CHAPTER 16 Diseases by Race/Ethnicity
Summary Points
Introduction
Any discussion of diseases by race/ethnicity must be prefaced by a discussion of the present debate over use of these terms. The terms ‘race’ and ‘ethnicity’ do not have universally accepted definitions, which alludes to the complexity of the connotations. Francis Collins, director of the National Human Genome Research Institute, stated in a recent article:1
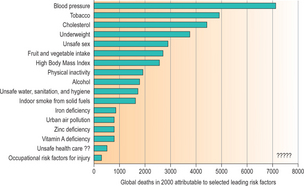
It will become apparent throughout the course of this chapter that racial and ethnic differences in diseases are influenced as much by socioeconomic and environmental factors as they are by cultural and genetic factors. Leading causes of death have varying evidence for genetic influence (Fig. 16.1). This chapter will focus on evidence as it relates to cardiovascular diseases, diabetes, obesity, cancer, and hemoglobinopathies.
Cardiovascular Disease
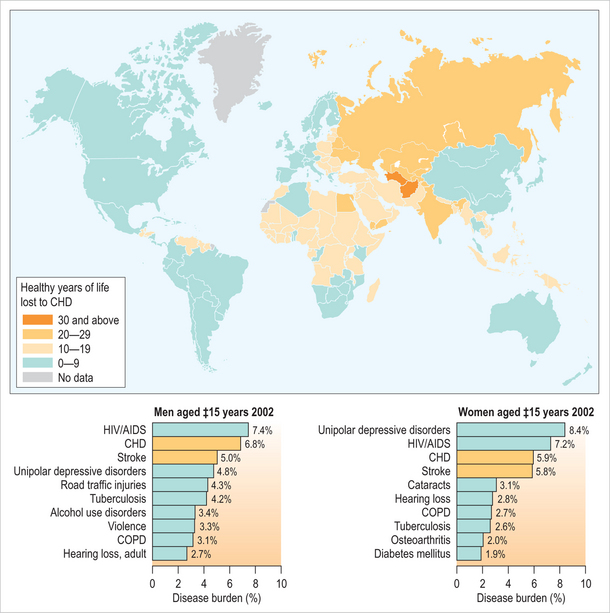
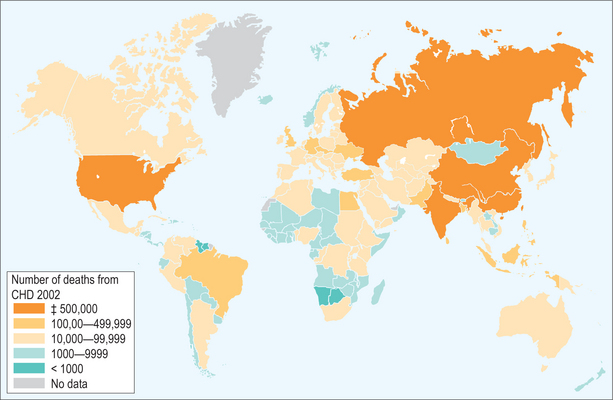
Cardiovascular disease is the most common cause of death in the Western world and is emerging as one of the most common causes of death in the developing world (Figs 16.2–16.5). Migrants to developed countries have variable risks of morbidity and mortality from heart disease that may be associated with their race or ethnic background, as well as multiple environmental and personal risk factors. Cardiovascular disease is known to have a multifactorial etiology including genetic determinants, environmental exposures, and lifestyle factors. Urbanization in Africa and rapid economic development in Asia have resulted in an increased burden of chronic vascular diseases in developing countries and exposed important ethnic differences regarding causation. Studies in the United Kingdom have compared variations in cardiovascular risk for people of South Asian and African descent.2,3 South Asians have been observed to have an elevated risk of ischemic heart disease when compared to Europeans and African-Caribbeans. More recent investigations have demonstrated that these differences in risk are primarily related to metabolic abnormalities that include insulin resistance, hyperglycemia, and dyslipidemia which have been shown to be more common in South Asians.4 A genetic basis for these differences has been postulated but not yet identified.
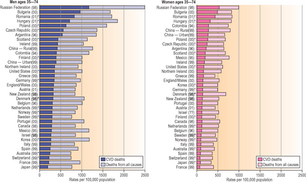
Fig. 16.2 Death rates for total cardiovascular disease, coronary heart disease, and stroke, and total deaths in selected countries. http://www.ehponline.org/members/2004/112–15/cvdratesbg.jpg
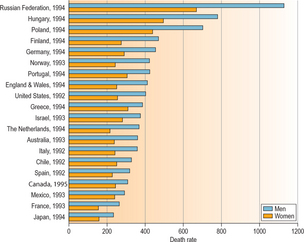
Fig. 16.3 Age standardized rates of death from cardiovascular disease in several countries in the mid-1990s.
(Source: 1995 World health statistics annual, World Health Organization. In: Disease and stroke in Canada. Ottawa: Heart and Stroke Foundation of Canada; 1997:8.) http://epe.lac-bac.gc.ca/100/201/300cdn_medical_association/cmaj/vol-157/issue-12/images/1659fig1.gif
In the early part of the twentieth century, African-Americans in the United States had a similar risk of ischemic heart disease as had recently been described in African-Caribbeans in the UK. However, with acculturation, these discrepancies have disappeared, with African-Americans now demonstrating a higher incidence of ischemic heart disease than US whites.5 These recent findings imply that in persons originally of African descent, socioeconomic and environmental factors may be more powerful determinants of ischemic heart disease than genetic causes. In contrast to the lower prevalence of coronary heart disease, Africans have consistently been shown to have increased rates of hypertension and stroke even prior to urbanization.6 In addition to the increased risks of hypertension, migration to urban areas in Africa has also been shown to lead to a higher prevalence of atherosclerosis and coronary artery disease, presumably heavily influenced by change in lifestyle and environmental modifications.7 This evidence would suggest that although genetic factors play an important role, migration and the corresponding change in environmental and social factors greatly influence cardiovascular disease rates in African immigrants and refugees.
The burden of cardiovascular disease in Hispanics who have immigrated to the US is thought to be similar to that of non-Hispanic whites. Studies in the early 1990s suggested that Hispanics often have higher traditional risk factors but lower rates of ischemic heart disease, implying a component of genetic protection.8 More recently, however, the risk of cardiovascular disease in Hispanics living in the US has been shown to parallel that of non-Hispanic whites.9,10
In Eastern Europe, the prevalence of cardiovascular disease has increased rapidly since the collapse of the Soviet Union in 1991. Mortality from cardiovascular disease in Russia has been shown to be significantly higher than that of Western Europe and the US and resulted in an estimated 800 deaths per 100 000 in 2000.11 Interestingly, the sharp rise in cardiovascular mortality in Russia appears to be only partially related to classic risk factors for cardiovascular disease such as cigarette smoking, blood pressure and serum cholesterol. It has also been driven by excessive alcohol consumption which is pervasive within certain segments of this population.12,13
Metabolic Syndrome, Obesity, and Diabetes
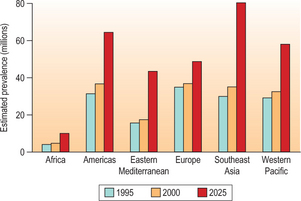
The prevalence of obesity, diabetes, and the metabolic syndrome is increasing globally and has reached epidemic proportions in many areas (Tables 16.1, 16.2; Fig. 16.6). The incidence of obesity in all age and racial groups continues to rise worldwide (Fig. 16.7). In children, the risk of being overweight and obese in affluent countries is greater for those from lower-income families, whereas the opposite occurs in low-income countries.14 In the US, ethnic minority children are disproportionately overweight and are thus at risk of obesity in adulthood. Ironically, although overweight and obese, these children are at risk of nutritional deficiencies due to the poor nutritional value of the calorie-rich foods frequently available to low-income populations in developed countries. In both males and females in the US, the prevalence of obesity is higher in African-Americans and Mexican-Americans compared with Caucasians. Duration of residence in the US influences rates of obesity. Goel et al. found that immigrants who had resided in the US for less than 1 year had a rate of obesity of approximately 8% that rose to a rate of 19%, approaching the rate of 22% for US-born individuals, after 15 years of residence. They were also able to show that this change in obesity rates was associated with assimilation of dietary and physical activity patterns.15 Furthermore, racial differences in the distribution of adiposity have been observed. Caucasians generally have excess fat in the upper body regions including the abdominal viscera compared to African-Americans and Mexicans. Asian Indians also appear to have a greater amount of intra-abdominal fat as well as an overall higher percentage of body fat relative to body mass index, placing them at increased risk for insulin resistance and dyslipidemia, which is commonly referred to as the metabolic syndrome.4,16
Table 16.1 List of countries with the highest numbers of estimated cases of diabetes for 2000 and predicted for 2030
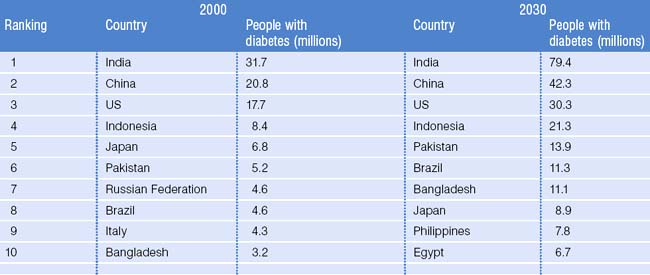
Table 16.2 Estimated numbers of people with diabetes by region for 2000 and 2030 and summary of population changes
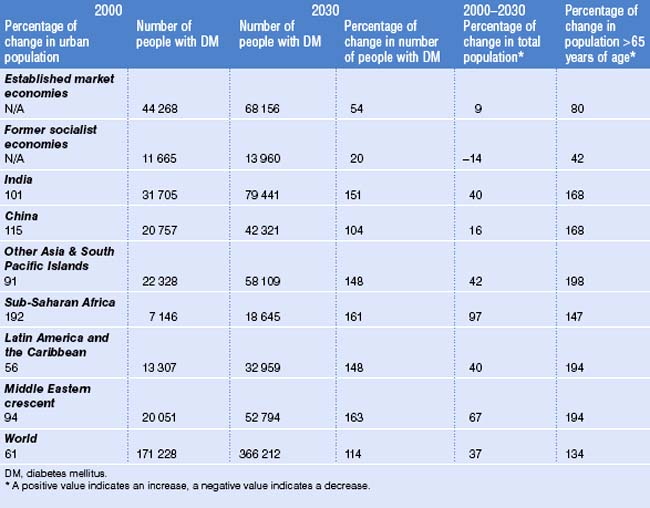

Fig. 16.7 Proportion of obesity in selected countries. http://www.foodmuseum.com/images/obesworldobesityflags.jpg
Metabolic syndrome is associated with undesirable health outcomes including diabetes and coronary heart disease. The syndrome is age dependent, with the prevalence rising substantially in individuals over 60 years of age. Prevalence has also been demonstrated to vary by race/ethnicity within the US, with Mexican-American women having the highest prevalence followed by Mexican-American men and finally African-American women.17,18 Studies that have examined insulin resistance and obesity in migrant populations within the UK have found Asian Indians to have a significantly higher prevalence of the metabolic syndrome compared with individuals from other ethnic backgrounds. Recent investigations exploring the role of underlying genetic or early-life adverse events in the pathogenesis of the metabolic syndrome have revealed that the proteins adiponectin and resistin may contribute to insulin resistance; however, the mechanism is unclear.16 As with cardiovascular disease, lifestyle and environmental factors are important determinants in the development of the metabolic syndrome.
One undesirable consequence of the metabolic syndrome is the development of type 2 diabetes. The global increase of type 2 diabetes was noted in adults many years ago and recently has been shown to be occurring among children and adolescents as well (Figs 16.3, 16.4).19 In the US, adolescent and adult immigrants have been found to be disproportionately affected by type 2 diabetes. Specifically, African-Americans, Hispanic-Americans, Asian-Americans and Pacific Islanders are at increased risk.20 The etiology of the observed ethnic disparity in the prevalence and incidence of type 2 diabetes is thought to be multifactorial, involving both genetic and environmental factors. Studies have demonstrated higher degrees of insulin resistance among West African descendants, including native Ghanaians, African-Americans and Hispanics compared to whites.21,22 Interestingly, a study with a cohort of approximately 3000 individuals with impaired glucose tolerance found that the risk of progression to diabetes did not vary across race or ethnic groups.23 This finding implies that genetic or ethnic components predisposing to diabetes must wield the greatest impact during the transition from normal metabolism to impaired glucose tolerance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree