DIFFERENTIAL DIAGNOSIS OF HYPERTHYROIDISM
Part of “CHAPTER 42 – HYPERTHYROIDISM“
GRAVES DISEASE
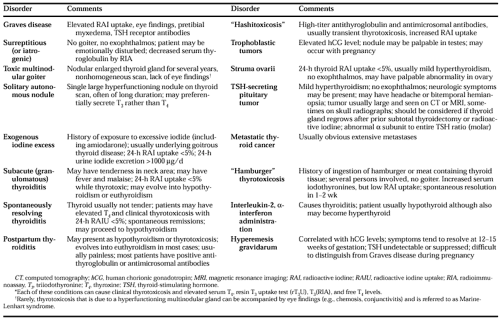
Graves disease occurs most frequently in young women (˜5:1 female to male ratio) but is not uncommon in any age group or in any geographic population.1,2 and 3,5 No single clinical sign or symptom differentiates Graves disease from other causes of thyrotoxicosis, although the presence of ophthalmopathy, a diffusely enlarged and firm thyroid gland, and pretibial myxedema or acropachy strongly suggests this illness. The cooccurrence of another autoimmune disease in the patient (e.g., myasthenia gravis) or a family history of Hashimoto or Graves disease or of any other autoimmune disease is a frequent accompaniment of this condition. Graves disease is found more frequently in patients with HLA-DR3 antigens. The laboratory diagnosis is supported by the presence of stimulatory TSH receptor antibodies in a thyrotoxic patient.1,2 and 3,43 However, the measurement of TSH receptor antibodies is not indicated in most patients, as usually the diagnosis can be made on the basis of the previously listed clinical characteristics.
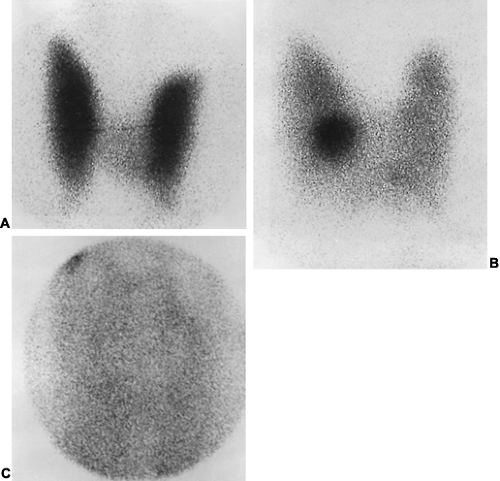
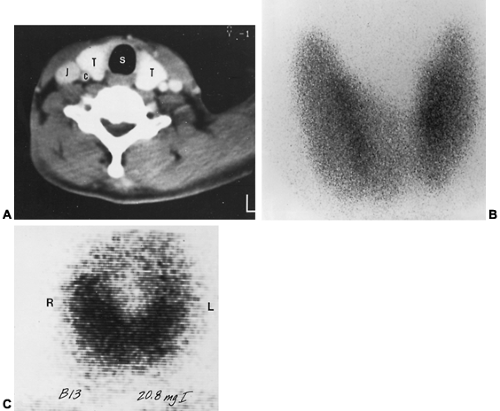
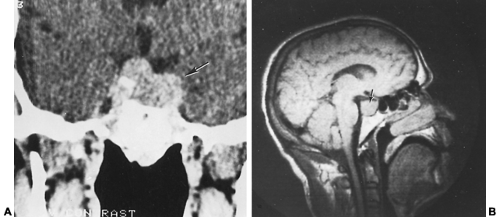
Although rarely indicated, the thyroid gland may be imaged in such patients by a radioisotopic thyroid scan, CT, magnetic resonance imaging (MRI), or fluorescent iodide scan (Fig. 42-5, Fig. 42-6 and Fig. 42-7) (see Chap. 34, Chap. 35 and Chap. 39). The differential diagnosis of hyperthyroidism includes more than a dozen other conditions (Table 42-3).
SURREPTITIOUS INGESTION OF THYROXINE OR TRIIODOTHYRONINE
Hyperthyroidism that is due to the administration of thyroid hormones is not uncommon, as exogenous thyroid hormone is easily obtained. This medication is often taken by persons who wish to lose weight. The surreptitious ingestion of T4 or T3 (thyrotoxicosis factitia) can be inferred from the measurement of inappropriately low levels of serum thyroglobulin. Because thyroglobulin is normally secreted by the thyroid gland in concert with T4 and T3, its levels should be elevated in cases of thyroidal hyperfunction, whereas its levels are suppressed with ingestion of exogenous thyroid hormones.44 In addition, the
thyroid radioiodine uptake is depressed. If the patient is taking T4, serum values of this hormone are typically increased more than those of T3. If the patient is taking T3, the serum T3 level may be preferentially increased, with the T4 level being decreased. The extent of serum T3 changes in these patients depends on the dose ingested and how long after ingestion the blood is obtained. Thyroid extract ingestion may be associated with elevations of both T4 and/or T3, depending on the preparation used and the time interval since ingestion.
thyroid radioiodine uptake is depressed. If the patient is taking T4, serum values of this hormone are typically increased more than those of T3. If the patient is taking T3, the serum T3 level may be preferentially increased, with the T4 level being decreased. The extent of serum T3 changes in these patients depends on the dose ingested and how long after ingestion the blood is obtained. Thyroid extract ingestion may be associated with elevations of both T4 and/or T3, depending on the preparation used and the time interval since ingestion.
TOXIC MULTINODULAR GOITER
Toxic multinodular goiters that cause thyrotoxicosis are usually very large. Patients with thyrotoxicosis that is due to a multinodular gland do not undergo spontaneous exacerbations and remissions, and definitive therapy (131I or surgery) is usually required. Thyroid scans show diffuse inhomogeneous tracer uptake, reflecting areas of hyperfunction and hypofunction within the gland. Occasionally, CT or MRI of the neck may be helpful in delineating the size of a thyroid gland and in assessing impingement on surrounding structures (see Fig. 42-6). As stated in Chapter 37, the iodine contained in radiocontrast agents used with CT scans may cause thyroid dysfunction. On physical examination, the thyroid glands are multinodular and enlarged. The nodules usually are benign follicular adenomas. Toxic nodular goiters occur equally in men and women and can appear at any age, although they most frequently occur in patients older than 40 years. Usually, there is no exophthalmos, acropachy, onycholysis, or pretibial myxedema. Toxic nodular goiters are not believed to have an autoimmune etiology, because serum TSH receptor antibodies are absent. Antibodies that stimulate thyroid growth may be important in these disorders,45 but this finding is controversial. Low-titer antithyroglobulin or antimicrosomal antibodies may be present. Occasionally, eye findings may also be present. This presentation of stigmata of Graves disease with a nodular rather than diffuse goiter has been termed the Marine-Lenhart syndrome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree