CHAPTER 15 Diseases by Country of Origin
Introduction
Infectious disease risks vary by geographic region and can change over time. Because many infections can persist in an individual for years and sometimes for a lifetime, the geographic regions of previous residence, and, to a lesser extent, travel, are relevant in the evaluation of immigrants, whether or not they have symptoms. Because many immigrants have families and relatives in their country of origin, they and their children may visit, placing them at risk for infections that may be absent or rare in the United States. Previous exposures, infections, and healthcare may place them at lower or higher risk for specific infections. For example, most people who grew up in developing countries are immune to hepatitis A because of infection in childhood (which may have been mild or inapparent and unrecognized), though as sanitation facilities improve in many countries, levels of immunity to hepatitis A are decreasing.1,2 On the other hand, people who reside in tropical and subtropical areas are much less likely to be immune to varicella (chickenpox) than are residents of temperate areas, where most people (in the pre-vaccine era) became infected in childhood. Varicella infections occur in adult immigrants and are more likely to be severe than cases acquired in childhood.3 In the US between 1985 and 1994 about 20% of all adult varicella deaths were in foreign-born adults.4 Immigrants may be susceptible to other infections because vaccinations were not given or were ineffective, for example, because of poor vaccine quality, inadequate dose or number of doses, or poor immune response because of age, nutritional status, coincidental infections, or other factors. Older immigrants who have been in the US for a long time may lack immunity to tetanus because they have never received a primary series of tetanus toxoid (and a booster dose after an injury will not provide adequate protection).5,6
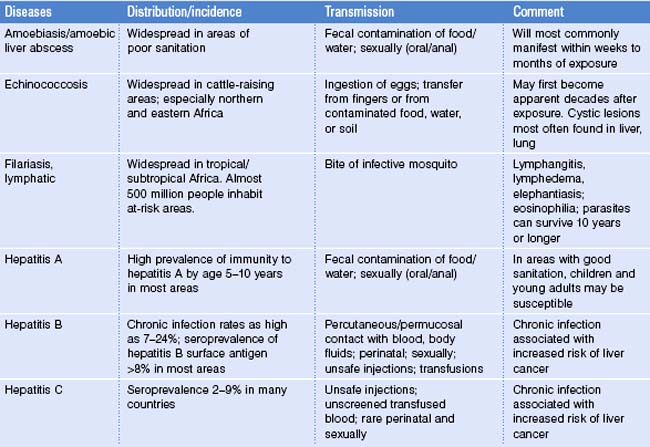
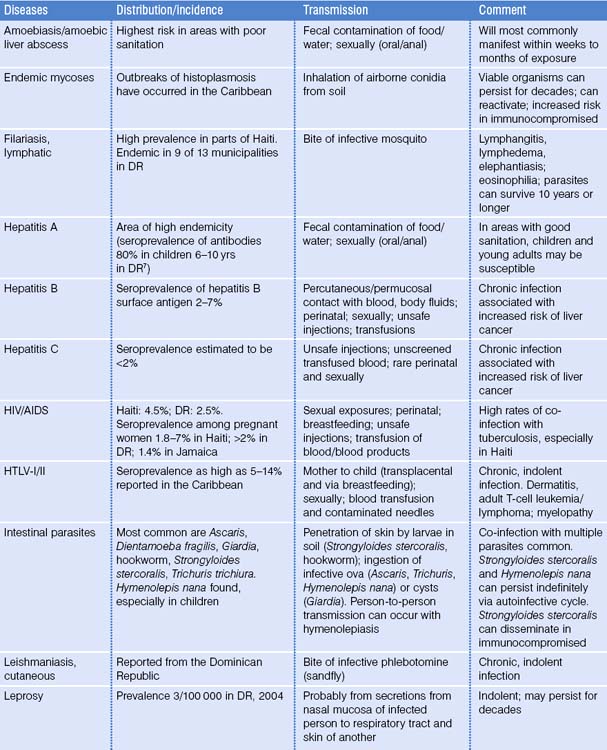
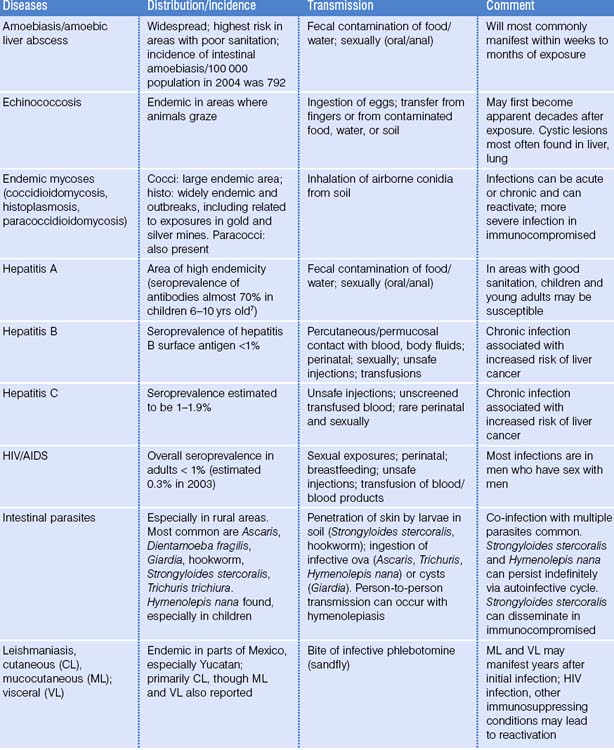
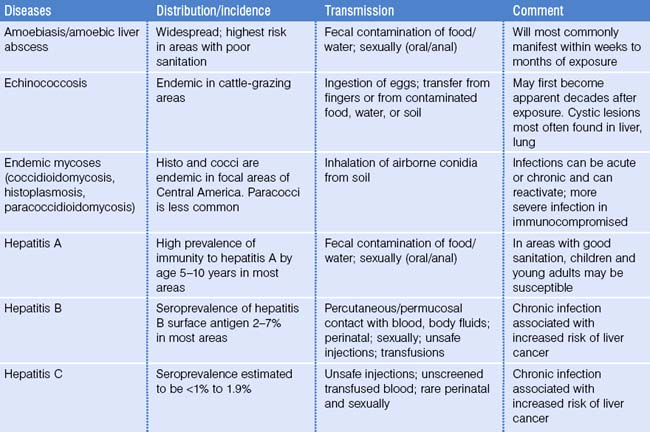
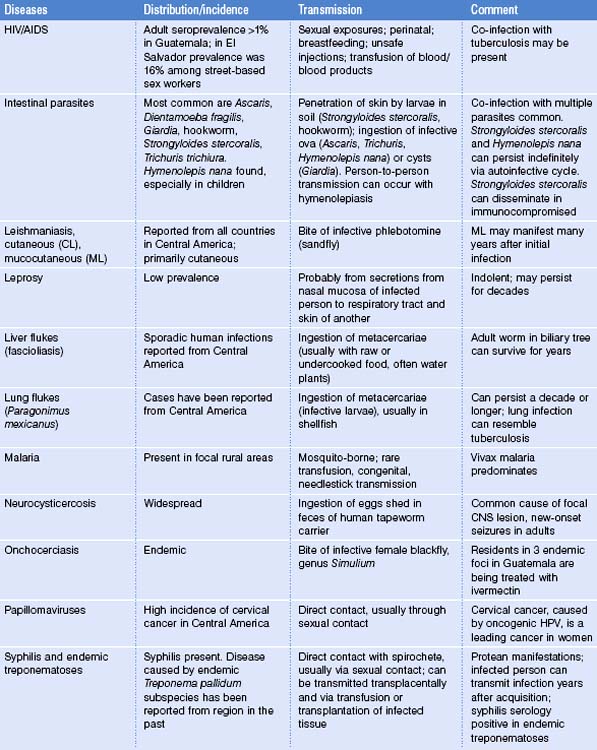
Clinicians caring for immigrants and their families need to know what persisting infections or sequelae of past infections in immigrants may be clinically or epidemiologically relevant today and in the future.7–9 This chapter provides a series of tables that describe infectious diseases by geographic region of the world.10,11 The geographic areas chosen are those that have been the origin of the largest number of immigrants to the United States, especially in recent years.12–16 Specific countries are listed within some regions. Although space does not permit listing of all countries of the world, other countries in a given region may share similarities in infectious disease risk. The majority of immigrants to the US before 1950 came from Europe and Canada, areas where many infectious disease risks are similar to those in the US. Thus, infectious disease risks in those areas are not listed separately.
The infections chosen for the tables are those that may be associated with morbidity weeks to decades after a person has left a country of origin.9 Where data are available and relevant, some description of the distribution and incidence is provided. The estimated incidence of tuberculosis is given by country and, when available, the percentage of cases with multidrug resistance is included. The incidence for many infections has decreased over time in many regions (HIV is a notable exception). Current incidence of infection may not accurately reflect the risk of acquiring infection when the immigrant lived in a country 10 or 20 years earlier. This is especially true for chronic infections, such as syphilis, tuberculosis, onchocerciasis, lymphatic filariasis, leprosy, and schistosomiasis. For example, global prevalence of leprosy has fallen by almost 90% in the last 20 years. The epidemiological situation in earlier years may be more relevant than the current prevalence or current rates of transmission for persons who resided in another country many years earlier.
The tables also detail the means of transmission, in part to help the clinician assess risk factors that might have led to infection and also to review whether infection might pose any risk to family and close contacts, including sexual partners, and whether any specific precautions might be needed.17–19 Some of the infections can be transmitted from mother to child (including via breastfeeding) and by blood transfusion or organ or tissue transplantation. Additional comments provide other points that may be useful clinically (e.g. clinical findings, drug resistance patterns, time of appearance, and others).
Many of the infections listed can persist for prolonged periods, some for the lifetime of the host. A broad framework that can be used in thinking about consequences of past infections includes: active infection (primary, persistent, or reactivation), latent infection, immunity to infection, and other sequelae of infection.20 In contrast to most viral infections, in which infection is followed by immunity that protects against subsequent infections with that pathogen, infection with one dengue serotype can increase the probability that infection with a different serotype can be associated with severe or complicated infection. This is relevant for immigrants from dengue-endemic areas who visit areas with dengue outbreaks. Patients with hepatitis B may be chronic carriers with or without symptoms; patients infected with tuberculosis may have latent infection, which can reactivate. Infection with HIV is persistent, typically with progression, if no interventions are applied. Other consequences of infection include malignancies related to infections (e.g. hepatitis B and C and liver cancer; papillomaviruses and cervical cancer).21,22 Scarring and mechanical effects related to active or past infection can obstruct a ureter (e.g. tuberculosis), biliary tree (e.g. fascioliasis or echinococcal cyst), or be associated with liver fibrosis and portal hypertension (e.g. schistosomiasis). Allergic or hypersensitivity reactions may follow the release of antigen-rich material, e.g. leaking echinococcal cyst. Focal lesions and masses can lead to seizures (e.g. neurocysticercosis) and focal neurologic deficits. In many instances, the infection may have been clinically silent for years and the patient may have no knowledge of it. The clinical presentation may not lead the clinician on initial evaluation to think that the process was the result of infectious disease, and certainly not one acquired long ago. Many of these late consequences of infection are not associated with fever.
Immigrants bring with them microbiologic and parasitic baggage related to past residences. Return trips to visit friends and family put them at risk for acquiring new infections that may be unfamiliar to many clinicians in the US. Those whose purpose of travel is visiting friends and relatives (VFRs) are at increased risk for a number of infections, including malaria, enteric fever (typhoid and paratyphoid), and hepatitis A.23,24 Immigrants who have previously lived in malaria-endemic areas and are familiar with the infection may not realize that the immunity from previous infections that gave partial protection against severe malaria wanes over time. Many fail to take chemoprophylaxis and develop malaria.25 In Europe during the period 1991–2001, non-nationals accounted for 43% of malaria cases registered at major centers. Children who visit high tuberculosis incidence countries are more likely to be tuberculin positive. A study in California found that US-born children who traveled to or had a visitor from a country with a high prevalence of tuberculosis were, respectively, 4.7 and 2.4 times more likely to have a positive tuberculin skin test than control children.18
During residence in the United States, immigrant populations and their families may have exposures related to visits from relatives as well as from travel to their country of origin. Tuberculosis is an infection that can be transmitted by household visitors, as noted above. Human infections due to Mycobacterium bovis have recently increased in the US after having been almost eliminated by control of infection in dairy herds and routine pasteurization of milk. At least 35 cases (and at least one death) were identified in New York City from 2001 to 2004.26 M. bovis accounted for 34% of the culture-confirmed cases of TB in children aged less than 15 years in San Diego, California, during 1980–1997. About 90% of these children were born in the US to Hispanic families. Fresh cheese brought from Mexico was thought to be the source of many of these infections. It has been estimated that about 20% of cow’s milk in Mexico that is used to make fresh cheeses is not pasteurized. A study published in 2000 found that 17% of cows sampled at a meat processing plant in Mexico were infected with M. bovis. M. bovis is characterized by resistance to pyrazinamide, a marker that may help to distinguish it from Mycobacterium tuberculosis.
Brucellosis, another infection associated with consumption of contaminated milk products,27 has been diagnosed after travel to endemic areas, including Mexico, but also in immigrants in the US after consumption of unpasteurized goat milk or cheese brought from Mexico.
With some parasitic infections, such as filariasis and schistosomiasis, individuals repeatedly exposed or infected at a young age may manifest clinical findings that differ from those in persons from nonendemic areas who are first exposed at an older age.28,29
The number of legal immigrants reflects only a part of the pool of foreign-born in the US. For example, although the estimated number of legal immigrants from Mexico entering the US per year was 175 000 (2002 statistics), the number of undocumented migrants was 961 600 and temporary visitors from Mexico was 633 078.30
Limitations
The tables (Table 15.1 to Table 15.11) are based on the best information available, including materials from the World Health Organization, Pan American Health Organization, (PAHO), Centers for Disease Control and Prevention (CDC), and other regional or country-based institutions.31,32 For many infections, data are absent or incomplete and reflect the best estimate of infection based on published reports of cases, outbreaks, seroepidemiological surveys, or other studies. In some instances, immigrants come predominately or exclusively from one part of a country, whereas the only incidence data are from the country as a whole. Many of the infections are not reportable, so information by geographic region is incomplete, outdated, and may be incorrect.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree