourage patients to seek rehabilitation.
Risk factors for, and other factors associated with, AMD are listed in Tables 85.3 and 85.4.
Table 85.3 Confirmed risk factors for AMD.
|
Table 85.4 Factors associated with AMD.
|
Diabetic Retinopathy
Diabetic retinopathy (DR) is a leading cause of blindness in the industrialized world in people between the ages of 25 and 74,31 and the fourth leading cause of blindness in people of all ages in developing countries.32 Annually, between 12 000 and 24 000 diabetic patients in the United States become legally blind as a result of complications of diabetic retinopathy.33 Every diabetic patient is at risk for several changes to vision that occur as a result of uncontrolled systemic diabetes mellitus (DM) of long duration, including numerous ocular and periocular changes that characterize diabetic retinopathy. DR is a disorder of the retinal vasculature. Resulting changes are characterized by waxy exudates, micro-aneurysms, punctate haemorrhages and, less frequently, neovascularization, all of which lead to a decrease in visual acuity and, perhaps, to blindness. Indeed, the elderly diabetic patient is 1.5 times more likely to develop vision loss and blindness than is an age-matched non-diabetic person.34
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








