Dietary Factors
Karin B. Michels
Walter C. Willett
INTRODUCTION
Over two decades ago, Doll and Peto1 speculated that 35% (range: 10% to 70%) of all cancer deaths in the United States may be preventable by alterations in diet. The magnitude of the estimate for dietary factors exceeded that for tobacco (30%) and infections (10%).
Studies of cancer incidence among populations migrating to countries with different lifestyle factors have indicated that most cancers have a large environmental etiology. Although the contribution of environmental influences differs by cancer type, the incidence of many cancers changes by as much as five- to tenfold among migrants over time, approaching that of the host country. The age at migration affects the degree of adaptation among first-generation migrants for some cancers, suggesting that the susceptibility to environmental carcinogenic influences varies with age by cancer type. Identifying the specific environmental and lifestyle factors most important to cancer etiology, however, has proven difficult.
Environmental factors such as diet may influence the incidence of cancer through many different mechanisms and at different stages in the cancer process. Simple mutagens in foods, such as those produced by the heating of proteins, can cause damage to DNA, but dietary factors can also influence this process by inducing enzymes that activate or inactivate these mutagens, or by blocking the action of the mutagen. Dietary factors can also affect every pathway hypothesized to mediate cancer risk-for example, the rate of cell cycling through hormonal or antihormonal effects, aiding or inhibiting DNA repair, promoting or inhibiting apoptosis, and DNA methylation. Because of the complexity of these mechanisms, knowledge of dietary influences on risk of cancer will require an empirical basis with human cancer as the outcome.
METHODOLOGIC CHALLENGES
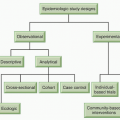
Study Types and Biases
The association between diet and the risk of cancer has been the subject of a number of epidemiologic studies. The most prevalent designs are the case-control study, the cohort study, and the randomized clinical trial. When the results from epidemiologic studies are interpreted, the potential for confounding must be considered. Individuals who maintain a healthy diet are likely to exhibit other indicators of a healthy lifestyle, including regular physical activity, lower body weight, use of multivitamin supplements, lower smoking rates, and lower alcohol consumption. Even if the influence of these confounding variables is analytically controlled, residual confounding remains possible.
Ecologic Studies
In ecologic studies or international correlation studies, variation in food disappearance data and the prevalence of a certain disease are correlated, generally across different countries. A linear association may provide preliminary data to inform future research but, due to the high probability of confounding, cannot provide strong evidence for a causal link. Food disappearance data also may not provide a good estimate for human consumption. The gross national product is correlated with many dietary factors such as fat intake.2 Many other differences besides dietary fat exist between the countries with low fat consumption (less affluent) and high fat consumption (more affluent); reproductive behaviors, physical activity level, and body fatness are particularly notable and are strongly associated with specific cancers.
Migrant Studies
Studies of populations migrating from areas with low incidence of disease to areas with high incidence of disease (or vice versa) can help sort out the role of environmental factors versus genetics in the etiology of a cancer, depending on whether the migrating group adopts the cancer rates of the new environment. Specific dietary components linked to disease are difficult to identify in a migrant study.
Case-Control Studies
Case-control studies of diet may be affected by recall bias, control selection bias, and confounding. In a case-control study, participants affected by the disease under study (cases) and healthy controls are asked to recall their past dietary habits. Cases may overestimate their consumption of foods that are commonly considered “unhealthy” and underestimate their consumption of foods considered “healthy.” Giovannucci et al.3 have documented differential reporting of fat intake before and after disease occurrence. Thus, the possibility of recall bias in a case-control study poses a real threat to the validity of the observed associations. Even more importantly, in contemporary case-control studies using a population sample of controls, the participation rate of controls is usually far from complete, often 50% to 70%. Unfortunately, health-conscious individuals may be more likely to participate as controls and will thus be less overweight, will consume fruits and vegetables more frequently, and will consume less fat and red meat, which can substantially distort associations observed.
Cohort Studies
Prospective cohort studies of the effects of diet are likely to have a much higher validity than retrospective case-control studies because diet is recorded by participants before disease occurrence. Cohort studies are still affected by measurement error because diet consists of a large number of foods eaten in complex combinations. Confounding by other unmeasured or imperfectly measured lifestyle factors can remain a problem in cohort studies.
Now that the results of a substantial number of cohort studies have become available, their findings can be compared with those of case-control studies that have examined the same relations. In
many cases, the findings of the case-control studies have not been confirmed; for example, the consistent finding of lower risk of many cancers with higher intake of fruits and vegetables in case-control studies has generally not been seen in cohort studies.4 These findings suggest that the concerns about biases in case-control studies of diet, and probably many other lifestyle factors, are justified, and findings from such studies must be interpreted cautiously.
many cases, the findings of the case-control studies have not been confirmed; for example, the consistent finding of lower risk of many cancers with higher intake of fruits and vegetables in case-control studies has generally not been seen in cohort studies.4 These findings suggest that the concerns about biases in case-control studies of diet, and probably many other lifestyle factors, are justified, and findings from such studies must be interpreted cautiously.
Randomized Clinical Trials
The gold standard in medical research is the randomized clinical trial (RCT). In an RCT on nutrition, participants are randomly assigned to one of two or more diets; hence, the association between diet and the cancer of interest should not be confounded by other factors. The problem with RCTs of diet is that maintaining the assigned diet strictly over many years, as would be necessary for diet to have an impact on cancer incidence, is difficult. For example, in the dietary fat reduction trial of the Women’s Health Initiative (WHI), participants randomized to the intervention arm reduced their fat intake much less than planned.5 The remaining limited contrast between the two groups left the lack of difference in disease outcomes difficult to interpret. Furthermore, the relevant time window for intervention and the necessary duration of intervention are unclear, especially with cancer outcomes. Hence, randomized trials are rarely used to examine the effect of diet on cancer but have better promise for the study of diet and outcomes that require a considerably shorter follow-up time (e.g., adenoma recurrence). Also, the randomized design may lend itself better to the study of the effects of dietary supplements such as multivitamin or fiber supplements, although the control group may adopt the intervention behavior because nutritional supplements are widely available. For example, in the WHI trial of calcium and vitamin D supplementation, two-thirds of the study population used vitamin D or calcium supplements that they obtained outside of the trial, again rendering the lack of effect in the trial uninterpretable.
Diet Assessment Instruments
Observational studies depend on a reasonably valid assessment of dietary intake. Although, for some nutrients, biochemical measurements can be used to assess intake, for most dietary constituents, a useful biochemical indicator does not exist. In population-based studies, diet is generally assessed with a self-administered instrument. Since 1980, considerable effort has been directed at the development of standardized questionnaires for measuring diet, and numerous studies have been conducted to assess the validity of these methods. The most widely used diet assessment instruments are the food frequency questionnaire, the 7-day diet record, and the 24-hour recall. Although the 7-day diet record may provide the most accurate documentation of intake during the week the participant keeps a diet diary, the burden of computerizing the information and extracting foods and nutrients has prohibited the use of the 7-day diet record in most large-scale studies. The 24-hour recall provides only a snapshot of diet on one day, which may or may not be representative of the participant’s usual diet and is thus affected by both personal variation and seasonal variation. The food frequency questionnaire, the most widely used instrument in large population-based studies, asks participants to report their average intake of a large number of foods during the previous year. Participants tend to substantially overreport their fruit and vegetable consumption on the food frequency questionnaire.6 This tendency may reflect social desirability bias, which leads to overreporting healthy foods and underreporting less healthy foods. Studies of validity using biomarkers or detailed measurements of diet as comparisons have suggested that carefully designed questionnaires can have sufficient validity to detect moderate to strong associations. Validity can be enhanced by using the average of repeated assessments over time.7
THE ROLE OF INDIVIDUAL FOOD AND NUTRIENTS IN CANCER ETIOLOGY
Energy
The most important impact of diet on the risk of cancer is mediated through body weight. Overweight, obesity, and inactivity are major contributors to cancer risk. (A more detailed discussion is provided in Chapter 10.) In the large American Cancer Society Cohort, obese individuals had substantially higher mortality from all cancers and, in particular, from colorectal cancer, postmenopausal breast cancer, uterine cancer, cervical cancer, pancreatic cancer, and gallbladder cancer than their normal-weight counterparts.8 Adiposity and, in particular, waist circumference are predictors of colon cancer incidence among women and men.9,10 A weight gain of 10 kg or more is associated with a significant increase in postmenopausal breast cancer incidence among women who never used hormone replacement therapy, whereas a weight loss of comparable magnitude after menopause substantially decreases breast cancer risk.11 Regular physical activity contributes to a lower prevalence of being overweight and obesity and consequently reduces the burden of cancer through this pathway.
The mechanisms whereby adiposity increases the risk of various cancers are probably multiple. Being overweight is strongly associated with endogenous estrogen levels, which likely contribute to the excess risks of endometrial and postmenopausal breast cancers. The reasons for the association with other cancers are less clear, but excess body fat is also related to higher circulating levels of insulin, insulin-like growth factor (IGF)-1, and C-peptide (a marker of insulin secretion), lower levels of binding proteins for sex hormones and IGF-1, and higher levels of various inflammatory factors, all of which have been hypothesized to be related to risks of various cancers.
Energy restriction is one of the most effective measures to prevent cancer in the animal model. While energy restriction is more difficult to study in humans, voluntary starvation among anorectics and situations of food rationing during famines provide related models. Breast cancer rates were substantially reduced among women with a history of severe anorexia.12 Although breast cancer incidence was higher among women exposed to the Dutch famine during childhood or adolescence, such short-term involuntary food rationing for 9 months or less was often followed by overnutrition.13 A more prolonged deficit in food availability during World War II in Norway was associated with a reduction in adult risk of breast cancer if it occurred during early adolescence.14
Alcohol
Aside from body weight, alcohol consumption is the best established dietary risk factor for cancer. Alcohol is classified as a carcinogen by the International Agency for Research on Cancer. The consumption of alcohol increases the risk of numerous cancers, including those of the liver, esophagus, pharynx, oral cavity, larynx, breast, and colorectum in a dose-dependent fashion.15 Evidence is convincing that excessive alcohol consumption increases the risk of primary liver cancer, probably through cirrhosis and alcoholic hepatitis. At least in the developed world, about 75% of cancers of the esophagus, pharynx, oral cavity, and larynx are attributable to alcohol and tobacco, with a marked increase in risk among drinkers who also smoke, suggesting a multiplicative effect. Mechanisms may include direct damage to the cells in the upper gastrointestinal tract; modulation of DNA methylation, which affects susceptibility to DNA mutations; and an increase in acetaldehyde, the main metabolite of alcohol, which enhances the proliferation of epithelial cells, forms DNA adducts, and is a recognized carcinogen. The association between alcohol consumption and breast cancer is notable because a small but significant risk has been found even
with one drink per day. Mechanisms may include an interaction with folate, an increase in endogenous estrogen levels, and an elevation of acetaldehyde. Some evidence suggests that the excess risk is mitigated by adequate folate intake possibly through an effect on DNA methylation.16 Notably, for most cancer sites, no important difference in associations was found with the type of alcoholic beverage, suggesting a critical role of ethanol in carcinogenesis.
with one drink per day. Mechanisms may include an interaction with folate, an increase in endogenous estrogen levels, and an elevation of acetaldehyde. Some evidence suggests that the excess risk is mitigated by adequate folate intake possibly through an effect on DNA methylation.16 Notably, for most cancer sites, no important difference in associations was found with the type of alcoholic beverage, suggesting a critical role of ethanol in carcinogenesis.
Dietary Fat
In recent years, reducing dietary fat has been at the center of cancer prevention efforts. In the landmark 1982 National Academy of Sciences review of diet, nutrition, and cancer, a reduction in fat intake to 30% of calories was the primary recommendation.
Interest in dietary fat as a cause of cancer began in the first half of the 20th century, when studies by Tannenbaum17 indicated that diets high in fat could promote tumor growth in animal models. Dietary fat has a clear effect on tumor incidence in many models, although not in all; however, a central issue has been whether this is independent of the effect of energy intake. In the 1970s, the possible relation of dietary fat intake to cancer incidence gained greater attention as the large international differences in rates of many cancers were noted to be strongly correlated with apparent per capita fat consumption in ecologic studies.2 Particularly strong associations were seen with cancers of the breast, colon, prostate, and endometrium, which include the most important cancers not due to smoking in affluent countries. These correlations were observed to be limited to animal, not vegetable, fat.
Dietary Fat and Breast Cancer
Breast cancer is the most common malignancy among women, and incidence has been increasing for decades, although a decline has been noted starting with the new millennium. Rates in most parts of Asia, South America, and Africa have been only approximately one-fifth that of the United States, but in almost all these areas rates of breast cancer are also increasing. Populations that migrate from low- to high-incidence countries develop breast cancer rates that approximate those of the new host country. However, rates do not approach those of the general US population until the second or third generation.18 This slower rate of change for immigrants may indicate delayed acculturation; although because a similar delay in rate increase is not observed for colon cancer, it may suggest an origin of breast cancer earlier in the life course.
The results from 12 smaller case-control studies that included 4,312 cases and 5,978 controls have been summarized in a metaanalysis.19 The pooled relative risk (RR) was 1.35 (P <.0001) for a 100-g increase in daily total fat intake, although the risk was somewhat stronger for postmenopausal women (RR, 1.48; P <.001). This magnitude of association, however, could be compatible with biases due to recall of diet or the selection of controls.
Because of the prospective design of cohort studies, most of the methodologic biases of case-control studies are avoided. In an analysis of the Nurses’ Health Study that included 121,700 US female registered nurses, no association with total fat intake was observed, and there was no suggestion of any reduction in risk at intakes below 25% of energy.20 Because repeated assessments of diet were obtained at 2- to 4-year intervals, this analysis provided a particularly detailed evaluation of fat intake over an extended period in relation to breast cancer risk. Similar observations were made in the National Institutes of Health (NIH)-American Association of Retired Persons (AARP) Diet and Health Study including 188,736 postmenopausal women21 and in the European Prospective Investigation into Cancer and Nutrition (EPIC), which included 7,119 incident cases.22 In a pooled analysis of seven prospective studies, which included 337,000 women who developed 4,980 incident cases of breast cancer, no overall association was seen for fat intake over the range of less than 20% to more than 45% energy (reflecting the current range observed internationally).23 A similar lack of association was seen for specific types of fat. This lack of association with total fat intake was confirmed in a subsequent analysis of the pooled prospective studies of diet and breast cancer, which included over 7,000 cases.24 Therefore, these cohort findings do not support the hypothesis that dietary fat is an important contributor to breast cancer incidence.
Endogenous estrogen levels have now been established as a risk factor for breast cancer. Thus, the effects of fat and other dietary factors on estrogen levels are of potential interest. Vegetarian women, who consume higher amounts of fiber and lower amounts of fat, have lower blood levels and reduced urinary excretion of estrogens, apparently due to increased fecal excretion. A metaanalysis has suggested that a reduction in dietary fat reduces plasma estrogen levels,25 but the studies included were plagued by the lack of concurrent controls, the short duration, and the negative energy balance. In a large, randomized trial among postmenopausal women with a previous diagnosis of breast cancer, a reduction in dietary fat did not affect estradiol levels when the data were appropriately analyzed.26
The WHI Randomized Controlled Dietary Modification Trial similarly suggested no association between fat intake and breast cancer incidence,5 but these results are difficult to interpret.27 The data on biomarkers that reflect fat intake suggest little if any difference in fat intake between the intervention and control groups.28 Even if dietary fat does truly have an effect on cancer incidence and other outcomes, this lack of adherence to the dietary intervention could explain the absence of an observed effect on total cancer incidence and total mortality. In another randomized trial in Canada that tested an intervention target of 15% of calories from fat, a small but significant difference in high-density lipoprotein (HDL) levels was observed after 8 to 9 years of follow-up suggesting a difference in fat intake in the two groups.29 The incidence of breast cancer in the intervention and the control group did not differ significantly.
Some prospective cohort studies suggest an inverse association between monounsaturated fat and breast cancer. This is an intriguing observation because of the relatively low rates of breast cancer in southern European countries with high intakes of monounsaturated fats due to the use of olive oil as the primary fat. In case-control studies in Spain, Greece, and Italy, women who used more olive oil had reduced risks of breast cancer.
In a report of findings from the Nurses’ Health Study II cohort of premenopausal women, a higher intake of animal fat was associated with an approximately 50% greater risk of breast cancer, but no association was seen with intake of vegetable fat.30 This suggests that factors in foods containing animal fats, rather than fat per se, may account for the findings. In the same cohort, an intake of red meat and total fat during adolescence was also associated with the risk of premenopausal breast cancer.31,32
Dietary Fat and Colon Cancer
In comparisons among countries, rates of colon cancer are strongly correlated with a national per capita disappearance of animal fat and meat, with correlation coefficients ranging between 0.8 and 0.9.2 Rates of colon cancer rose sharply in Japan after World War II, paralleling a 2.5-fold increase in fat intake. Based on these epidemiologic investigations and on animal studies, a hypothesis has developed that higher dietary fat increases the excretion of bile acids, which can be converted to carcinogens or act as promoters. However, evidence from many studies on obesity and low levels of physical activity increasing the risk of colon cancer suggests that at least part of the high rates in affluent countries previously attributed to fat intake is probably due to a sedentary lifestyle.
The Nurses’ Health Study suggested an approximately twofold higher risk of colon cancer among women in the highest quintile of animal fat intake than in those in the lowest quintile.33 In a multivariate analysis of these data, which included red meat intake and animal fat intake in the same model, red meat intake
remained significantly predictive of colon cancer risk, whereas the association with animal fat was eliminated. Other cohort studies have supported associations of colon cancer and the consumption of red meat and processed meats but not other sources of fat or total fat.34,35,36 Similar associations were also observed for colorectal adenomas. In a meta-analysis of prospective studies, red meat consumption was associated with a risk of colon cancer (RR = 1.24; 95% confidence interval [CI], 1.09 to 1.41 for an increment of 120 g per day).37 The association with the consumption of processed meats was particularly strong (RR = 1.36; 95% CI, 1.15 to 1.61 for an increment of 30 g per day).
remained significantly predictive of colon cancer risk, whereas the association with animal fat was eliminated. Other cohort studies have supported associations of colon cancer and the consumption of red meat and processed meats but not other sources of fat or total fat.34,35,36 Similar associations were also observed for colorectal adenomas. In a meta-analysis of prospective studies, red meat consumption was associated with a risk of colon cancer (RR = 1.24; 95% confidence interval [CI], 1.09 to 1.41 for an increment of 120 g per day).37 The association with the consumption of processed meats was particularly strong (RR = 1.36; 95% CI, 1.15 to 1.61 for an increment of 30 g per day).
The apparently stronger association with red meat consumption than with fat intake in most large cohort studies needs further confirmation, but such an association could result if the fatty acids or nonfat components of meat (e.g., the heme iron or carcinogens created by cooking) were the primary etiologic factors. This issue has major practical implications because current dietary recommendations support the daily consumption of red meat as long as it is lean.38
Dietary Fat and Prostate Cancer
Although further data are desirable, the evidence from international correlations, case-control39 and cohort studies40,41,42,43,44 provides some support for an association between the consumption of fat-containing animal products and prostate cancer incidence. This evidence does not generally support a relation with intake of vegetable fat, which suggests that either the type of fat or other components of animal products are responsible. Some evidence also indicates that animal fat consumption may be most strongly associated with the incidence of aggressive prostate cancer, which suggests an influence on the transition from the widespread indolent form to the more lethal form of this malignancy. Data are limited on the relation of fat intake to the probability of survival after the diagnosis of prostate cancer.
Dietary Fat and Other Cancers
Rates of other cancers that are common in affluent countries, including those of the endometrium and ovary, are also correlated with fat intake internationally. In prospective studies between Iowa and Canadian women, no evidence of a relation between fat intake and risk of endometrial cancer was found. Positive associations between dietary fat and lung cancer have been observed in many case-control studies. However, in a pooled analysis of large prospective studies that included over 3,000 incident cases, no association was observed.45 These findings provide further evidence that the results of case-control studies of diet and cancer are likely to be misleading.
Summary
Largely on the basis of the results of animal studies, international correlations, and a few case-control studies, great enthusiasm developed in the 1980s that modest reductions in total fat intake would have a major impact on breast cancer incidence. As the findings from large prospective studies have become available, however, support for this relation has greatly weakened. Although evidence suggests that a high intake of animal fat early in adult life may increase the risk of premenopausal breast cancer, this is not likely to be due to fat per se because vegetable fat intake was not related to risk. For colon cancer, the associations seen with animal fat intake internationally have been supported in numerous case-control and cohort studies, but this also appears to be explained by factors in red meat other than simply its fat content. Further, the importance of physical activity and leanness as protective factors against colon cancer indicates that international correlations probably overstate the contribution of diet to differences in colon cancer incidence. At present, the available evidence most strongly suggests an association between animal fat consumption and risk of prostate cancer, particularly the aggressive form of this disease. As with colon cancer, the possibility remains that other factors in animal products contribute to risk.
Despite the large body of data on dietary fat and cancer that has accumulated since 1985, any conclusions should be regarded as tentative, because these are disease processes that are poorly understood and are likely to take many decades to develop. Because most of the reported literature from prospective studies is based on fewer than 20 years’ follow-up, further evaluations of the effects of diet earlier in life and at longer intervals of observation are needed to fully understand these complex relations. Nevertheless, persons interested in reducing their risk of cancer could be advised, as a prudent measure, to minimize their intake of foods high in animal fat, particularly red meat. Such a dietary pattern is also likely to be beneficial for the risk of cardiovascular disease. On the other hand, unsaturated fats (with the exception of transfatty acids) reduce blood low-density lipoprotein cholesterol levels and the risk of cardiovascular disease, and little evidence suggests that they adversely affect cancer risk. Thus, efforts to reduce unsaturated fat intake are not warranted at this time and are likely to have adverse effects on cardiovascular disease risk. Because excess adiposity increases the risk of several cancers and cardiovascular disease, balancing calories from any source with adequate physical activity is extremely important.
Fruits and Vegetables
General Properties
Fruits and vegetables have been hypothesized to be major dietary contributors to cancer prevention because they are rich in potential anticarcinogenic substances. Fruits and vegetables contain antioxidants and minerals and are good sources of fiber, potassium, carotenoids, vitamin C, folate, and other vitamins. Although fruits and vegetables supply less than 5% of total energy intake in most countries worldwide on a population basis, the concentration of micronutrients in these foods is greater than in most others.
The comprehensive report of the World Cancer Research Fund and the American Institute for Cancer Research, published in 2007 and titled Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective, reached the consensus based on the available evidence: “findings from cohort studies conducted since the mid-1990s have made the overall evidence, that vegetables or fruits protect against cancers, somewhat less impressive. In no case now is the evidence of protection judged to be convincing.”15
Fruit and Vegetable Consumption and Colorectal Cancer
The association between fruit and vegetable consumption and the incidence of colon or rectal cancer has been examined prospectively in at least six studies. In some of these prospective cohorts, inverse associations were observed for individual foods or particular subgroups of fruits or vegetables, but no consistent pattern emerged and many comparisons revealed no such links. The results from the largest studies, the Nurses’ Health Study and the Health Professionals’ Follow-Up Study, suggested no important association between the consumption of fruits and vegetables and the incidence of cancers of the colon or rectum during 1,743,645 person-years of follow-up.46 In these two large cohorts, diet was assessed repeatedly during follow-up with a detailed food frequency questionnaire. Similarly, in the Pooling Project of Prospective Studies of Diet and Cancer, including 14 studies, 756,217 participants, and 5,838 cases of colon cancer, no association with overall colon cancer risk was found.47
Fruit and Vegetable Consumption and Stomach Cancer
At least 12 prospective cohort studies have examined the consumption of some fruits and vegetables and the incidence of stomach
cancer.15 Seven of these studies considered total vegetable intake. Three found significant protection from stomach cancer, whereas three did not. All other comparisons were made for subgroups of vegetables and produced inconsistent results. Nine prospective cohort studies investigated the association between fruit consumption and stomach cancer risk. Four studies found an inverse association of borderline statistical significance.
cancer.15 Seven of these studies considered total vegetable intake. Three found significant protection from stomach cancer, whereas three did not. All other comparisons were made for subgroups of vegetables and produced inconsistent results. Nine prospective cohort studies investigated the association between fruit consumption and stomach cancer risk. Four studies found an inverse association of borderline statistical significance.
Fruit and Vegetable Consumption and Breast Cancer
The most comprehensive evaluation of fruit and vegetable consumption and the incidence of breast cancer was provided by a pooled analysis of all cohort studies.48 Data were pooled from eight prospective studies that included 351,825 women, 7,377 of whom developed incident invasive breast cancer during follow-up. The pooled relative risk adjusted for potential confounding variables was 0.93 (95% CI, 0.86 to 1.0; P for trend, .08) for the highest versus the lowest quartile of fruit consumption, 0.96 (95% CI, 0.89 to 1.04; P for trend, .54) for vegetable intake, and 0.93 (95% CI, 0.86 to 1.0; P for trend, .12) for total consumption of fruits and vegetables combined. The EPIC study confirmed this lack of association.49 In a recent analysis within the Nurses’ Health Study, an inverse association was seen between vegetable intake and the risk of estrogen receptor-negative breast cancer.50 This observation was confirmed in the pooling project of prospective studies: The pooled relative risk for the highest vs. the lowest quintile of total vegetable consumption was 0.82 (95% CI 0.74 to 0.90) for estrogen-receptor negative breast cancer.51
Fruit and Vegetable Consumption and Lung Cancer
The relation between fruit and vegetable consumption and the incidence of lung cancer was examined in the pooled analysis of cohort studies.52 Overall, no association was observed, although a modest increase in lung cancer incidence was evident among participants with the lowest fruit and vegetable consumption.
Fruit and Vegetable Consumption and Total Cancer
An analysis of the Nurses’ Health Study and the Health Professionals’ Follow-Up Study, including over 9,000 incident cases of cancer, did not reveal a benefit of fruit and vegetable consumption for total cancer incidence.53 Observations from the EPIC cohort were essentially consistent with these findings.54 Although there may be no or only a very weak protection conferred for cancer from consuming an abundance of fruits and vegetables, there is a substantial benefit for protection from cardiovascular disease.
Summary
The consumption of fruits and vegetables and some of their main micronutrients appear to be less important in cancer prevention than previously assumed. With an accumulation of data from prospective cohort studies and randomized trials, a lack of association of these foods and nutrients with cancer outcomes has become apparent. A modest association cannot be excluded because of an imperfect measurement of diet, and it remains possible that a high consumption of fruits and vegetables during childhood and adolescence is more effective at reducing cancer risk than consumption in adult life due to the long latency of cancer manifestation.
Conversely, it is possible that, with the fortification of breakfast cereal, flour, and other staple foods, the frequent consumption of fruits and vegetables has become less essential for cancer prevention. Nevertheless, an abundance of fruits and vegetables as part of a healthy diet is recommended, because evidence consistently suggests that it lowers the incidence of hypertension, heart disease, and stroke.
Fiber
General Properties
Dietary fiber was defined in 1976 as “all plant polysaccharides and lignin which are resistant to hydrolysis by the digestive enzymes of men.”55 Fiber, both soluble and insoluble, is fermented by the luminal bacteria of the colon. Among the properties of fiber that make it a candidate for cancer prevention are its “bulking” effect, which reduces colonic transit time, and the binding of potentially carcinogenic luminal chemicals. Fiber may also aid in producing short-chain fatty acids that may be directly anticarcinogenic. Fiber may also induce apoptosis.
Dietary Fiber and Colorectal Cancer
In 1969, Dennis Burkitt hypothesized that dietary fiber is involved in colon carcinogenesis.56 While working as a physician in Africa, Burkitt noticed the low incidence of colon cancer among African populations whose diets were high in fiber. Burkitt concluded that a link might exist between the fiber-rich diet and the low incidence of colon cancer. Burkitt’s observations were followed by numerous case-control studies that seemed to confirm his theories. A combined analysis of 13 case-control studies57 as well as a meta-analysis of 16 case-control studies58 suggested an inverse association between fiber intake and the risk of colorectal cancer. The inclusion of studies was selective, however, and effect estimates unadjusted for potential confounders were used for most studies. Moreover, recall bias is a severe threat to the validity of retrospective case-control studies of fiber intake and any disease outcome.
Data from prospective cohort studies have largely failed to support an inverse association between dietary fiber and colorectal cancer incidence. Initial analyses from the Nurses’ Health Study and the Health Professionals’ Follow-Up Study36 found no important association between dietary fiber and colorectal cancer. A significant inverse association between fiber intake and incidence of colorectal cancer was reported from the EPIC study. The analysis presented on dietary fiber and colorectal cancer encompassed 434,209 women and men from eight European countries.59 The analytic model used by the EPIC investigators included adjustments for age, height, weight, total caloric intake, sex, and center assessed at baseline and identified60 a significant inverse association between fiber intake and colorectal cancer. Applying the same analytic model used in EPIC to data from the Nurses’ Health Study and the Health Professionals’ Follow-Up Study encompassing 1.8 million person-years of follow-up and 1,572 cases of colorectal cancer revealed associations similar to those found in the EPIC study.61 After a more complete adjustment for confounding variables, however, the association vanished.61 Results from the pooled analysis of 13 prospective cohort studies, including 8,081 colorectal cancer cases diagnosed during over 7 million person-years of follow-up, suggested an inverse relation between dietary fiber and colorectal cancer incidence in age-adjusted analyses, but this association disappeared after appropriate adjustment for confounding variables, particularly other dietary factors.62 The NIH-AARP study, which included 2,974 cases of colorectal cancer, confirmed the lack of association between total dietary fiber and colorectal cancer risk.63
The association between dietary fiber and colorectal cancer appears to be confounded by a number of other dietary and non-dietary factors. These methodologic considerations must be taken into account when interpreting the evidence. It is possible that other dietary factors such as folate intake are more important for colorectal cancer pathogenesis than dietary fiber.
Dietary Fiber and Colorectal Adenomas
In a few prospective cohort studies, the primary occurrence of colorectal polyps was investigated, but no consistent relation was found.
The study of fiber intake and colorectal adenoma recurrence lends itself to a randomized clinical trial design because of the relatively short follow-up necessary and because fiber can be provided as a supplement. A number of RCTs have explored the effect of fiber supplementation on colorectal adenoma recurrence. Evidence has fairly consistently indicated no effect of fiber intake.64,65,66,67,68 In one RCT, an increase in adenoma recurrence was observed among participants randomly assigned to use a fiber supplement, which was stronger among those with high dietary calcium.69
Dietary Fiber and Breast Cancer
Investigators have speculated that dietary fiber may reduce the risk of breast cancer through a reduction in intestinal absorption of estrogens excreted via the biliary system.
Relatively few epidemiologic studies have examined the association between fiber intake and breast cancer. In a meta-analysis of 10 case-control studies, a significant inverse association was observed. However, these retrospective studies were likely affected by the aforementioned biases—selection and recall bias, in particular. Results from at least six prospective cohort studies consistently suggested no association between fiber intake and breast cancer incidence.70,71,72,73,74,75
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree